Effect of Sunlight Exposure on Serum 25-Hydroxyvitamin D Concentration in Women with Vitamin D Deficiency: Using Ambulatory Lux Meter and Sunlight Exposure Questionnaire
Article information
Abstract
Background
Vitamin D is an important factor in human health. Yet, vitamin D deficiency is very common. We aimed to confirm serum 25-hydroxyvitamin D (25OHD) concentration change after sunlight exposure and to elucidate the relationship between the amount of sunlight exposure and serum 25OHD level change by ambulatory lux meter and sunlight exposure questionnaire.
Methods
Twenty healthy young women were enrolled. They were educated to obtain 20 minutes of sunlight exposure during weekdays from October to November, 2010, during which they were to wear an ambulatory lux meter on an arm. All subjects completed a one-week recall sunlight exposure questionnaire at the end of the study. Before and after sunlight exposure, serum 25OHD level was measured.
Results
Mean pre-exposure serum 25OHD concentration was 11.01 ng/mL. The mean change of pre- and post-exposure 25OHD level was -0.62 ng/mL, but it was not statistically significant. The mean personal sunlight exposure recorded by ambulatory lux meter, 292.6 lux/s, showed no significant relationship with average change of 25OHD and average weekly sunlight exposure score, 11.9, calculated by the sunlight exposure questionnaire. However, the mean change of serum 25OHD level and weekly sunlight exposure score showed significant negative correlation (r = -0.469, P = 0.037).
Conclusion
Change of serum 25OHD concentration after four weeks of sunlight exposure was not statistically significant in women with vitamin D deficiency. However, serum 25OHD concentration change was significantly negatively correlated with the sunlight exposure score by the questionnaire.
INTRODUCTION
Vitamin D is a fat-soluble vitamin with various and important health benefits.1-3) Previous epidemiology studies have reported a very high prevalence of vitamin D deficiency, ranging from 40% to 90%.4-7) Decreased sunlight exposure can be a main cause of this phenomenon. The ultraviolet (UV) B portion of sunlight synthesizes vitamin D3 (cholecalciferol) from human skin, and it is a major source of human vitamin D.1) Therefore, appropriate sunlight exposure is an effective and costless method for prevention and treatment of vitamin D deficiency.
To evaluate appropriate sunlight exposure, a precise quantitative method of measurement is needed. But in South Korea, some previous studies about sunlight exposure used only self-reported questionnaires, and the questionnaires solicited responses only about outdoor activity time.6,8,9) Recently, a new sunlight exposure questionnaire was developed, which numerically measures both the exposed skin area and outdoor activity time.10) This questionnaire will be a more precise and useful tool than its predecessors.
As well, an ambulatory lux meter capable of measuring the intensity of exposed sunlight personally has been developed by a research team in Ajou University Ubiquitous System Research Center. The device, LifeSens, was originally developed as an ambulatory three-axis accelerometer for measurement of human physical activity. In one of several versions of this instrument, the lux meter was additionally applied to measure and record the intensity of personal sunlight exposure as lux per second. This allows the collection of various data about sunlight exposure, such as average sunlight exposure or sunlight exposure during specific hours.
In the present study conducted with Korean women, we aimed to confirm serum vitamin D level change after intentional sunlight exposure, and to elucidate the relationship between serum vitamin D level change and quantified estimation of the sunlight exposure, measured by ambulatory lux meter, and by the completion of a newly developed sunlight exposure questionnaire.
METHODS
1. Study Design and Subjects
This study was a single-center, observational clinical trial. Twenty women working in Ajou University Hospital Health Promotion Center in Suwon, Korea (latitude: 37°N) voluntarily agreed to participate. Exclusion criteria were patients with a condition that influenced vitamin D status, such as chronic liver disease, chronic renal disease or hypo/hyper-parathyroidism, use of vitamin D supplements due to osteoporosis or osteomalacia, high-risk of damage from sunlight exposure, such as history of skin cancer or cataract; and pregnancy or anticipated pregnancy.
The study period was four weeks, between October and November 2010. We tried to measure the exact period of time for significant change of serum 25-hydroxyvitamin D (25OHD) concentration, as a marker of vitamin D status, after sunlight exposure. Previous relevant data are scant, with one prior study showing an average 12 ng/mL increment of serum 25OHD concentration after four weeks of sunlight exposure.11) Likewise, the present study period was four weeks with the consideration of weather and study compliance.
