Factors of Compliance in Patients with Hypercholesterolemia Using Rosuvastatin in Primary Care
Article information
Abstract
Background
In order to evaluate the factors of compliance with a lipid lowering therapy, a prospective observational study of patients with hypercholesterolemia using rosuvastatin was carried out.
Methods
A total of 2,607 patients who were newly prescribed rosuvastatin were enrolled from 32 family physicians in Korea from March 2009 to December 2009. Of them, 301 patients were excluded due to incomplete data or follow-up compliance data. The patients were regularly observed to ascertain the compliance associated with rosuvastatin at intervals of 12 and 24 weeks. We collected risk factors for the compliance using a structured questionnaire. The criteria for evaluating compliance are to measure clinic attendance, to assess the continuity of therapy, and to calculate the percentage of doses taken.
Results
Among a total of 2,306 patients, the degree of compliance was 54.1%. According to logistic regression analysis, the factors for compliance with the lipid lowering drug included old age (odds ratio [OR], 2.68; 95% confidence interval [CI], 2.09 to 3.45), frequent exercise (OR, 1.76; 95% CI, 1.43 to 2.18), previous statin therapy (OR, 4.02; 95% CI, 3.22 to 5.01), hypertension (OR, 1.80; 95% CI, 1.48 to 2.19), diabetes mellitus (OR, 2.20; 95% CI, 1.69 to 2.87), concomitant medication (OR, 2.28; 95% CI, 1.88 to 2.77), and high coronary heart disease (CHD) risk category (OR, 1.82; 95% CI, 1.39 to 2.38). The compliance decreased with high low density lipoprotein cholesterol levels (OR, 0.20; 95% CI, 0.16 to 0.26).
Conclusion
The compliance of patients using rosuvastatin was 54.1% in primary care. The factors related to higher compliance were old age, regular exercise, previous statin therapy, concomitant medication, presence of hypertension or diabetes, and higher CHD risk level.
INTRODUCTION
According to the Korean National Statistical Office in 2009, the mortality rate for cerebrovascular disease and heart disease came in 2nd and 3rd, respectively, next only to cancer.1) Thus, control of chronic diseases such as hypertension, diabetes, and hypercholesterolemia is emphasized in public health. Of them, lipid lowering therapy significantly reduces the incidence and mortality rate for cardiovascular disease (CVD) in patients with hypercholesterolemia.2,3) Therefore, the National Cholesterol Education Program Adult Treatment Panel (NCEP-ATP) III guidelines encouraged to lower the target level of cholesterol.4)
Rosuvastatin has a strong potency among several lipid lowering drugs, but has a relatively low lipophilicity and good safety.5) In addition, it is known to reduce CVD mortality when used as the primary preventative treatment in patients with low CVD risk.5) As most of the patients visiting primary care physicians are hypercholesterolemic patients with low CVD risk, this study was conducted with rosuvastatin, whose effects on primary prevention had been previously reported.
In order to obtain the goal of lipid reduction, the compliance of patients to the drugs is important, but it is commonly overlooked. The compliance was especially low in the case of chronic diseases compared to acute diseases.6) A previous study reported that the compliance of patients with hypercholesterolemia tended to decrease rapidly six months after the start of treatment.6) In addition, lipid lowering therapy in primary care mostly aims for the primary prevention of CVDs, and it was reported that the discontinuation of drugs was higher in the primary prevention than in the secondary prevention.2,7-10) Also previous studies reported that the lipid lowering drugs were continuously taken for a long time in only about 50% of cases.11,12)
However, there have been only a few studies on related factors among the studies on compliance of lipid lowering therapy.13-17) Therefore, we aimed to observe the compliance to rosuvastatin of patients with hypercholesterolemia in the primary care setting and to check the factors related to drug compliance by examining sociodemographic characteristics, previous statin use, and health related factors.
