1. Rizzoli R, Bonjour JP, Ferrari SL. Osteoporosis, genetics and hormones. J Mol Endocrinol 2001;26:79-94. PMID:
11241160.


2. WHO Study Group. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO Study Group. World Health Organ Tech Rep Ser 1994;843:1-129. PMID:
7941614.

3. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 2006;17:1726-1733. PMID:
16983459.



4. Felson DT, Zhang Y, Hannan MT, Anderson JJ. Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Miner Res 1993;8:567-573. PMID:
8511983.


5. Beck TJ, Oreskovic TL, Stone KL, Ruff CB, Ensrud K, Nevitt MC, et al. Structural adaptation to changing skeletal load in the progression toward hip fragility: the study of osteoporotic fractures. J Bone Miner Res 2001;16:1108-1119. PMID:
11393788.


6. Taaffe DR, Cauley JA, Danielson M, Nevitt MC, Lang TF, Bauer DC, et al. Race and sex effects on the association between muscle strength, soft tissue, and bone mineral density in healthy elders: the Health, Aging, and Body Composition Study. J Bone Miner Res 2001;16:1343-1352. PMID:
11450711.


7. Pluijm SM, Visser M, Smit JH, Popp-Snijders C, Roos JC, Lips P. Determinants of bone mineral density in older men and women: body composition as mediator. J Bone Miner Res 2001;16:2142-2151. PMID:
11697812.


8. Wang MC, Bachrach LK, Van Loan M, Hudes M, Flegal KM, Crawford PB. The relative contributions of lean tissue mass and fat mass to bone density in young women. Bone 2005;37:474-481. PMID:
16040285.


9. Reid IR, Plank LD, Evans MC. Fat mass is an important determinant of whole body bone density in premenopausal women but not in men. J Clin Endocrinol Metab 1992;75:779-782. PMID:
1517366.


11. Hsu YH, Venners SA, Terwedow HA, Feng Y, Niu T, Li Z, et al. Relation of body composition, fat mass, and serum lipids to osteoporotic fractures and bone mineral density in Chinese men and women. Am J Clin Nutr 2006;83:146-154. PMID:
16400063.



12. Park JH, Song YM, Sung J, Lee K, Kim YS, Kim T, et al. The association between fat and lean mass and bone mineral density: the Healthy Twin Study. Bone 2012;50:1006-1011. PMID:
22306928.


13. Kim JH, Choi HJ, Kim MJ, Shin CS, Cho NH. Fat mass is negatively associated with bone mineral content in Koreans. Osteoporos Int 2012;23:2009-2016. PMID:
22006041.


14. Kim CJ, Oh KW, Rhee EJ, Kim KH, Jo SK, Jung CH, et al. Relationship between body composition and bone mineral density (BMD) in perimenopausal Korean women. Clin Endocrinol (Oxf) 2009;71:18-26. PMID:
19178508.


15. Fu X, Ma X, Lu H, He W, Wang Z, Zhu S. Associations of fat mass and fat distribution with bone mineral density in pre- and postmenopausal Chinese women. Osteoporos Int 2011;22:113-119. PMID:
20306018.


16. Bredella MA, Torriani M, Ghomi RH, Thomas BJ, Brick DJ, Gerweck AV, et al. Determinants of bone mineral density in obese premenopausal women. Bone 2011;48:748-754. PMID:
21195217.


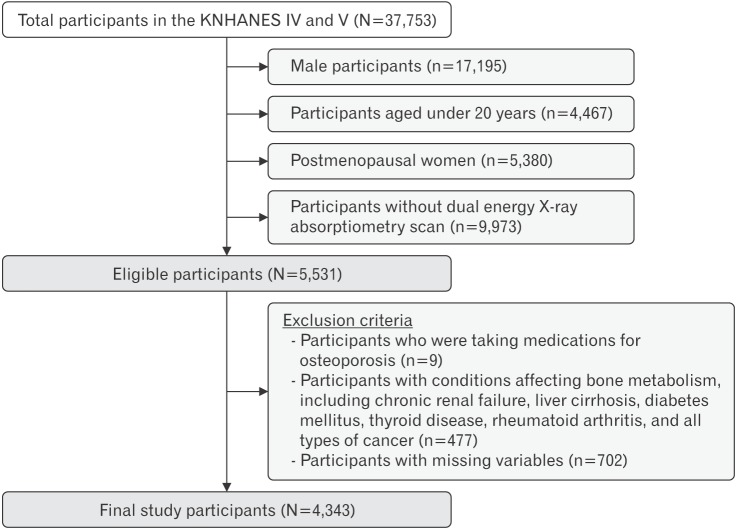
17. Korea Centers for Disease Control and Prevention. The fourth and the fifth Korea National Health and Nutrition Examination Survey (KNHANES IV & V). Cheongju: Korea Centers for Disease Control and Prevention; 2008ŌĆō2011.
18. Schousboe JT, Shepherd JA, Bilezikian JP, Baim S. Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on bone densitometry. J Clin Densitom 2013;16:455-466. PMID:
24183638.


19. Oh JY, Yang YJ, Kim BS, Kang JH. Validity and reliability of Korean version of International Physical Activity Questionnaire (IPAQ) short form. J Korean Acad Fam Med 2007;28:532-541.
20. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412-419. PMID:
3899825.



21. World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment. Geneva: World Health Organization; 2000.
23. Seeman E, Hopper JL, Young NR, Formica C, Goss P, Tsalamandris C. Do genetic factors explain associations between muscle strength, lean mass, and bone density?: a twin study. Am J Physiol 1996;270(2 Pt 1):E320-E327. PMID:
8779955.


24. Nguyen TV, Howard GM, Kelly PJ, Eisman JA. Bone mass, lean mass, and fat mass: same genes or same environments? Am J Epidemiol 1998;147:3-16. PMID:
9440393.



26. Ahn SH, Lee SH, Kim H, Kim BJ, Koh JM. Different relationships between body compositions and bone mineral density according to gender and age in Korean populations (KNHANES 2008ŌĆō2010). J Clin Endocrinol Metab 2014;99:3811-3820. PMID:
24960546.


27. Kim YM, Kim SH, Kim S, Yoo JS, Choe EY, Won YJ. Variations in fat mass contribution to bone mineral density by gender, age, and body mass index: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008ŌĆō2011. Osteoporos Int 2016;27:2543-2554. PMID:
27112764.



28. Ho-Pham LT, Nguyen UD, Nguyen TV. Association between lean mass, fat mass, and bone mineral density: a meta-analysis. J Clin Endocrinol Metab 2014;99:30-38. PMID:
24384013.


29. Reid IR. Fat and bone. Arch Biochem Biophys 2010;503:20-27. PMID:
20599663.


30. Lim JS, Kim KM, Rhee Y, Lim SK. Gender-dependent skeletal effects of vitamin D deficiency in a younger generation. J Clin Endocrinol Metab 2012;97:1995-2004. PMID:
22442269.