All participants stayed outdoors for sunlight exposure for 20 minutes every weekday during mid-day (12:00 to 1:00 PM) except on days of rain. During the outdoor time, all subjects exposed their face and both forearms and hands to the sunlight. Wearing a hat, carrying an open parasol, and resting in the shade were not permitted. Sunblock application was permitted only for the face. Use of glasses and sunglasses was permitted. There were no interventions during the entire study period and there were no limitations on dietary intake. However, participants were recommended to avoid foods and products rich in vitamin D, such as salmon, mackerel, and cod, to minimize the effect of the dietary intake of vitamin D. In addition, the use vitamin D containing drugs or supplements was prohibited. All subjects provided their informed written consent. The institutional review board of Ajou University Hospital approved the study (AJUIRB-MED-OBS-10-198).
2. Data Collection
All participants were instructed to wear the ambulatory lux meter on their left arm during duty hours (Monday to Friday, 9:00 AM to 5:00 PM) for the entire four weeks of the study period. The total wearing time was 160 hours. Subsequently, each meter was collected and the data analyzed, especially focusing on average mid-day sunlight exposure.
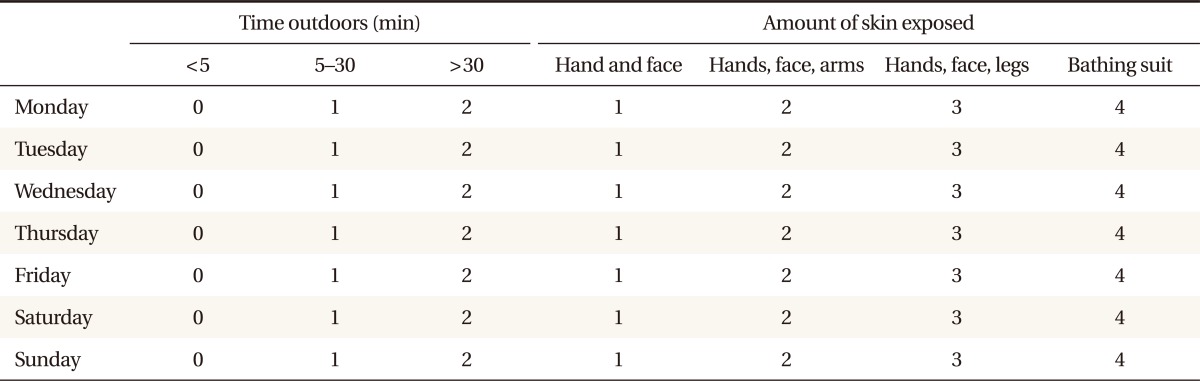
A pre-study questionnaire was completed and basic anthropometric measurements and blood test were conducted. The pre-study questionnaire, written in Korean, included residence, Fitzpatrick skin type,12) past history, social history, and history of use of vitamin D containing medications. The anthropometric measurements were conducted while each subject wore a light gown and no shoes, after an overnight fast. Height and weight were automatically measured to the nearest 0.1 cm and 0.1 kg, respectively. Body mass index (BMI) was calculated by dividing weight (kg) by height squared (m2). Waist circumference was measured with a flexible tape, at the level of the umbilicus, and was recorded to the nearest mm. Systolic blood pressure (BP) and diastolic BP were automatically measured with the subject in the sitting position after 10 minutes of rest. Body fat percentage was measured after the overnight fast using an Inbody 720 body composition estimator (Biospace, Seoul, Korea), which is based on bioelectrical impedence. Blood samples were also obtained after the same overnight fast for measurements of serum 25OHD, calcium, inorganic phosphorus, intact parathyroid hormone (PTH), and fasting glucose. A post-study questionnaire was administered, and BP measurement and blood testing were done. The post-study questionnaire, written in Korean, included the sunlight exposure questionnaire (Supplement 1). The original version of this questionnaire10) is an English version developed by researchers in Canada and Italy. The Korean version was presently created by the authors. The questionnaire scored the amount of time spent outdoors each day on a 0 to 2 scale (0, ≤5 minutes; 1, 5-30 minutes; 2, ≥30 minutes). Also, responses were solicited on a 0 to 4 scale to four questions about clothing-related skin exposure while outdoors (1, face and hands only; 2, face, hands, and arms; 3, face, hands, and legs; 4, 'bathing suit'; the latter indicating exposure of almost the entire body). The estimated score of mean weekly sun exposure was calculated as the amount of time spent outdoors and the amount of skin exposed was calculated for each day to create a daily sunlight exposure score on a scale ranging from 0 to 8, with 0 being minimum and 8 being maximum. The sunlight exposure scores of all seven days were summed to equal the weekly sunlight exposure score, with a possible range from a minimum of 0 to a maximum of 56. Post-study BP measurements and blood tests were performed as in the pre-study.
