Trends of the New Outpatients in a University-based Family Practice
Article information
Abstract
Background
Analysis of outpatient visits to primary care offers essential data for residency training by understanding 'reasons for encounter (RFE).' This study was designed to recognize the effect of population aging on demographic characteristics and RFEs.
Methods
We included all patients who had visited family practice clinic in Kyung Hee University Hospital in Seoul during each first 5 working days of September, October, and November in 2001 and 2008. New patients included those who hadn't visited within the last 6 months or more. Information on each patient's age, sex, and reason for encounter was obtained from the electronic medical record. The RFEs were compared using International Classification of Primary Care (ICPC)-2-E.
Results
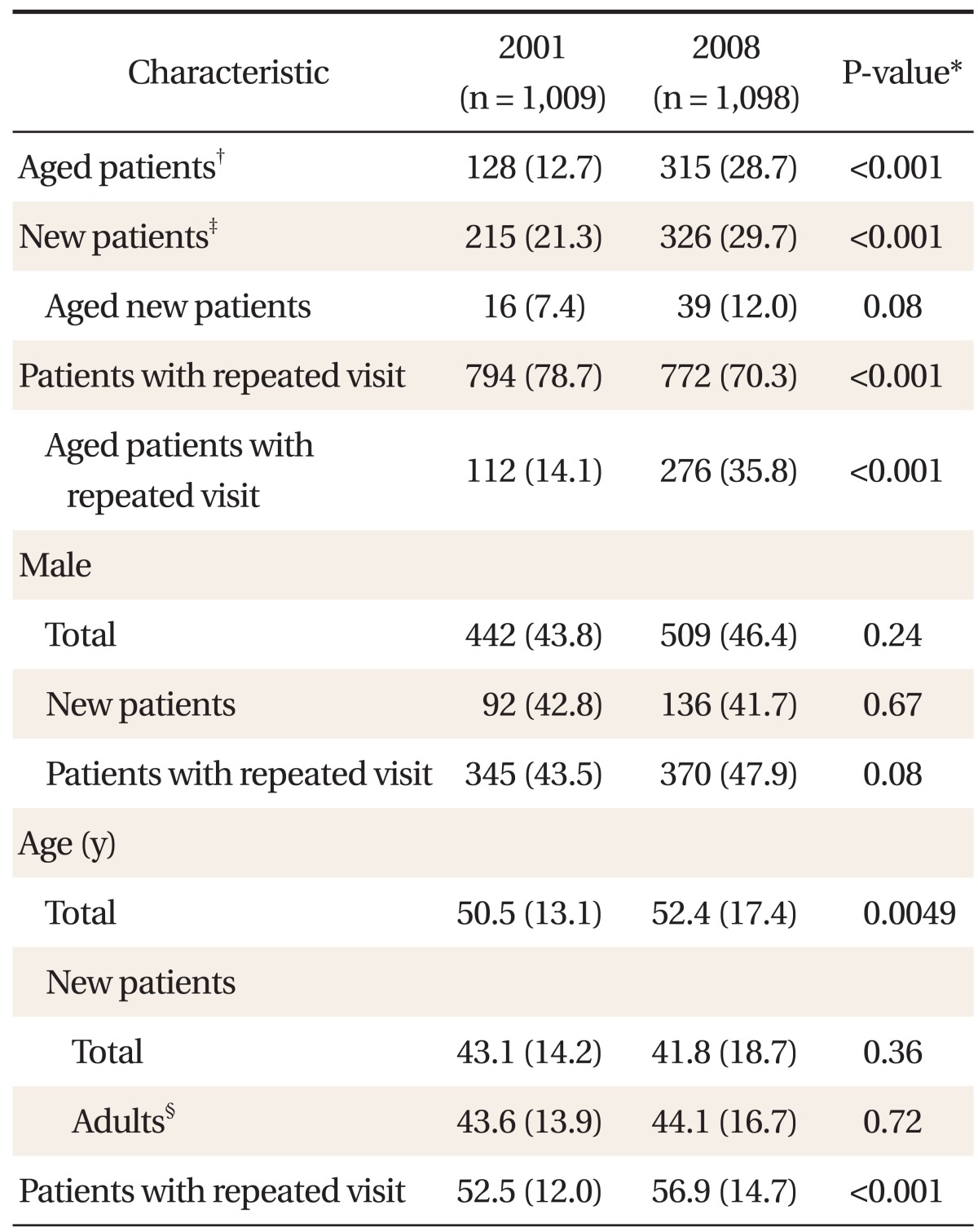
Mean age of overall outpatients was 50.5 and 52.4 years in 2001 and 2008 respectively. The number of new outpatient visits increased from 215 (21.3%) to 326 (29.7%) between 2001 and 2008 (P < 0.001) along with the number of patients aged 65 or more from 7.4% to 12.0% (P = 0.08). Mean age of established patients was 52.5 and 56.9 years (P < 0.001), and the patients aged 65 or more was 14.1% and 35.8% (P < 0.001) in 2001 and 2008 respectively. Analysis by ICPC-2-E revealed a decrease in chapter A in 2008 (P = 0.03) and an increase in chapter F, L, and X (P = 0.01, 0.003, <0.001). Component 1 had increased (P = 0.01), and component 2 had decreased (P = 0.04) in proportion.