METHODS
1. Study Subjects
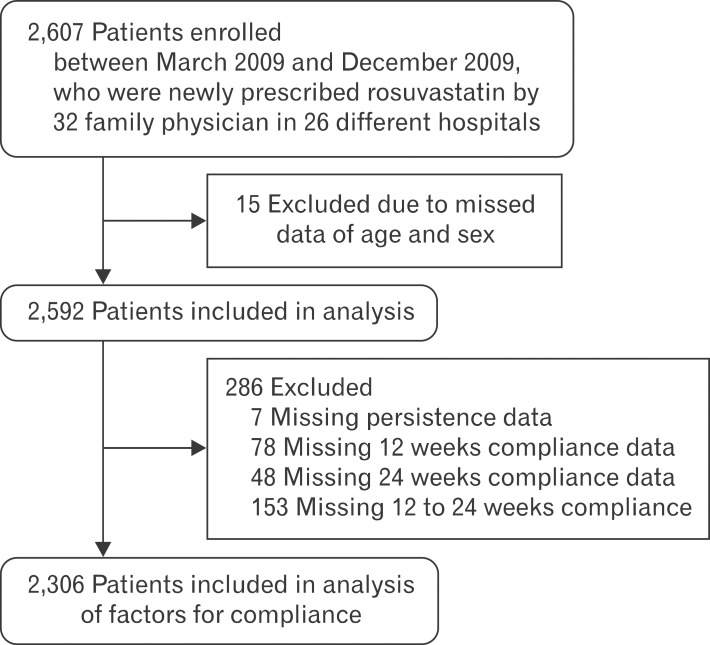
The subjects of this study were 2,607 patients who were newly prescribed rosuvastatin since March 2009 until December 2009 among the hypercholesterolemic patients who visited 32 family physicians at a total of 26 hospitals. Subjects diagnosed with hypercholesterolemia previously who received the lipid lowering therapy were also included. Of the 2,607 patients, 15 whose age or sex was not recorded were excluded and 286 were also excluded due to lack of monitoring data. Thus, a total of 2,306 patients were included in the analysis (Figure 1).
2. Methods
1) Data
Sociodemographic factors, including family history of CVDs, smoking status, drinking status, frequency of exercise, educational level, and monthly income per household were investigated using a standardized questionnaire. The medical record of patients was evaluated including age, sex, history of CVDs, use of antihypertensive medication, use of oral hypoglycemic agents, and concomitant medication. Those records were registered in the structured case record form (CRF).
In relation to smoking status, current smokers were classified as smokers, and those who had never smoked and those who had smoked in the past but do not smoke currently were classified as non-smokers. In relation to drinking status, those who drink twice or more a month were classified as drinkers, and those who drink less than that were classified as non-drinkers. The educational level was classified into 9 years or shorter, 9 through 12 years and 12 years or longer with the highest level of education as the standard, and in relation to frequency of exercise, the subjects were divided into the group that did not exercise at all for a week, the group that regularly exercised once to twice a week, and the group that regularly exercised 3 times or more a week.
2) Anthropometric measurement and laboratory tests
The body mass index (BMI) was obtained by measuring the height and weight of subjects at the beginning of treatment, and waist circumference (WC) and blood pressure was also measured. The subjects were defined as having abdominal obesity when the WC was 90 cm or more in men and 80 cm or more in women according to Asia-Pacific guidelines. The blood pressure was measured once or twice in the upper arm and was averaged for analysis. A blood test was conducted after 12 hours of not eating, thereby measuring fasting plasma glucose, total cholesterol, triglyceride, high density lipoprotein (HDL) cholesterol, and low density lipoprotein (LDL) cholesterol. When LDL cholesterol was not measured, the estimate was calculated by using Friedewald's formula.
Hypertension was defined as average blood pressure ≥140/90 mm Hg, or if the subject was taking antihypertensive medication. The diagnosis of diabetes was established by the participating physicians based on the patients' history and medical records according to current international guidelines (a recorded increased fasting plasma glucose ≥126 mg/dL, random plasma glucose ≥200 mg/dL, or the use of oral hypoglycemic medications or insulin).
Framingham scores of all patients were calculated, and according to the coronary heart disease (CHD) risk category presented in the NCEP-ATP III guideline, the cases in which there were CHD or CHD risk equivalents (peripheral arterial diseases, aneurysm of abdominal aorta, carotid artery disease with symptoms, and diabetes) and the Framingham score was higher than 20% were classified as the high CVD risk group, and the cases in which the Framingham score was 20% or lower and two or more CHD risk factors (smoking, hypertension, HDL-C of less than 40 mg/dL, family history of premature coronary artery disease [men who are younger than 55 years and women who are younger than 65 years], and age [45 years or older in men and 55 years or older in women]) were classified as the moderate CVD risk group, and cases with one or less CHD risk factor were classified as the low CVD risk group.