3. Statistical Analyses
Descriptive statistics and frequency analysis were performed to describe the baseline characteristics of the study subjects. A one-sample Kolmogorov-Smirnov test was used for normality testing of all continuous variables. Through the test, all continuous variables were normally distributed. To compare baseline and post-exposure variables, a paired t-test was used. To elucidate relationship between personal sunlight exposure, weekly sunlight exposure score and mean of serum 25OHD concentration change, Pearson's correlation test was performed. Additionally, baseline (or post-study) serum 25OHD concentrations and other baseline (or post-study) variables were analyzed by Pearson's correlation test. All statistical analyses were two-tailed, and a P-value < 0.05 was considered statistically significant. Data were analyzed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
1. Baseline Characteristics
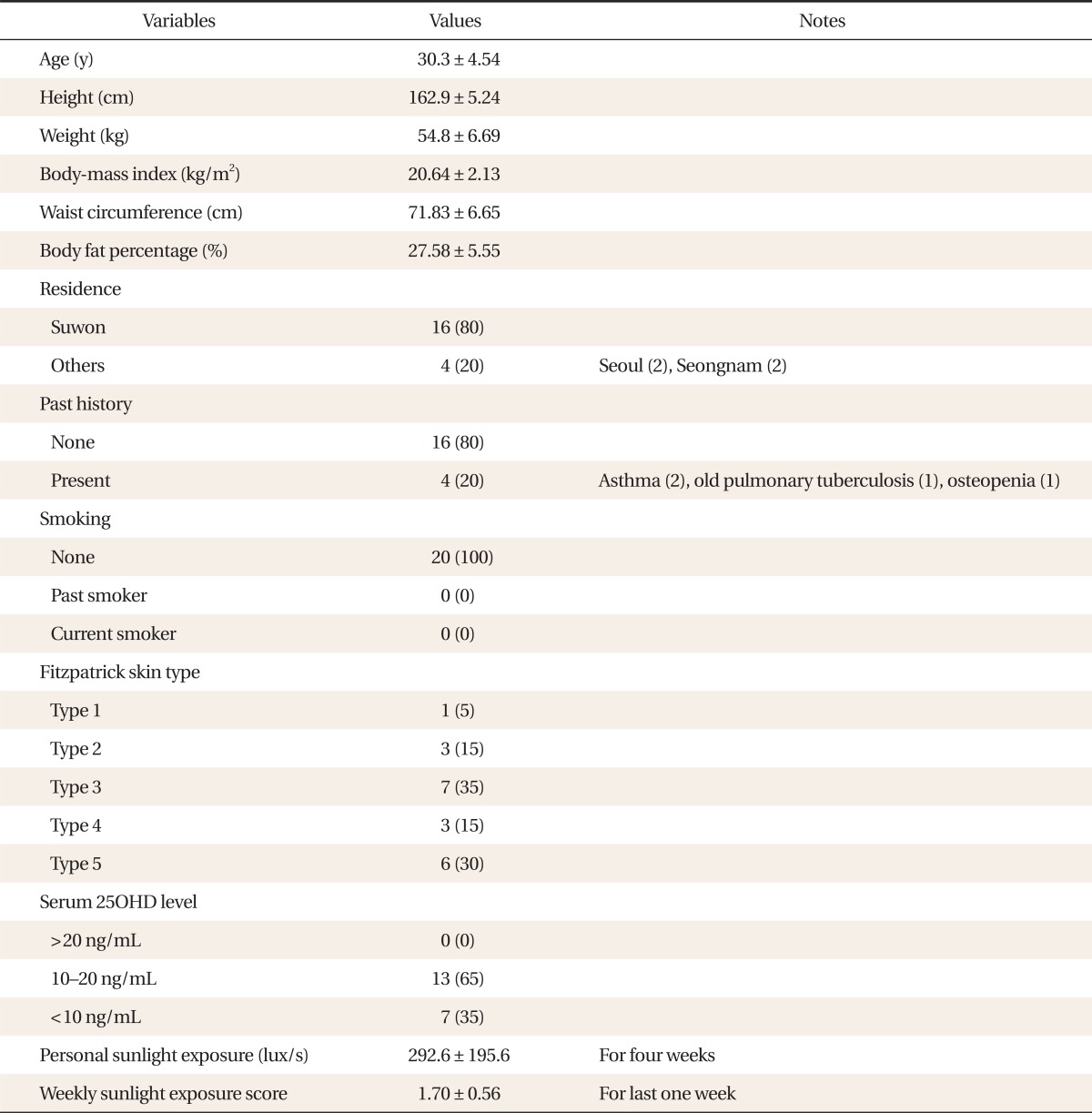
Table 1 summarizes baseline characteristics of the study population. Mean age of the study subjects was 30 years, and mean anthropometric results stayed within the normal range for height (162.9 cm), body weight (54.8 kg), BMI (20.6 kg/m2), and waist circumference (71.8 cm). Average