Conclusion
Changes in population composition have brought a shift of the distribution of age in outpatients, more significantly in follow-up patients. Comparison by ICPC-2-E showed changes in RFEs of new patients between 2001 and 2008.
INTRODUCTION
Analysis of outpatients' reasons for encounter (RFEs) and diagnoses in primary medical services provides students and residents with educational resources.1) The International Classification of Primary Care (ICPC) was published by World Organization of Family Doctors (WONCA) in 1987. Unlike International Classification of Diseases (ICD), ICPC enables classification of patients by using a person-centered approach rather than a disease-centered approach by comprehensively incorporating RFEs, clinical process, and diagnosis. It consists of 17 chapters, each with an alphabetical code and divided into 7 components dealing with symptoms and complaints, diagnostic, screening, preventive procedures, and so forth. The second edition was published in 1998 followed by ICPC-2-E, an electronic version always available on website, which was introduced in 2000.2) A couple of attempts had been made to analyze RFEs of outpatients by ICPC classification in Korea. According to the study by Kim et al.,3) ICPC-2 includes REF classification missing from ICD-10, thus complementing the ICD-10 limitations in appropriately evaluating RFEs.
Recently, demographic change by rapid population aging has become a social issue. Korea became an 'aging society' in 2009 with a 10.7% of its population aged 65 years or older. In 2018, Korea will become an 'aged society' with 14.3% of the population aged 65 or over and eventually turn into a 'super-aged society' by 2026 when the ratio of aged population reaches 20.8%.4) This sudden change in population composition has significantly influenced the demographic characteristics of the outpatients visiting primary care service. Oh et al.5) reported that the proportion of people aged 65 or older was limited to 6.7% in 1988 according to the analysis of primary care services, which increased to 13.9% in 2001 according to a recent study by a university hospital family practice, projecting that the proportion of older patients is rising.6)
This study attempted to analyze the trends in new outpatients at a university-based family practice by ICPC-2-E classification to recognize a possible shift in age groups as well as changes in their main RFEs. The extracted data can then contribute in implementation of training programs that focus on the common symptoms and 'reasons for encounter.'
METHODS
1. Study Population and Period
To analyze the trends in new outpatients, we included all patients who had paid visits to the Family Practice Clinic in Kyung Hee University Hospital in Seoul during each first five working days of September, October, and November in 2001 and 2008, respectively. Patients who had not visited the clinic within the last 6 months or more were regarded as new patients. Kyung Hee University Hospital is located in eastern Seoul with a mostly middle class population where a quite a portion of senior citizens live in close proximity.
2. Study Protocol
We separated new patients from those who had made repeated visits by reviewing each year's outpatient lists adopted from the electronic medical records (EMR), from which we also collected information on each patient's sex, age and the main RFE. Established patients were excluded from the study to obviate the possible bias occurring from repeated inclusion of the same RFE. In case of short-term follow-up, we only compared new patients in 2001 and 2008 to preclude bias caused from any changes in the RFE.
