 |
 |
- Search
| Korean J Fam Med > Volume 39(6); 2018 > Article |
|
Abstract
Background
Methods
Results
Figure.┬Ā1.

Figure.┬Ā2.
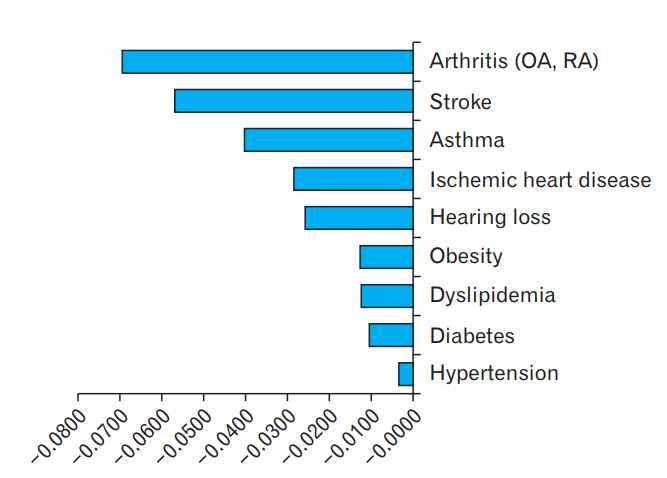
Figure.┬Ā3.
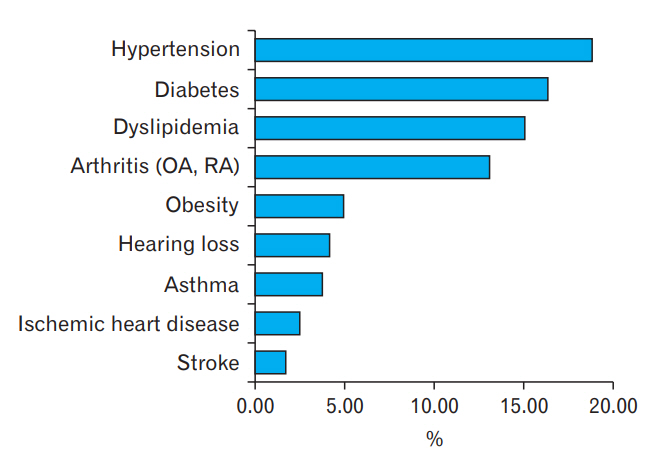
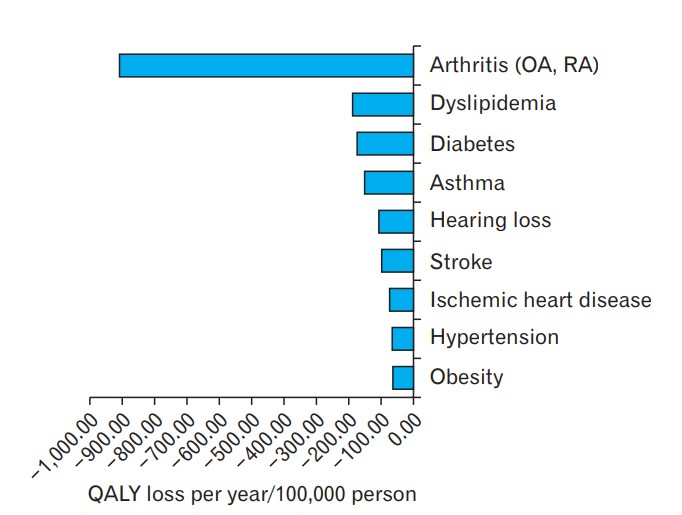
Figure.┬Ā4.
Table┬Ā1.
| Characteristic | Normal group | Hearing loss group* | Total | P-valueŌĆĀ |
|---|---|---|---|---|
| Age (y) | <0.01 | |||
| ŌĆā19ŌĆō29 | 2,431 | 2 | 2,433 | |
| ŌĆā30ŌĆō39 | 3,712 | 8 | 3,720 | |
| ŌĆā40ŌĆō49 | 4,586 | 26 | 4,612 | |
| ŌĆā50ŌĆō59 | 4,608 | 95 | 4,703 | |
| ŌĆā60ŌĆō69 | 3,853 | 359 | 4,212 | |
| ŌĆā70ŌĆō79 | 2,420 | 644 | 3,064 | |
| ŌĆāŌēź80 | 280 | 273 | 553 | |
| Sex | <0.01 | |||
| ŌĆāMen | 9,207 | 756 | 9,963 | |
| ŌĆāWomen | 12,683 | 651 | 13,334 | |
| Education | <0.01 | |||
| ŌĆāŌēżElementary school | 5,188 | 956 | 6,144 | |
| ŌĆāŌēżMiddle school | 2,481 | 190 | 2,671 | |
| ŌĆāŌēżHigh school | 7,664 | 192 | 7,856 | |
| ŌĆāŌēźGraduate school | 6,544 | 66 | 6,610 | |
| Occupation | <0.01 | |||
| ŌĆāWhite collar | 7,383 | 77 | 7,460 | |
| ŌĆāBlue collar | 5,721 | 421 | 6,142 | |
| ŌĆāUnemployed | 8,717 | 906 | 9,623 | |
| Household income | <0.01 | |||
| ŌĆāLowest quantile | 3,850 | 735 | 4,585 | |
| ŌĆāSecond quantile | 5,533 | 325 | 5,858 | |
| ŌĆāThird quantile | 6,045 | 190 | 6,235 | |
| ŌĆāHighest quantile | 6,248 | 147 | 6,395 | |
| Smoking status | <0.01 | |||
| ŌĆāNon-smoker | 13,620 | 702 | 14,322 | |
| ŌĆāEx-smoker | 3,322 | 371 | 3,693 | |
| ŌĆāCurrent smoker | 4,948 | 334 | 5,282 | |
| Marital status | <0.01 | |||
| ŌĆāMarried | 19,029 | 1,393 | 20,422 | |
| ŌĆāSingle | 2,850 | 14 | 2,864 |
Definition of white collar: worker who performs semi-professional, office, or sales-coordination tasks. Definition of blue collar: worker who performs non-agricultural manual labor.
