 |
 |
- Search
| Korean J Fam Med > Volume 41(3); 2020 > Article |
|
Abstract
Chronic constipation (CC) is a common disorder in the elderly population globally and is associated with comorbidities and negative implications on the quality of life. Constipation prevalence varies in different studies, primarily owing to the nonuniformity of the diagnostic criteria. However, 15%–30% of individuals aged >60 years are diagnosed with CC. Primary care physicians are the main healthcare providers that manage constipation in elderly patients in parallel with increased population aging and increased prevalence of constipation. Physical inactivity, polypharmacy, chronic medical conditions, rectal hyposensitivity, and defecatory disorders all play a role in the pathogenesis of CC in elderly patients. Detailed anamnesis, particularly history related to chronic medication use, with digital rectal examination may assist in identifying constipation causes. Additionally, blood tests and colonoscopy may identify organic causes of CC. Physiologic tests (i.e., anorectal manometry, colonic transit time with radiopaque markers, and defecography) can evaluate the physiologic function of the colon, rectum, and anus. However, generally, there are several causes of constipation in older patients, and an individualized approach is recommended. Treatment of chronic idiopathic constipation is empiric, based on the stepwise approach. Lifestyle advice, adjustment of chronic medications, and prescription of laxatives are the first steps of management. Several laxatives are available, and the treatment is evolving in the last decade. Biofeedback is an effective therapy especially for defecatory disorders. This review aimed to summarize the most updated knowledge for primary care physicians in the approach and management of CC in elderly patients.
The prevalence of chronic constipation (CC) increases with age in both sexes, particularly above the age of 60 years [1]. In two related global surveys, the prevalence of self-defined constipation in Asian adults (from South Korea, China, and Indonesia) was estimated to be 15%–23% in women and approximately 11% in men [2,3]. CC leads to major impairments in the quality of life and is an economic burden to the patient and national health services. The definition of CC between patients and physicians and among different physicians lacks uniformity; thus, the reported prevalence is diverse in different epidemiological studies [1,4]. An international expert committee congregated in 2016 in Rome to update the definition of CC (Rome IV criteria) (Table 1) [5].
The most prevalent complaints in elderly patients with constipation are as follows: need to apply prolonged abdominal pressure during defecation, sensation of outlet obstruction at the level of the anus, and digitalization to relieve impacted stool [6]. The main risk factors for constipation in the elderly population include the following: immobility, weakness of the abdominal and pelvic floor muscles, malnutrition, rectal hyposensitivity, ignoring a “defecation call,” chronic medical conditions (metabolic, neurologic, cardiovascular), chronic medication use (analgesics, calcium channel blockers, antihypertensive drugs, and antipsychotics), and aging effects on colonic motility (Tables 2, 3) [7,8]. Additionally, psychological, social, and behavioral factors may contribute to the development of CC in the elderly population [4]. CC may lead to serious anorectal complications, including anal pain, anal fissures, hemorrhoids, rectal bleeding, and fecal impaction, a stern condition that may cause restlessness, anxiety, rectal ulcers, and perforation in extremely rare cases [8].
It is a type of constipation in the elderly population and characterized by infrequent bowel movements and slow movement of stool through the colon. Patients with slow transit constipation often have reduced frequency of high-amplitude propagated contractions (the physiological function of moving contents through the colon) after meals. Bloating, abdominal pain, and an infrequent urge to defecate are commonly associated with this condition clinically. Histopathological studies have shown several processes such as myopathic and degenerative alterations in the colonic smooth muscle cells and collagen depositions in the right colon to lead to colonic hypomotility in elderly patients with constipation [9].
Normal transit constipation is characterized by a normal rate of stool movement through the colon, but the patient feels constipated. This is usually secondary to perceived difficulty with defecation and hard stools. Patients often complain of bloating and abdominal pain. At other times, these patients present with abdominal pain, which is relieved by defecation, and therefore the symptoms may overlap those of constipation-predominant irritable bowel syndrome (IBS).
Defecatory disorders are most commonly due to functional paradoxical contraction of the pelvic floor, abdominal muscles, and anal sphincter (dyssenergia or anismus) and are the type of constipation in the elderly population [8]. Patients typically report an inability to defecate, despite feeling an urge to do so. They frequently use digital manipulation or need to adopt a specific position on the toilet to pass stool [10]. Secondary causes of defecatory disorders include structural abnormalities, such as a rectocele (bulging of the rectum into the posterior wall of the vagina), rectal intussusception (telescoping of the rectum into itself during straining), perianal descent (downward movement of the perineum during straining), and other anatomical causes [11].