The main RFE was recruited from the item 'chief complaint' in the EMR. If there were multiple chief complaints, we used the first recorded complaint only. In case there was no chief complaint recorded, we used the first mentioned symptom as the main RFE. Collected data was sorted according to ICPC-2-E classification.
Chapters were systematically organized by RFEs and represented by alphabetic letters: A: general and unspecified; B: blood, blood forming organs and immune mechanism; D: digestive; F: eye; H: ear; K: cardiovascular; L: musculoskeletal; N: neurological; P: psychological; R: respiratory; S: skin; T: endocrine/metabolic and nutritional; U: urological; W: pregnancy, childbearing, family planning; X: demale genital; Y: male genital; Z: social problems. Each chapter divided RFEs into seven components in terms of symptoms, diagnosis, treatment, test results, administrative activities, and so forth.
3. Statistical Analysis
The main RFEs were sorted according to number of each year's new outpatients, their mean age, age-specific distribution, and ICPC-2 classification. T-test was employed for analysis of the age variant. In terms of the remaining variants, we used Fisher's exact test, if the sample size was 5 or less and χ2 test, if the sample size was greater than 5. Statistical significance used was 5% (P < 0.05). Stata/SE ver. 10.0 (StataCorp, College Station, TX, USA) was used for all statistical analyses.
RESULTS
1. Baseline Demographic Characteristics