3) Outcome measurement of follow-up
All patients were prescribed rosuvastatin once daily at the first visit, and the dose was adjusted by the physician's decision. The follow-up visit was conducted at the 12th and 24th week after the start of rosuvastatin. At the follow-up visit, the blood pressure, anthropometric data, and serum lipid profiles were measured and compliance was evaluated. All data were recorded in the CRF and the framed CRFs were collected after the completion of a follow-up visit at the 24th week.
4) Definition of compliance
The standards used by this study to evaluate compliance were drug compliance, whether the patient visited as an outpatient, and whether rosuvastatin was stopped. Cases in which drug compliance assessed at the 12th and 24th week was less than 80% at least once, where the patient did not visit as an outpatient at the 12th or 24th week, or where the administration of medicine was stopped at the 24th week, were classified as the 'noncompliant' group, and cases in which the medicine was continuously taken at the evaluation at the 24th week and drug compliance was 80% or greater at both of the outpatient evaluations were classified as the 'compliant' group.
3. Statistical Analysis
The subjects were divided into a compliant group and a noncompliant group, as described, and all the variables were changed into categorical variables, and the differences between the two groups were examined. In addition, a logistic regression analysis was conducted by including the sociodemographic variables that showed a significant correlation with compliance in single-variate logistic regression analysis and correcting for age and sex. For all statistical analyses, the SPSS ver. 19.0 (SPSS Inc., Chicago, IL, USA) was used and P-value < 0.05 (two-tailed test) considered as statistically significant.
RESULTS
1. Baseline Characteristics of Study Participants
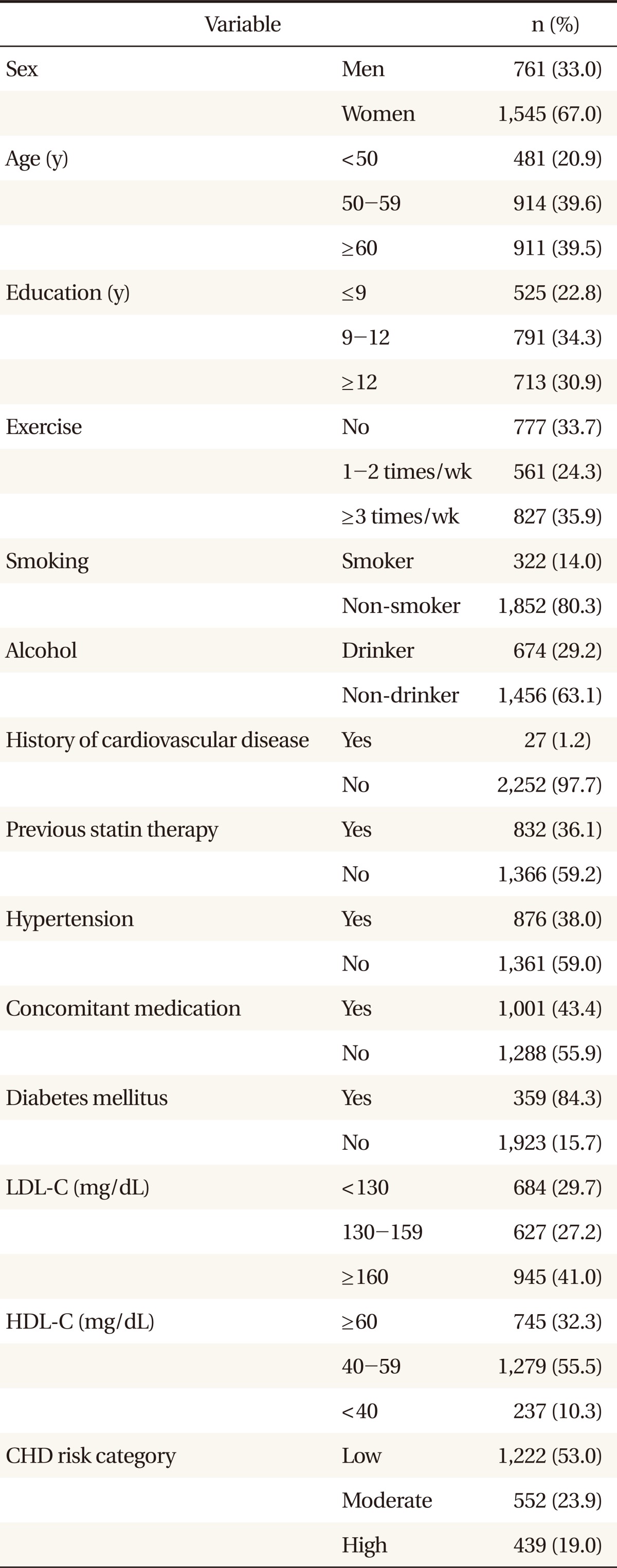