Table┬Ā2.
| Chronic diseases | Marginal utilities | 95% confidence interval | P-value* |
|---|---|---|---|
| Hearing loss | -0.0224 | -0.0363 to -0.0086 | <0.01 |
| Hypertension | -0.0025 | -0.0093 to 0.0043 | 0.472 |
| Diabetes | -0.0083 | -0.0149 to -0.0017 | 0.013 |
| Dyslipidemia | -0.0138 | -0.0215 to -0.0060 | <0.01 |
| Arthritis (osteoarthritis, rheumatoid arthritis) | -0.0692 | -0.0780 to -0.0603 | <0.01 |
| Stroke | -0.0579 | -0.0779 to -0.0379 | <0.01 |
| Ischemic heart disease | -0.0355 | -0.0549 to -0.0161 | <0.01 |
| Obesity | -0.0119 | -0.0219 to -0.0018 | 0.021 |
| Asthma | -0.0394 | -0.0553 to -0.0235 | <0.01 |
The adjusted factors were age, sex, smoking status, household income, education, occupation, marital status, hypertension, diabetes, dyslipidemia, osteoarthritis or rheumatoid arthritis, stroke, ischemic heart disease, obesity, and asthma. Hearing loss was defined as a moderate to severe grade on the World Health Organization hearing loss classification. Hypertension was defined as a systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg or diagnosis by a physician.
Diabetes was defined as a glycated hemoglobin level >6.5% or medication for diabetes or diagnosis by a physician. Dyslipidemia was defined as a total cholesterol level >240 mg/dL or diagnosis by a physician. Obesity was defined as a body mass index of Ōēź30 kg/m2. Other chronic diseases were defined as diagnosed or recognized by a physician. Marginal utilities were weighted to the Korean standard population >19 years of age.
Table┬Ā3.
Prevalence estimates were weighted to the Korean standard population >19 years of age. Hearing loss was defined as moderate-to-severe grade on the World Health Organization hearing loss classification. Hypertension was defined as systolic blood pressure of >140 mm Hg or diastolic blood pressure of >90 mm Hg or diagnosis by a physician. Diabetes was defined as hemoglobin A1c level of >6.5% or medication for diabetes or diagnosis by a physician. Dyslipidemia was defined as total cholesterol level of >240 mg/dL or diagnosis by a physician. Obesity was defined as a body mass index of Ōēź30 kg/m2. Other chronic diseases were defined as diagnosed or recognized by a physician.
Table┬Ā4.
| Chronic diseases | Marginal utilities | 95% confidence interval | P-value* |
|---|---|---|---|
| Hearing loss | -0.0169 | -0.0327 to -0.0012 | 0.035 |
| Hypertension | -0.0017 | -0.0097 to 0.0064 | 0.686 |
| Diabetes | -0.0074 | -0.0166 to 0.0019 | 0.12 |
| Dyslipidemia | -0.0100 | -0.0198 to -0.0002 | 0.045 |
| Arthritis (osteoarthritis, rheumatoid arthritis) | -0.0746 | -0.0857 to -0.0636 | <0.01 |
| Stroke | -0.0635 | -0.0878 to -0.0392 | <0.01 |
| Ischemic heart disease | -0.0410 | -0.0663 to -0.0157 | <0.01 |
| Obesity | -0.0140 | -0.0339 to 0.0060 | 0.169 |
| Asthma | -0.0494 | -0.0774 to -0.0215 | <0.01 |
The adjusted factors were age, sex, smoking status, household income, education, occupation, marital status, hypertension, diabetes, dyslipidemia, osteoarthritis or rheumatoid arthritis, stroke, ischemic heart disease, obesity, and asthma. Hearing loss was defined as moderate-to-severe grade on the World Health Organization hearing loss classification. Hypertension was defined as systolic blood pressure of >140 mm Hg or diastolic blood pressure of >90 mm Hg or diagnosis by a physician.
Diabetes was defined as hemoglobin A1c level of >6.5% or medication for diabetes or diagnosis by a physician. Dyslipidemia was defined as total cholesterol level of >240 mg/dL or diagnosis by a physician. Obesity was defined as a body mass index of Ōēź30 kg/m2. Other chronic diseases were defined as diagnosed or recognized by a physician. Marginal utilities were weighted to the Korean standard population aged >19 years.
Table┬Ā5.
Prevalence estimates were weighted to the Korean standard population >19 years of age. Hearing loss was defined as moderate-to-severe grade on the World Health Organization hearing loss classification. Hypertension was defined as systolic blood pressure of >140 mm Hg or diastolic blood pressure of >90 mm Hg or diagnosis by a physician. Diabetes was defined as HbA1c level of >6.5% or medication for diabetes or diagnosis by a physician. Dyslipidemia was defined as total cholesterol level of >240 mg/dL or diagnosis by a physician. Obesity was defined as a body mass index of Ōēź30 kg/m2. Other chronic diseases were defined as diagnosed or recognized by a physician.
REFERENCES
- TOOLS