The number of overall outpatient visits was 1,009 in 2001 and 1,098 in 2008. The total number of new outpatient visits increased from 215 (21.3%) to 326 (29.7%) between 2001 and 2008 (P < 0.001). Mean age of the outpatients in total was 50.5 and 52.4 years (P = 0.0049), respectively. Of these, mean age of the new patients was 43.1 and 41.8 years (P = 0.36), whereas that of established patients was 52.5 and 56.9 years, respectively. In 2001, there was no patient younger than 10 years, while in 2008, there were as many as 16 patients; we thereby attempted to compare only adult patients older than 18 years of age. For the new patient group, the mean age (standard deviation, SD) of the adult patients aged 18 or more was 43.6 (13.9) and 44.1 (16.7) years, respectively (P = 0.72).
To observe the trends in demographic composition of patients, we counted the number of patients aged 65 years or older. Overall, the proportion of patients aged 65 years or older had increased significantly from 128 (12.7%) to 315 (28.7%) between 2001 and 2008 (P < 0.001), and that of established patients had increased from 112 (14.1%) to 276 (35.8%), respectively (P < 0.001) (Table 1). However, there was no significant difference in the proportion of patients aged 65 years or older between 2001 and 2008 in terms of new outpatient visits (16 [7.4%] vs. 39 [12.0%], P = 0.08).
2. Comparison of the Reasons for Encounter
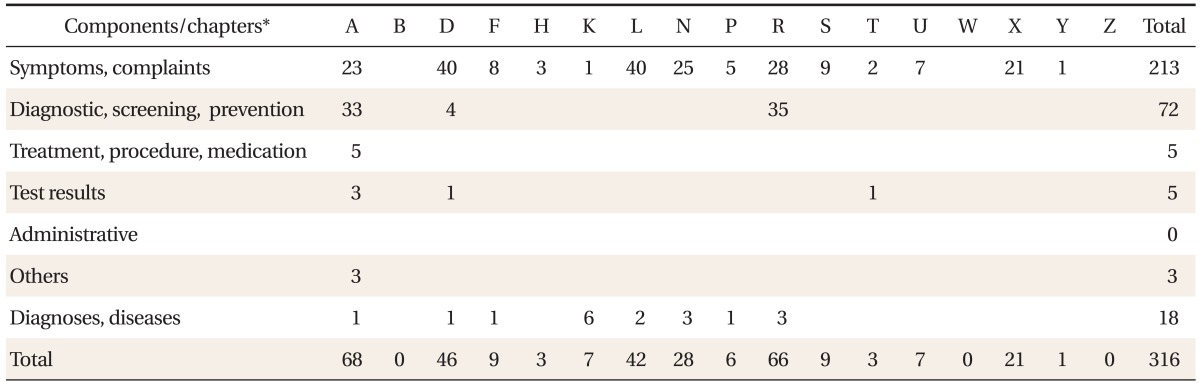
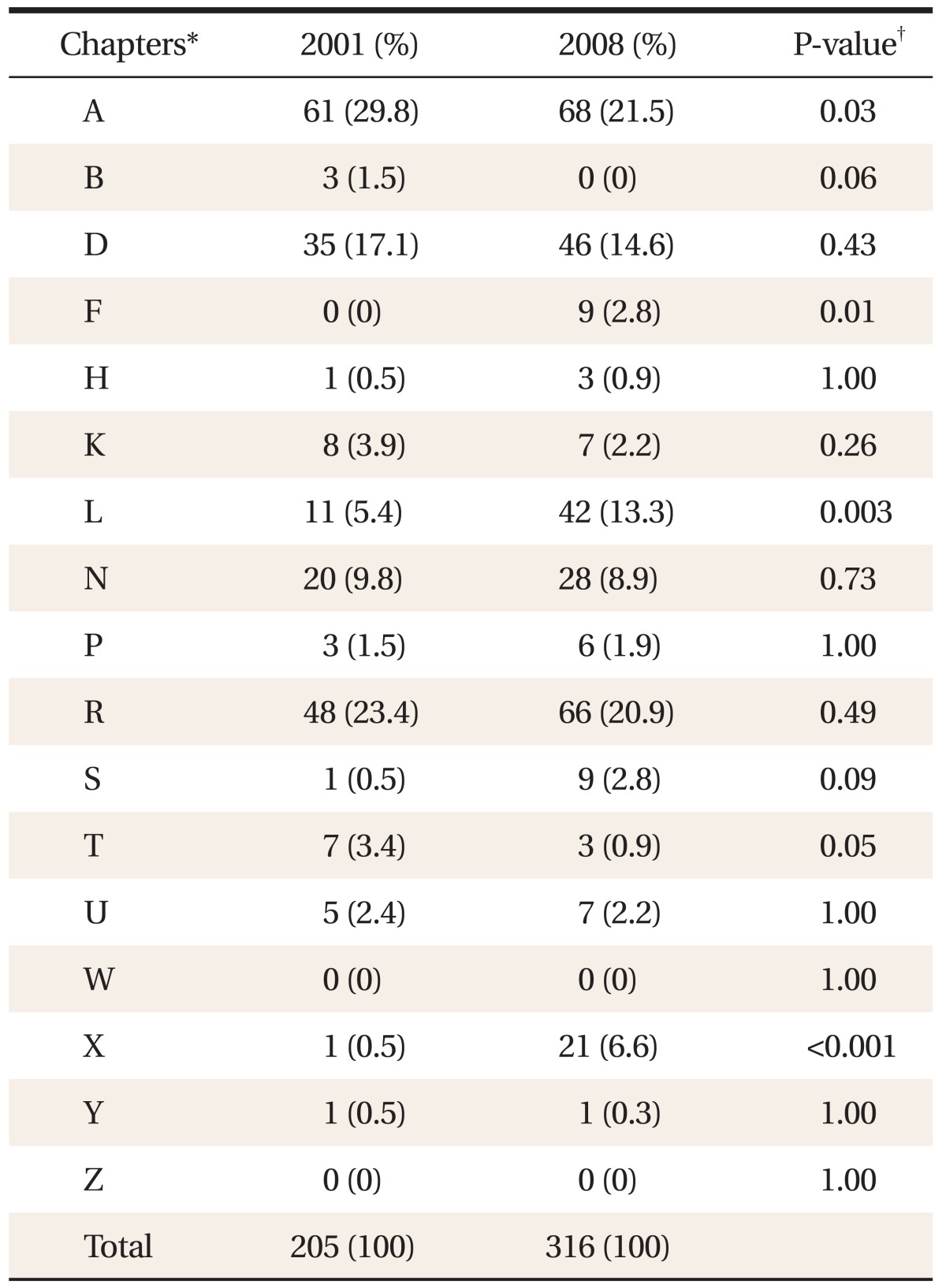
We analyzed medical records of new patients who visited the Family Medicine Clinic at Kyung Hee University Hospital, thus obtaining 205 and 316 main RFEs in 2001 and 2008, respectively. Patient-reported RFEs were then classified according to the 17 chapters and 7 components of ICPC-2-E (Tables 2 and 3).