The primary aim of evaluation is to rule out secondary or organic cause of constipation that may be treated differently depending on the specific pathology. A detailed medical history with a focus on alarm signs (i.e., rectal bleeding, weight loss, personnel or family history of colon cancer, new iron deficiency anemia, and changes in bowel habits) (Table 4), chronic medical condition use, medication history, and social history is the first important step in managing an elderly patient with constipation. Examination of the perianal area for suggestive findings of CC, such as scars, fistulas, anal fissures, skin erythema or excoriation (may be a sign of fecal leakage), and external hemorrhoid, is an important initial part of the evaluation. Rectal examination is essential in identifying internal hemorrhoids, rectal prolapse, rectocele, fecal impaction, anal stricture, and rectal masses and aids in the diagnosis of functional defecatory disorders [12]. Blood tests, including blood count, blood glucose level, liver and kidney function tests, electrolyte level, thyroid function tests, and inflammatory markers, are necessary to exclude a secondary cause of constipation, albeit their yield is generally low and the chance to detect an abnormality showing constipation is unlikely [13]. A Korean study aimed to determine the utility of blood tests in identifying the organic cause of constipation in patients who visited a tertiary hospital in Korea. One major finding was that the prevalence of subclinical hypothyroidism was 0.41% in elderly men and women [14]. As per the recommendations of the Asia-Pacific colorectal cancer screening guidelines, colonoscopy is necessary in the presence of alarm signs (Table 4); in Japanese, Korean, and Chinese individuals aged >45 years; and in Indian and Thai individuals aged >50 years [15]. However, the workup strategy should be individualized based on the patient’s medical conditions, cognitive state, physical performance, and preference [16].
Physiologic evaluation is rarely required in elderly patients, and conservative measure with laxative prescription is generally the most reasonable, appropriate approach. Nonetheless, patients with refractory constipation and clinical suspicion of defecatory disorders should be referred to specialized pelvic floor centers.
This is a technique that evaluates anorectal morphology and dynamics during defecation. It is used to determine whether complete emptying of the rectum is achieved and measure the anorectal angle and perianal descent. It can be used to detect other abnormalities of rectal emptying, such as intussusception, mucosal prolapse, solitary rectal ulcer, and rectocele [17,18].
It is a technique that measures colonic transit time, and is a useful, practical measure of the motor function. Transit time can be measured by performing abdominal radiography after ingestion of radiopaque markers. Retention of >20% of the markers after 120 hours is considered a pathological result and an indicator of slow transit constipation [19].
Wireless Motility Capsule (WMC) is a novel technology introduced to the clinical practice in the last decade that assesses gut motility. WMC measures intraluminal temperature, pH, and pressure in different segments of the gastrointestinal (GI) tract and can measure regional or whole GI transit times. WMC is noninvasive, safe, and well tolerated by patients. However, presently, WMC is not used as a routine clinical investigation; rather, it is a research investigation tool whose clinical utility, value, and accuracy have not yet been entirely validated [21].
Elderly patients with mild constipation benefit from changes to their diet and lifestyle [13]. Excluding patients with symptoms of dehydration, there is no evidence that increasing water intake alone increases stool frequency and softens consistency [13]. Dietary fiber increases stool bulk and frequency, and some patients with low dietary fiber intake may benefit from a moderate increase in intake to 25–30 g [22]. Dietary fibers are unlikely to have any benefit in severe constipation, especially in patients with slow transit or evacuation disorders. Dietary fibers may aggravate symptoms of abdominal bloating and flatulence; therefore, it is important to commence dietary fibers in the lowest possible dose, generally 5 g, and increase the amount gradually up to 25–30 g with adequate water intake [18]. Studies have shown that increased moderate physical activity in elderly patients is associated with improvement in mild constipation symptoms but is unlikely to have an effect in patients with severe constipation [23]. Furthermore, studies have shown that immobility in an elderly patient worsens the symptoms of constipation and is considered a risk factor for fecal impaction [23].
It is an important to advise patients to employ correct toileting routines, such as regular, unhurried defecation, responding immediately to the sensation of needing to defecate (defecation call), having appropriate assistance to access the toilet, and avoiding prolonged pushing.
Laxatives are generally required for the management of constipation in the elderly population in case of inability to achieve symptom relief through lifestyle and dietary modifications (Figure 1) [18]. The choice of drug to be prescribed should be personalized for each patient, taking into account the patient’s medical history, medications, kidney and liver function test results, and electrolyte status. In this review, we will focus on the most commonly used laxatives in daily clinical practice.