Of the 2,607 participants in the study, 2,306 persons excluding 301 were included in the subject of analysis. There were 761 men (33.0%) and 1,545 women (67.0%), and the average age was 56.9 years (± 10.1). The ratios of smokers and drinkers were 14.0% and 29.2%, respectively, and 36.1% of patients had been taking statin previously. The cases with history of cardiovascular diseases occupied 1.2% of the patients, 38.0% had hypertension, and 84.3% had diabetes. Patients with LDL cholesterol of 160 mg/dL or more occupied 41.0%, and patients with HDL cholesterol of less than 40 mg/dL occupied 10.3%. It was found that the patients with high CVD risk were 19.0% (Table 1).
2. Relationship between Sociodemographic Factors, Anthropometric Measurements, and Compliance
Participants with drug compliance of 80% or greater at the 12th week were 70%, but decreased to 61% at the 24th week, and the continuation of rosuvastatin at the 24th week was 72%. According to the previous mentioned definition, the compliant group was 54.1% and the noncompliant group was 45.9%. Of all the participants, 16.3% did not visit as outpatients at the 12th week, and 28.0% did not visit at the 24th week. The participants who did not visit at the 12th week but visited at the 24th week were 2.6%. Therefore, the participants who did not visit follow-up clinics were 78.2% of the noncompliant group. Age, sex, smoking status, drinking status, frequency of exercise, and educational level were significantly different between the compliant group and non-compliant group. However, there was no difference in abdominal obesity and BMI.
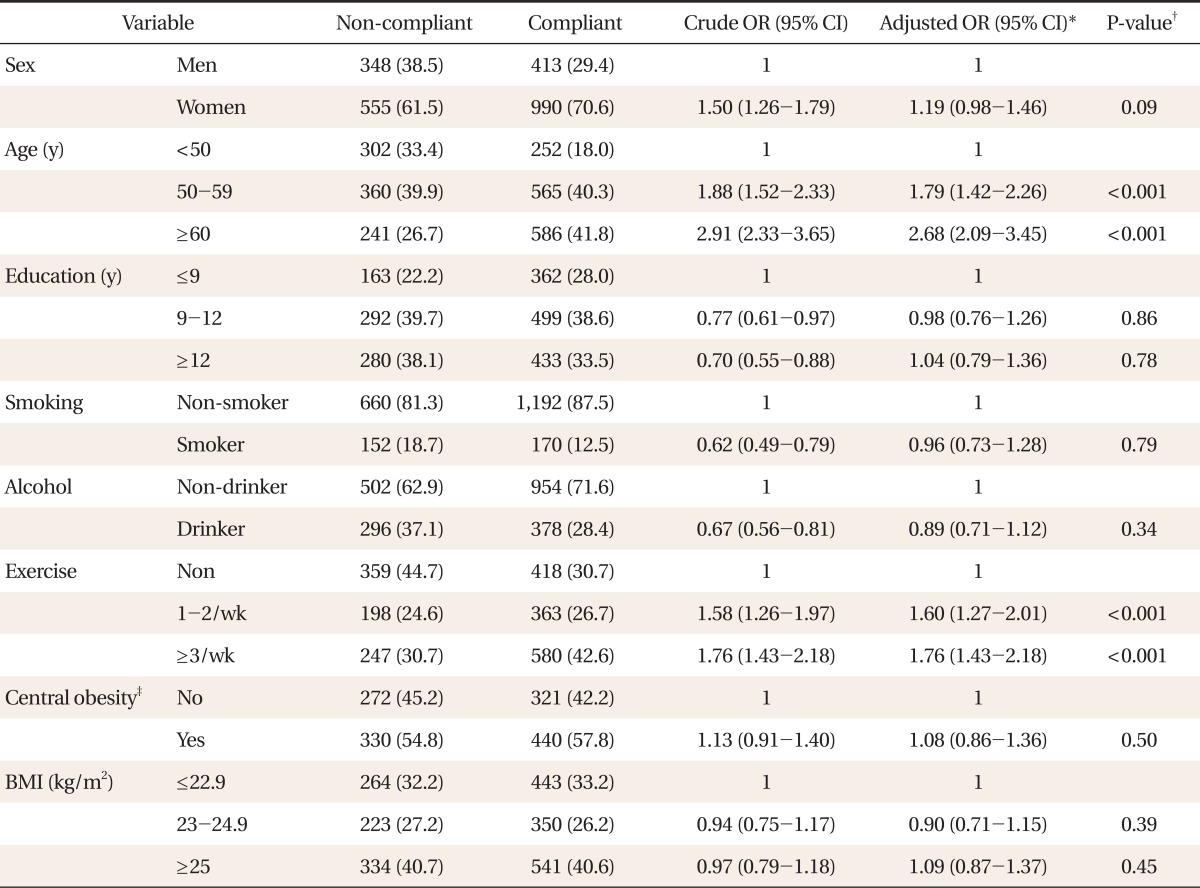
In the univariate logistic regression analysis, the compliance was higher in women, older patients, and patients demonstrating a higher frequency of regular exercise. The compliance was lower in the educational level of 12 years or longer than in that of 9 years or shorter, and in cases of smokers and drinkers. In the multivariate logistic regression analysis conducted by correcting for age, sex, and frequency of exercise, there was a