baseline serum 25OHD concentration was 11.01 ng/mL and no subject had a 25OHD level exceeding 20 ng/mL. Thirteen subjects (65% of total) had a 25OHD level of 10 to 20 ng/mL and the level in seven subjects (35% of total) was <10 ng/mL. Therefore, all study subjects were in vitamin D deficiency status. Personal sunlight exposure, measured by ambulatory lux meter at mid-day (12:00 PM to 1:00 PM) during the study period, was 292.6 lux/s. Weekly sunlight exposure score, calculated by the sunlight exposure questionnaire, was 1.70 (1.64 for weekdays, 1.85 for weekend) (Table 1). Other baseline variables, such as body fat percentage, blood pressure, serum calcium, inorganic phosphorus, intact PTH, and fasting glucose, stayed within normal limits (Tables 1, 2).
2. Comparison of Pre- and Post-study Variables
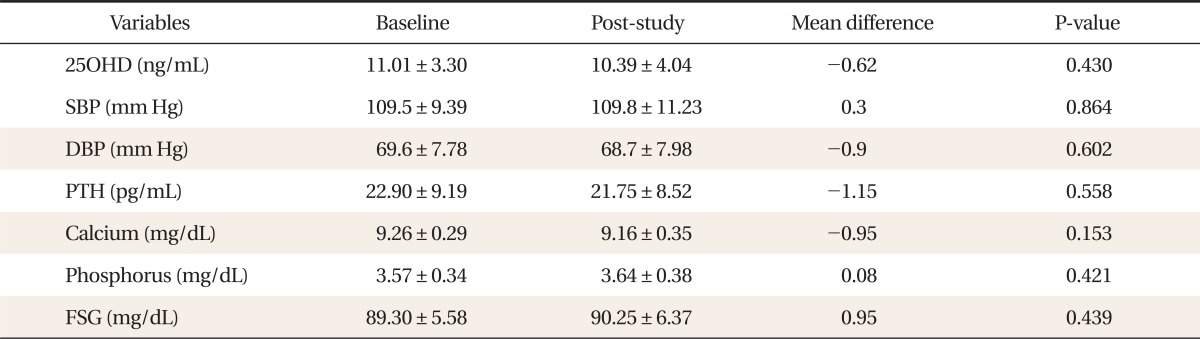
After four weeks, the mean serum 25OHD level of study subjects was 10.39 ng/mL. It was 0.62 ng/mL lower than that of the baseline. However, the difference was not statistically significant by the paired t-test (P = 0.430). In addition, other variables, such as BP, intact PTH, serum calcium, inorganic phosphorus, and fasting glucose, showed no significant differences between pre- and post-study values (Table 2).