These are laxatives that apply osmotic pressure within the colon lumen, thus attracting water and electrolytes and causing increased intraluminal pressure and volume. Osmotic laxatives cause stool softening, shorten colonic transit time, and enhance colonic motility [24]. The use of insoluble sugars, such as lactulose and macrogel, has been shown to be safe and effective in elderly patients, and starting lactulose 15 g/d is a reasonable early pharmacological option in managing CC in elderly patients [25]. Another important group of osmotic laxatives are polyethylene glycol (PEG)-based formulations. PEG-based formulations were originally used for colon cleansing before colonoscopy. However, they have also been shown to be useful in fecal disimpaction in the elderly population [26-28]. PEG-based formulations are currently used in a form of powder for the management of CC starting with a daily dose of 17 g, which may be increased gradually if needed and tolerated by the patient [29,30]. These drugs are generally effective and safe for use in the elderly. Some PEG-based formulations contain sodium and potassium; it is unknown whether small quantities may lead to electrolyte disturbances in elderly patient and should be avoided [31].
Bisacodyl and sodium picosulfate are the best known and most studied stimulant laxatives. Two recent randomized clinical trials on adults, using both picosulfate and bisacodyl at an average dose of 10 mg daily, involving a total of 735 primary care patients, have been shown to relieve symptoms of constipation and improve quality of life [32,33]. Nonetheless, high-quality, randomized control trials that aimed to evaluate the efficacy and safety of stimulant laxatives in the elderly population are limited. However, based on the extensive experience with bisacodyl and sodium picosulfate and the known safety and efficacy, they may be added to osmotic laxatives in the lowest possible dose (5 mg), in ad hoc bases up to 2–3 times a week, while monitoring the clinical status of the patient and electrolyte and kidney function test results [4,34]. Despite the common use of senna, there is actually no well-designed randomized controlled trial comparing its efficacy with placebo.
Prucalopride is an enterokinetic agent that activates serotonergic receptors and leads to the release of acetylcholine and activation of the myenteric plexus, thus enhancing colonic motility [35]. Prucalopride has been shown to shorten bowel transit time, relieve constipation symptoms, and improve the quality of life mainly in women in clinical trials [35,36]. Prucalopride has been shown to be effective and safe in the Asian population in a randomized, double blinded, placebo controlled trial [37]. Prucalopride has high selectivity for the 5-hydroxytryptamine 4 receptor with extremely encouraging safety and tolerability profiles; hence, it has been approved in some countries for use in the elderly population. Prucalopride 2 mg is prescribed when other laxatives have failed to control the symptoms of constipation.
It is a secretory drug (chloride channel activator) acts locally to increase intestinal fluid secretion and improve colonic transit. It has been shown to be more effective than placebo in increasing the number of spontaneous bowel movements, decreasing straining, improving stool consistency, and relieving symptoms of CC. Lubiprostone has been shown to be effective for relief of IBS symptoms at a low dose of 8 μg and effective and safe for relief CC symptoms and opioid-induced constipation in non-oncological patients [38,39]. Lubiprostone has been shown to be safe in elderly patients; however, studies have a small number of participants [40].
Biofeedback is a training practice that aims to educate patients to relax, instead of contracting their pelvic floor muscles and abdominal muscles during straining, with the aid of visual or auditory signals to feedback patient’s performance. Currently, biofeedback therapy is useful mainly to patients with pelvic floor dyssynergia (animus). Generally, biofeedback is an effective and safe treatment with a reported success rate of 70%–80% after 1 year [41-44]. In the Asian, including Korean, population, biofeedback success rates are comparable to those in the Western population [45-48]. Nonetheless, biofeedback trials in elderly patients are limited, and the decision should be personalized for each patient based in the cognitive and physical status and level of cooperation with the therapist [34].
Surgery (colectomy with ileo-anal anastomosis) is not recommended in elderly patients due to high morbidity and mortality rates associated with major surgeries in frail elderly patients [34].
CC is a common medical condition in the elderly population and associated with distress and impairment of quality of life. The primary care physicians are the main providers that manage CC in the elderly population along with the global aging of the population. Dietary advice and lifestyle modifications are the primary interventions in the management algorithm. Osmotic laxatives are safe and efficient and should be the first-line therapy. Stimulant laxatives are added in the lowest effective dose when osmotic laxatives fail to achieve adequate relief. New drugs have been introduced to the armamentarium, such as prucalopride and lubiprostone, with promising results in adults; however, their efficacy and safety have been shown in elderly patients only in small sample studies. More randomized, controlled trials are warranted to better define the efficacy and safety of the new drugs in elderly patients.
Figure. 1.
Management algorithm in the elderly patient with chronic constipation. PEG, polyethylene glycol.
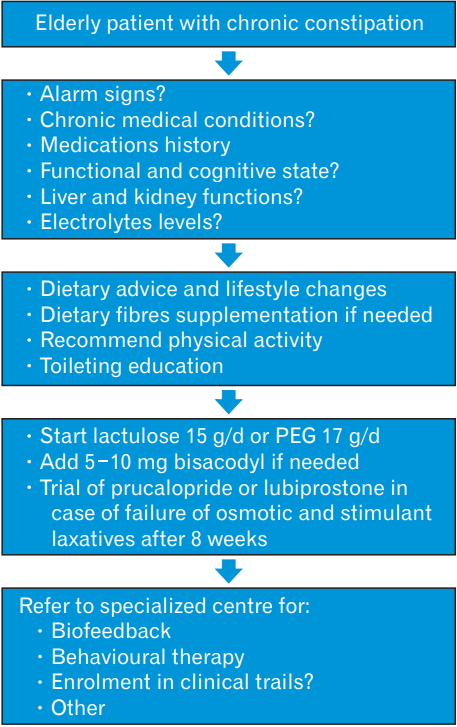
Table 1.
Rome IV criteria for primary chronic constipation
Table 2.
Risk factors of chronic constipation in elderly patients
REFERENCES
1. Pare P, Ferrazzi S, Thompson WG, Irvine EJ, Rance L. An epidemiological survey of constipation in canada: definitions, rates, demographics, and predictors of health care seeking. Am J Gastroenterol 2001;96:3130-7.