tendency compliance tended to be higher in ages 60 years or older than in ages younger than 50 years, (OR, 2.68; 95% CI, 2.09 to 3.45) and was higher in the group with exercise of 3 times or more a week than in the group with no exercise at all (OR, 1.76; 95% CI, 1.43 to 2.18; P < 0.001). It was found that the significant difference in compliance depending on sex, educational level, smoking status, and drinking status which was shown in the univariate logistic regression analysis was no longer significant after adjusted for age, sex, and frequency of exercise (Table 2).
3. Relationship between Factors Related to Diseases and Compliance
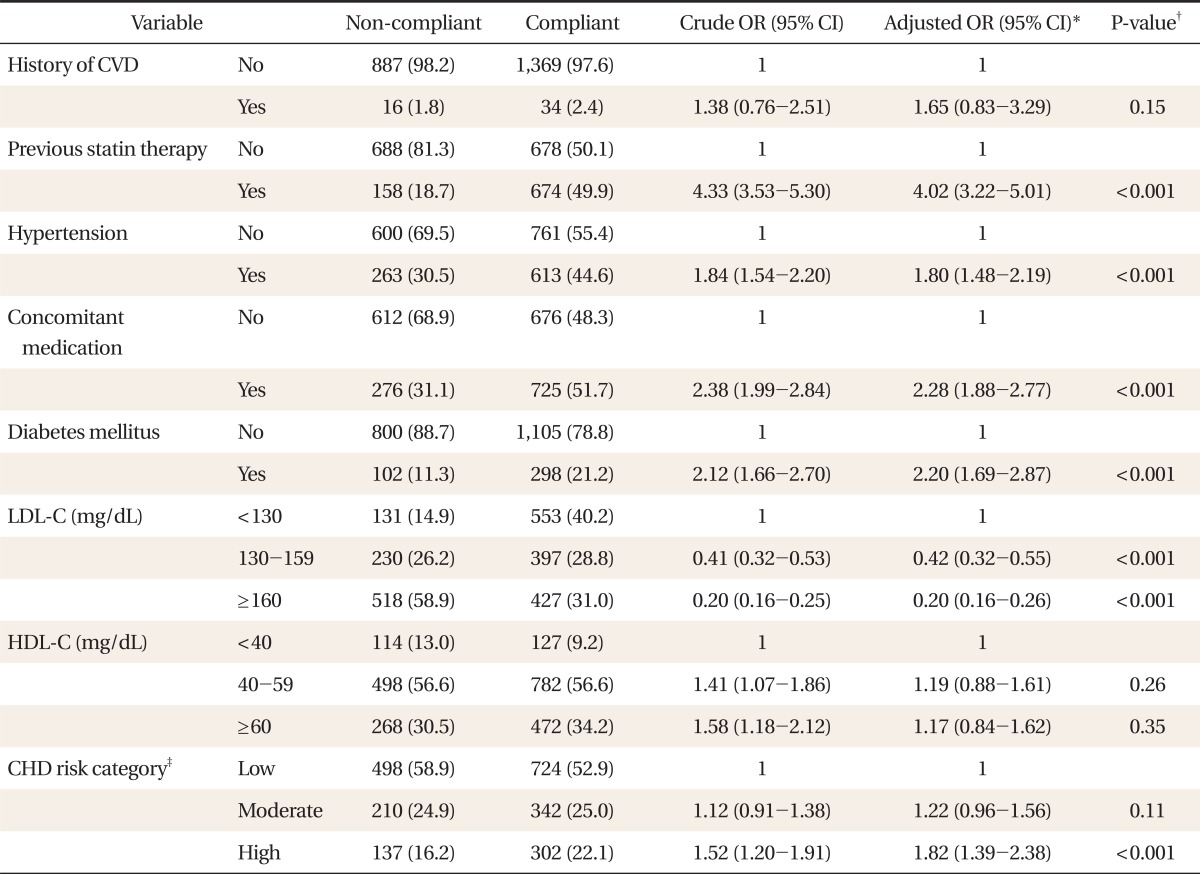
Previous statin use, hypertension, use of concomitant medication, and diabetes were associated with compliance (P < 0.001), and higher CVD risk showed higher compliance (P = 0.002). However, there was no difference in compliance when the participant had a history of cardiovascular diseases (P = 0.310).
In the multivariate logistic regression analysis which was performed by adjusting for age, sex, and frequency of exercise, the compliance was higher in cases where the patient had been taking statin previously (OR, 4.02; 95% CI, 3.22 to 5.01), where the patient had hypertension (OR, 1.80; 95% CI, 1.48 to 2.19), where there was a concomitant medication (OR, 2.28; 95% CI, 1.88 to 2.77) and where the patient had diabetes (OR, 2.20; 95% CI, 1.69 to 2.87), and in cases with higher CHD risk category (OR, 1.82; 95% CI, 1.39 to 2.38; P < 0.001). The compliance decreased in cases with a level of LDL cholesterol of 160 mg/dL or higher with OR of 0.20 than in the cases with that of less than 130 mg/dL (P < 0.001), and it was found that the level of HDL cholesterol, which had been significantly different in the univariate logistic regression analysis, was no longer significant after correction (Table 3).
DISCUSSION