3. Correlations between Personal Sunlight Exposure, Weekly Sunlight Exposure Score and Mean Serum 25OHD Concentration Change
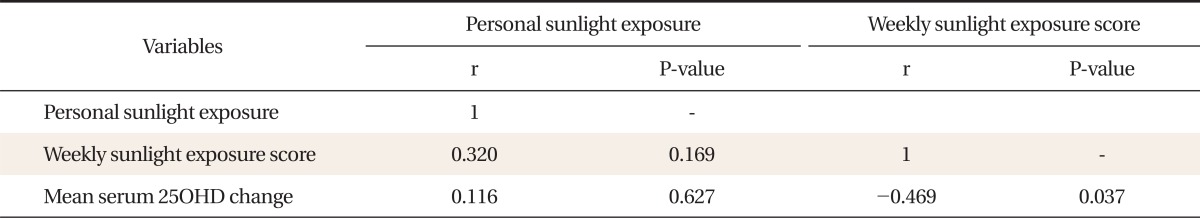
There was no significant relationship between personal sunlight exposure and weekly sunlight exposure score, and between personal sunlight exposure and mean serum 25OHD level change. Weekly sunlight exposure score and mean serum 25OHD concentration change, however, showed significant negative correlations (r = -0.469, P = 0.037). The value of mean serum 25OHD level change was negative (-0.62 ng/mL), which may mean that the subjects with higher weekly sunlight exposure score showed lower decline of serum 25OHD levels during the study period (Table 3).
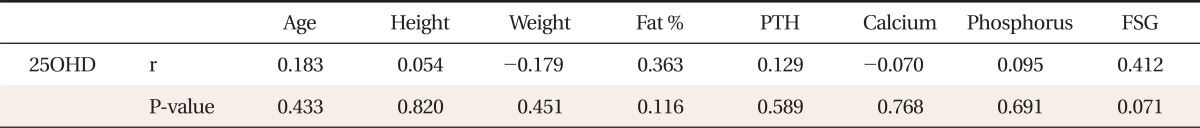
4. Correlations between Pre- and Post-serum 25OHD Concentration and Other Variables
Baseline serum 25OHD concentration and other baseline variables such as age, height, weight, BMI, waist circumference, body fat percentage, BP, intact PTH, serum calcium, inorganic phosphorus, and fasting glucose showed no significant relationship (Table 4). In addition, post-study serum 25OHD concentration was not correlated with weekly sunlight exposure score (r = 0.092, P = 0.701) and personal sunlight exposure (r = -0.397, P = 0.083).
DISCUSSION
Our study aimed to confirm serum vitamin D level change after intentional sunlight exposure, and to elucidate the relationship between serum vitamin D level change and quantified estimation of sunlight exposure, measured by the ambulatory lux meter and the novel sunlight exposure questionnaire. After intentional sunlight exposure for four weeks, there was no significant change of serum vitamin D levels in the study period. In addition, personal sunlight exposure, measured using the ambulatory lux meter, was not significantly related with a serum vitamin D level change and the sunlight exposure score measured by sunlight exposure questionnaire. Serum 25OHD concentration change and the sunlight exposure score, however, were significantly correlated with each other. Therefore, there was a different relationship according to the measuring method.