2. Wald A, Scarpignato C, Mueller-Lissner S, Kamm MA, Hinkel U, Helfrich I, et al. A multinational survey of prevalence and patterns of laxative use among adults with self-defined constipation. Aliment Pharmacol Ther 2008;28:917-30.


3. Wald A, Mueller-Lissner S, Kamm MA, Hinkel U, Richter E, Schuijt C, et al. Survey of laxative use by adults with self-defined constipation in South America and Asia: a comparison of six countries. Aliment Pharmacol Ther 2010;31:274-84.


4. Bouras EP, Tangalos EG. Chronic constipation in the elderly. Gastroenterol Clin North Am 2009;38:463-80.


5. Drossman DA, Hasler WL. Rome IV-functional GI disorders: disorders of gut-brain interaction. Gastroenterology 2016;150:1257-61.


6. Bernard CE, Gibbons SJ, Gomez-Pinilla PJ, Lurken MS, Schmalz PF, Roeder JL, et al. Effect of age on the enteric nervous system of the human colon. Neurogastroenterol Motil 2009;21:746-54.



7. Lagier E, Delvaux M, Vellas B, Fioramonti J, Bueno L, Albarede JL, et al. Influence of age on rectal tone and sensitivity to distension in healthy subjects. Neurogastroenterol Motil 1999;11:101-7.