This study investigated the compliance of patients receiving lipid lowering therapy at a primary care facility during a treatment period of 24 weeks and examined the factors related to the compliance. As a result of analysis, age, frequency of exercise, existence of hypertension and diabetes, presence or absence of concomitant medication, whether the patient had been taking statin previously, level of LDL cholesterol, and CHD risk category were the factors related to the compliance with lipid-lowering therapy.
The ratio of compliance in the present study was 54.1%, and similar results were shown in previous studies.8,12,17) The adherence was 72%, which was similar to results in the primary prevention clinical trial (69% to 71%)2) and lower than the results in the secondary prevention clinical trial (81% to 90%).8,9) The patients who had had a CVD previously were included in this study, but they occupied only 2.2%. Thus, previous CVD history might not have affected the compliance in this study.
The results of this study indicate that the greater the age of the patient, the greater the compliance; i.e., younger patients do not take statins diligently. Most previous studies also showed similar results.13,15,17) In our study, there was no difference in compliance according to sex, and this was similar with previous studies,8,12,13) but a few studies did report that women had a lower compliance.15) Patients who exercised more frequently had higher compliance and similar results were shown in other studies.13,17) This could mean that those who exercise more had more interest in health and better health behavior. Smoking was a factor of low compliance in other studies,13,17) but, in the present study, it was identified that there was no difference in compliance depending on smoking along with drinking status. As the ratio of women in the subjects of this study was 66.6%, which comes under two-thirds, and thus the smoking rate was 14.8% and the drinking rate was 31.9%, which were much lower than the average rates of Korean adults. Hence there is a possibility that this result was drawn due to selection bias.