A variety of recent studies have been conducted to address the various health benefits of vitamin D. Vitamin D is associated with osteoporosis and osteoporotic fracture,1-3) colon cancer,13) breast cancer,14) and total cancer incidence,15) total mortality,16) cardiovascular disease,17) fall,18) type 1 and 2 diabetes mellitus,19,20) multiple sclerosis,21) rheumatoid arthritis,22) and systemic lupus erythematosus.23) Nonetheless, the incidence of vitamin D deficiency is very high. In the United States, studies have reported vitamin D deficiency in 36% of healthy young adults in Boston during winter4) and in 57% of inpatients of Massachusetts General Hospital.5) In Korea, vitamin D deficiency was reported in 72% of premenopausal women in Busan during winter6) and in 92% of postmenopausal women in Seoul, also during winter.7) In our study, results consistent with these previous studies were found; the mean 25OHD level of the study population was 11.01 ng/mg and all study subjects had vitamin D deficiency. However, the definition of vitamin D deficiency is still controversial. Vitamin D deficiency is diagnosed by serum 25OHD concentration.1) Recent studies reported that the appropriate serum 25OHD level exceeded 30 ng/mL and the US Institute of Medicine recommended maintaining the level over 20 ng/mL.1,24) In Korea, there have been no reports concerning a definite cut-off value of serum vitamin D concentration, although some studies described a mean serum vitamin D level. According to the 4th Korea National Health and Nutrition Examination Survey (2007-2009), the mean serum 25OHD level of 1,613 premenopausal women was 17.2 ± 6.3 ng/mL,25) and that of 2,878 women who had a medical check-up at a university hospital during the autumn was 19.1 ng/mL.26)
High incidence of vitamin D deficiency is strongly related with low exposure to sunlight. Photo-synthesized vitamin D3 in the skin is a major source of human vitamin D, about 90%.1,2) Since the 1980s, the use of sunblock and other UV-based protection methods have been widely used due to the risk of skin cancer and photoaging. Furthermore, the shift in many occupations from outdoor activities (such as farming and fishing) to indoor activities (service- and information) has decreased sunlight exposure time during work. Increased use of public transportation has also limited outdoor activity time. In addition, increased air pollution in urban centers blocks UV radiation, decreasing vitamin D photosynthesis. There is still no published guideline regarding sunlight exposure for prevention and treatment of vitamin D deficiency, because many factors are associated with photosynthesis of vitamin D. Weather, latitude, altitude, air pollution, age, exposed skin area, and use of sunblock may influence vitamin D synthesis in human skin.27)
In the current study, personal sunlight exposure measured by ambulatory lux meter showed no significant relationship with vitamin D level change. There are several possible reasons. First, low study compliance due to cold weather can be presumed. The average temperature during November 2010 in Korea was 7.1℃, which may coincide with limited sunlight exposure. Second, we measured lux, not UV dose, because of a technical problem (the UV meter is more complex, with no versions of a UV meter-assembled device). Sunshine and UV radiation have been strongly positively correlated,28) but there were no direct data concerning the relationship between lux and UV dose in our ambulatory lux meter measurements. In addition, indoor illumination can be measured by an ambulatory lux meter. So, there may have been a difference between actual UV exposure and measured lux. Third, we were unable to measure sunlight exposure during the weekend. Generally, office workers may spend more time outdoors during the weekend than on weekdays. Fourth, we cannot control for pre-study sunlight exposure. Time for serum vitamin D concentration change after sunlight exposure is required, so pre-study sunlight exposure could have been a confounder to the study results. Small numbers and vitamin D deficient condition of the study subjects might be limitations. The study population showed various Fitzpatrick skin types. The relationship between Fitzpatrick skin type and vitamin D photosynthesis remains controversial.29,30) However, recently, negative results have been published, so the authors did not adjust skin type at analysis. We cannot confirm the relationship between sunlight exposure and serum 25OHD level. A follow-up study is required with more numbers of study subjects and longer study period during the summer.
Nonetheless, we used a previously-described self-reported sunlight exposure questionnaire.10) This new questionnaire31) has some stronger points than previous questionnaires: it is simple, uses both exposed skin area and outdoor activity time, and expresses sunlight exposure numerically. The results of this new questionnaire showed a significant positive correlation with the serum vitamin D level of healthy adults in the summer in southern Italy (r = 0.59, P = 0.003). The questionnaire also showed a significant correlation with serum vitamin D concentration change of vitamin D deficient women during the autumn in South Korea. In addition, our study has some strong points. First, this research is the first clinical trial that used an ambulatory lux meter. Second, this is the first study in Korea to evaluate the relationship between quantitative measurement of sunlight exposure and serum vitamin D concentration. Third, this study showed the clinical significance of the new sunlight exposure questionnaire in Korean women.
In conclusion, serum vitamin D concentration significantly correlated with the score of the sunlight exposure questionnaire, but was not associated with ambulatory lux meter results. Therefore, there is a possibility of a different relationship according to the measuring method. For more definite results and the clinical use of these tools, a well-designed follow-up study is needed.
ACKNOWLEDGMENTS
Authors thank Sanofi-Aventis Korea for research funding. We also thank Na-Ri Shin, a dietitian in Ajou University Hospital Nutrition Team for data collection, and Min-Young Jung, a registered nurse in Seoul Asan Medical Center for helping reference search.
Notes
No potential conflict of interest relevant to this article was reported.