8. Gallagher P, O’Mahony D. Constipation in old age. Best Pract Res Clin Gastroenterol 2009;23:875-87.


9. Camilleri M, Lee JS, Viramontes B, Bharucha AE, Tangalos EG. Insights into the pathophysiology and mechanisms of constipation, irritable bowel syndrome, and diverticulosis in older people. J Am Geriatr Soc 2000;48:1142-50.


10. Rao SS, Welcher KD, Leistikow JS. Obstructive defecation: a failure of rectoanal coordination. Am J Gastroenterol 1998;93:1042-50.


11. Karlbom U, Pahlman L, Nilsson S, Graf W. Relationships between defecographic findings, rectal emptying, and colonic transit time in constipated patients. Gut 1995;36:907-12.



12. Talley NJ. How to do and interpret a rectal examination in gastroenterology. Am J Gastroenterol 2008;103:820-2.


13. Gwee KA, Ghoshal UC, Gonlachanvit S, Chua AS, Myung SJ, Rajindrajith S, et al. Primary care management of chronic constipation in Asia: the ANMA chronic constipation tool. J Neurogastroenterol Motil 2013;19:149-60.




14. Kim J, Myung SJ, Yang DH, Yoon IJ, Seo SY, Ku HS, et al. Clinical characteristics of constipation with hypothyroidism. Intest Res 2010;8:48-57.


15. Sung JJ, Lau JY, Young GP, Sano Y, Chiu HM, Byeon JS, et al. Asia Pacific consensus recommendations for colorectal cancer screening. Gut 2008;57:1166-76.


16. Schuster BG, Kosar L, Kamrul R. Constipation in older adults: stepwise approach to keep things moving. Can Fam Physician 2015;61:152-8.


17. Stoker J, Bartram CI, Halligan S. Imaging of the posterior pelvic floor. Eur Radiol 2002;12:779-88.



18. Tack J, Muller-Lissner S, Stanghellini V, Boeckxstaens G, Kamm MA, Simren M, et al. Diagnosis and treatment of chronic constipation: a European perspective. Neurogastroenterol Motil 2011;23:697-710.



19. Rao SS. Constipation: evaluation and treatment of colonic and anorectal motility disorders. Gastroenterol Clin North Am 2007;36:687-711.


20. Rao SS. Constipation: evaluation and treatment of colonic and anorectal motility disorders. Gastrointest Endosc Clin N Am 2009;19:117-39.


21. Haase AM, Gregersen T, Schlageter V, Scott MS, Demierre M, Kucera P, et al. Pilot study trialling a new ambulatory method for the clinical assessment of regional gastrointestinal transit using multiple electromagnetic capsules. Neurogastroenterol Motil 2014;26:1783-91.


22. Towers AL, Burgio KL, Locher JL, Merkel IS, Safaeian M, Wald A. Constipation in the elderly: influence of dietary, psychological, and physiological factors. J Am Geriatr Soc 1994;42:701-6.


23. Bingham SA, Cummings JH. Effect of exercise and physical fitness on large intestinal function. Gastroenterology 1989;97:1389-99.


24. Spinzi G, Amato A, Imperiali G, Lenoci N, Mandelli G, Paggi S, et al. Constipation in the elderly: management strategies. Drugs Aging 2009;26:469-74.


25. Lee-Robichaud H, Thomas K, Morgan J, Nelson RL. Lactulose versus polyethylene glycol for chronic constipation. Cochrane Database Syst Rev 2010;(7):CD007570.

26. Culbert P, Gillett H, Ferguson A. Highly effective new oral therapy for faecal impaction. Br J Gen Pract 1998;48:1599-600.


27. Chen CC, Su MY, Tung SY, Chang FY, Wong JM, Geraint M. Evaluation of polyethylene glycol plus electrolytes in the treatment of severe constipation and faecal impaction in adults. Curr Med Res Opin 2005;21:1595-602.


28. Dipalma JA, Cleveland MV, McGowan J, Herrera JL. A randomized, multicenter, placebo-controlled trial of polyethylene glycol laxative for chronic treatment of chronic constipation. Am J Gastroenterol 2007;102:1436-41.