The compliance was markedly higher in the group that had been taking statin previously than in the group that started taking statin for the first time (OR, 4.02). This was similar to results of previous studies,13,15,17) but there were also a few studies showing conflicting results.8) In our study, the compliance was significantly higher in participants with hypertension or diabetes, and there was no relationship in patients with CVD. In previous studies, the compliance was significantly higher in patients with hypertension, diabetes or cardiovascular diseases,12,15) and also there were several studies with no relationship.17) In our study, as participants with CVD occupied only 2.2% and most participants were mainly in primary prevention, CVD could not be related with compliance. In addition, compliance was significantly higher in participants with concomitant medications (OR, 2.28), and this was similar in previous studies.18) The reason for the low compliance in the group of patients taking rosuvastatin only may be that these patients had fewer effects of treatment or symptoms, and, they may lack the motivation for taking rosuvastatin regularly and the knowledge of chronic diseases.18)
In the present study, it was identified that the higher the level of LDL cholesterol, the lower the compliance. Several studies reported that the higher the total cholesterol before starting the treatment, the lower the compliance, but it was not statistically significant,13,17) and the relationship between the level of LDL cholesterol and the compliance has never been discussed. It is thought that the negative correlation with the compliance was shown in this study because when the CHD risk level is higher, the treatment is started at a lower level of LDL cholesterol. Actually, as a result of linear analysis between the LDL cholesterol and CHD risk category, the P-value was 0.014, showing a negative correlation. That is, the group with lower LDL cholesterol is the group with higher CHD risk level. It was found that the compliance was significantly higher when the CHD risk level was higher, and the two results coincide with each other.
There are several methods to measure compliance, which include examination of daily record, represcription rate, pill count, and electronic medication monitor.19) In this study, physicians checked the drug compliance, the continuance of rosuvastatin, and outpatient clinic visits during the follow-up period. Therefore, compliance would be measured better than that of other studies that examined only the continuance of treatment. However, as this study depended on the responses of patients for drug compliance, it may be influenced by the wrong reports of patients more than pill count or electronic medication monitor. However, our method is a cheap and easily used method which is actually used much in primary care, and thus it seems that there would be no great obstacle in the evaluation of compliance.
Another limitation is that the present study did not follow-up the compliance after 24 weeks. However, in starting the first drug treatment, changes in compliance is sharp within the first 6 months, and shows a mild decrease after that, and thus it can be seen that there is sufficient significance in the evaluation of compliance. This study targeted patients who visited the department of family medicine of hospitals, and thus it may be difficult to apply it to all the hypercholesterolemic patients in Korea. Despite these limitations, the present study demonstrates significance in that it identified the compliance of lipid lowering therapy in primary care with the main purpose of primary prevention and the factors influencing compliance.
In addition, this study added drug compliance to the evaluation of compliance, assessed the CHD risk category together, and investigated a large population. It is known that in order to increase compliance, various attempts should be integrated such as increasing the degree of participation of patients in treatment through various methods including education, self-monitoring using devices, reminding the patients to take the medicine, performing a telephone consultation, reminding by phone or letter, or prescribing to take the medicine once daily.20) As identified in this study, the compliance of patients without chronic diseases such as diabetes or hypertension was low and patients younger than 50 years receiving the single treatment of lipid lowering agent showed low compliance. Therefore, it is necessary to emphasize the importance of taking the lipid lowering agent and to conduct education on risks of CVDs. Moreover, drug compliance could be increased by life style modifications such as regular exercise and monitoring the patients through diverse approaches including telephone use.
In conclusion, 6 months after the start of treatment, about 50% of the patients continued the drug treatment, maintaining the drug compliance of 80% or more, and the factors related to higher compliance to lipid lowering therapy were old age, regular exercise, previous statin therapy, presence of concomitant medication, presence of hypertension or diabetes, and higher CHD risk level. The high LDL cholesterol is a factor related to lower compliance.
Notes
No potential conflict of interest relevant to this article was reported.