A comparison of the main RFEs of 2001 and 2008 showed that the proportion of chapter A (general and unspecified) had decreased significantly from 29.8% to 21.5% between 2001 and 2008, respectively (P = 0.03) (Table 4) while that of chapters F (eye), L (musculoskeletal) and X (female genital) had significantly increased (P = 0.01, 0.003, <0.001 respectively) (Table 4).
Upon analyzing the main RFEs based on the 7 components, the proportion of component 1 (symptoms, complaints) had increased from 57.1% to 67.4% (P = 0.01), and that of component 2 (diagnostic, screening, prevention) had decreased from 30.7% to 22.8% (P = 0.04) (Figure 1).
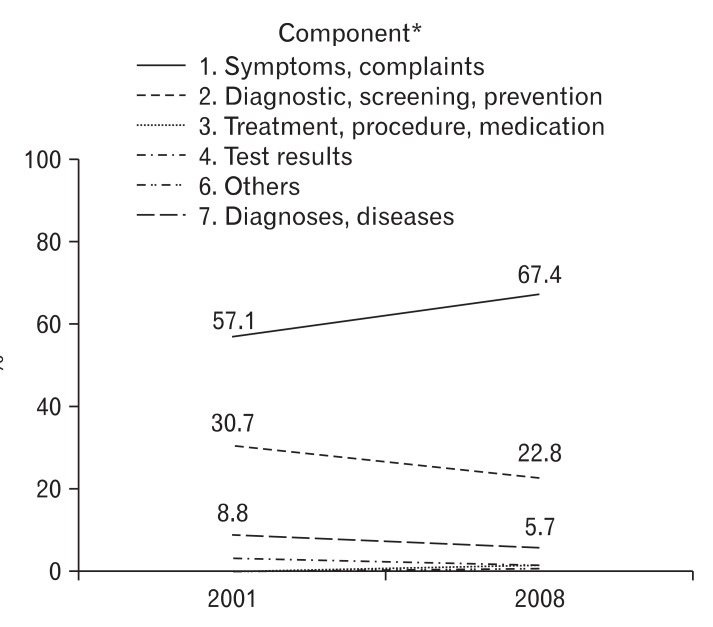
Comparison of the Components for new patients between 2001 and 2008. *P-value obtained from χ2 test and Fisher's exact test (1: 0.01, 2: 0.04, 3: 0.16, 4: 0.23, 5: 0.28, 6: 0.17). No patient encountered for the component 5 (administrative). So we did not describe it in this figure.
The 5 most commonly reported codes of ICPC-2-E in 2008 were identified by order of frequency (Figure 2), and R44 (preventive immunizations/medications-respiratory) was found to be most frequently reported. In comparison with the data obtained in 2001, the rate of utilization of code X11 (menopausal symptom/complaint) had increased from 0.5% to 5.4% (P = 0.002), whereas that of A30 (medical examination/evaluation-complete, general medical exam) had decreased from 18.1% to 3.5% (P < 0.001) (Figure 2).

Comparison of common§ ICPC coding for new patients in 2008 with 2001. *P = 0.002, from Fisher's exact test. †P < 0.001, from χ2 test. §10 or more patients. ‡R44: preventive immunizations/medications (respiratory), X11: menopausal symptom/complaint, R21: throat symptom/complaint, A30: medical examination/evaluation-complete, N01: headache, N17: vertigo/dizziness.