29. Paille F, Colombey N, Alleaume B, Vicari F. An open six-month study of the safety of Transipeg for treating constipation in community medicine. J Drug Assess 1999;2:97-108.
30. Chaussade S, Minic M. Comparison of efficacy and safety of two doses of two different polyethylene glycol-based laxatives in the treatment of constipation. Aliment Pharmacol Ther 2003;17:165-72.


31. Ford AC, Moayyedi P, Lacy BE, Lembo AJ, Saito YA, Schiller LR, et al. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol 2014;109 Suppl 1:S2-26.



32. Mueller-Lissner S, Kamm MA, Wald A, Hinkel U, Koehler U, Richter E, et al. Multicenter, 4-week, double-blind, randomized, placebo-controlled trial of sodium picosulfate in patients with chronic constipation. Am J Gastroenterol 2010;105:897-903.



33. Kamm MA, Mueller-Lissner S, Wald A, Richter E, Swallow R, Gessner U. Oral bisacodyl is effective and well-tolerated in patients with chronic constipation. Clin Gastroenterol Hepatol 2011;9:577-83.


34. Rao SS, Go JT. Update on the management of constipation in the elderly: new treatment options. Clin Interv Aging 2010;5:163-71.



35. Muller-Lissner S, Rykx A, Kerstens R, Vandeplassche L. A doubleblind, placebo-controlled study of prucalopride in elderly patients with chronic constipation. Neurogastroenterol Motil 2010;22:991-8.


36. Camilleri M, Piessevaux H, Yiannakou Y, Tack J, Kerstens R, Quigley EMM, et al. Efficacy and safety of prucalopride in chronic constipation: an integrated analysis of six randomized, controlled clinical trials. Dig Dis Sci 2016;61:2357-72.




37. Ke M, Zou D, Yuan Y, Li Y, Lin L, Hao J, et al. Prucalopride in the treatment of chronic constipation in patients from the Asia-Pacific region: a randomized, double-blind, placebo-controlled study. Neurogastroenterol Motil 2012;24:999-1009.



38. Chang L, Chey WD, Drossman D, Losch-Beridon T, Wang M, Lichtlen P, et al. Effects of baseline abdominal pain and bloating on response to lubiprostone in patients with irritable bowel syndrome with constipation. Aliment Pharmacol Ther 2016;44:1114-22.



39. Webster LR, Brewer RP, Lichtlen P, Losch-Beridon T, Mareya S, Wang M. Efficacy of lubiprostone for the treatment of opioid-induced constipation, analyzed by opioid class. Pain Med 2018;19:1195-205.



40. Gras-Miralles B, Cremonini F. A critical appraisal of lubiprostone in the treatment of chronic constipation in the elderly. Clin Interv Aging 2013;8:191-200.


41. Chiarioni G, Heymen S, Whitehead WE. Biofeedback therapy for dyssynergic defecation. World J Gastroenterol 2006;12:7069-74.



42. Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology 2006;130:657-64.


43. Heymen S, Scarlett Y, Jones K, Ringel Y, Drossman D, Whitehead WE. Randomized, controlled trial shows biofeedback to be superior to alternative treatments for patients with pelvic floor dyssynergia-type constipation. Dis Colon Rectum 2007;50:428-41.


44. Rao SS, Seaton K, Miller M, Brown K, Nygaard I, Stumbo P, et al. Randomized controlled trial of biofeedback, sham feedback, and standard therapy for dyssynergic defecation. Clin Gastroenterol Hepatol 2007;5:331-8.


45. Glia A, Gylin M, Gullberg K, Lindberg G. Biofeedback retraining in patients with functional constipation and paradoxical puborectalis contraction: comparison of anal manometry and sphincter electromyography for feedback. Dis Colon Rectum 1997;40:889-95.


46. Heymen S, Wexner SD, Vickers D, Nogueras JJ, Weiss EG, Pikarsky AJ. Prospective, randomized trial comparing four biofeedback techniques for patients with constipation. Dis Colon Rectum 1999;42:1388-93.