DISCUSSION
In a previous study by Hwang et al.7) which included 15,601 patients of the Family Medicine Clinic at Kyung Hee University Hospital from 1991 to 1992, proportion of new patients accounted for 28.2% of the total patients, and that of the patients aged 65 years or older accounted for 8.1%, The most frequently reported RFE was identified to be general medical examination (5.7%). In this study, the percentage of patients aged 65 or older increased from 12.7% to 28.7% between 2001 and 2008. Of new patients, the proportion of those aged 65 or more increased from 7.4% to 12.0% between 2001 and 2008 but lacked statistical significance presumably due to the small sample size. Both results mentioned above were higher than those obtained by the 'Korean Population Prospects (2005)' published by Korea National Statistical Office4) from which we can assume that the general trend of population aging had influenced the age-group distribution of the new patients as well as the established patients. This study was aimed at examining the aging trend of new patients, which turned out to have no statistical significance. However, conjecturing from the significant increase of the mean age and the proportion of the established patients from 52.5 to 56.9 and 14.1% to 35.8%, respectively, we could indirectly make a supposition that the percentage of elderly patients visiting the hospital from chronic illnesses is rising.
The main RFEs were sorted by using the ICPC-2-E classification. Analysis by chapters showed that complaints of musculoskeletal and female genital tract related symptoms increased significantly from 11 (5.4%) and 1 (0.5%) to 42 (13.3%) and 21 (6.6%), respectively between 2001 and 2008. Mean age of the patients with musculoskeletal complaints was 41.7 (SD, 14.7) in 2001 and 47.9 (SD, 16.5) in 2008. Among them, patients aged 65 or more was 0 and 8, respectively (P = 0.116). Of the 42 patients complaining of female genital tract related symptoms, 17 patients presented with menopausal symptoms in 2008; it is a significant increase since only one patient had presented with such symptoms in 2001 (P = 0.002). After the publication of Women's Health Initiative (WHI) Study in 2002 regarding oral hormone replacement therapy for menopausal symptoms, there were increasing concerns about hormone replacement therapy. But in the study by Choi et al.,8) 79.8% of women recognized the necessity of menopausal symptom treatment. The Study Group of Menopause9) concluded that even if overall prescriptions for hormone replacement had decreased, prescriptions for low dose pills, alternative or complementary therapies were increasing. We supposed that the increase in the number of patients with complaints of menopausal symptoms observed in this study was due to the increasing awareness of the necessity for treating menopausal symptoms.
In the analysis by components, like many previous studies, component 1 (symptoms/complaints) was the leading RFE both in 2001 and 2008, and had increased significantly in frequency.1,10-12) Since the number of patients who visited for a comprehensive medical evaluation decreased from 37 to 11, component 2 (diagnostic, screening, prevention) had decreased significantly in frequency. In 2001, family practice in this hospital was responsible for the comprehensive medical testing center. However, since 2008, as the department of internal medicine became in charge of the center, patients no longer needed to visit family practice for general medical examination, accounting for the decreased frequency of application of component 2. For the same reason, application of chapter A (general and unspecified) decreased.
In 2008, respiratory tract disease prevention (R44: preventive immunizations/medications-Respiratory) was the most common reason for encounter with a total 35 cases of vaccination (32 of influenza vaccination, 3 of pneumococcal vaccination). We could make a supposition that the lowering of the recommended age for influenza vaccination from 65 years to 50 years in 2004 would result in a significant increase in vaccination rate. In this study, however, the number of patients visiting for prevention of respiratory tract diseases increased only without a statistical significant result (9.3% to 11.1%, P = 0.51).
There are several limitations to this study. First, the sample size was small. We included patients visits made during each first five working days of September, October and November rather than all working days. Second, we conducted this research using data obtained from a single university-based family practice thus we were unable to exclude bias from pursuing one geographic location. Third, we were unable to retrieve the main RFEs of 10 cases in both 2001 and 2008 due to loss or destruction of the medical records, possibly affecting the overall results of analysis.
Despite the limitations, this study is distinguished from previous studies in that we compared reasons for encounter and age-specific distribution of new outpatients with a 7 year interval. We were also able to observe that the number of patients with musculoskeletal and female genital tract problems had increased and that prevention of respiratory system diseases was the most frequent reason for encounter. By offering our residents with an intensive education based on the study results, we can help strengthen competitiveness in treating diseases that are frequently encountered in primary health care service.
In summary, owing to population aging, there was a significant increase in the proportion of elderly established patients in Kyung Hee University Hospital. Comparison by ICPC-2-E classification revealed a significant increase in new patients visiting for musculoskeletal, ophthalmic or female genital tract problems since 2001.