|
 |
- Search
| Korean J Fam Med > Volume 33(1); 2012 > Article |
Abstract
Background
It is important to know and decide when to end regimen for the quality of life of the patients. However, there is currently no clear agreement on when to terminate palliative chemotherapy. We investigated the duration between the last chemotherapy and death, and associated factors affecting patients receiving palliative care after the last chemotherapy.
Methods
We studied 242 patients who were put into palliative care ward after receiving chemotherapy and died during hospitalization from 2008 to 2009. Electronic medical records were used to gather information on demographic characteristics, types of primary cancer, and palliative chemotherapy. Then we analyzed the relationship between the clinical characteristics of patients and interval between last chemotherapy and death.
Results
The average survival time of patients after referral to palliative care was 17.5 days; survival time after discontinuation of chemotherapy was 103 days. Also, 104 (43.0%) patients died within 3 months and 14 (5.8%) patients died within 1 month of persistent palliative chemotherapy. Chemotherapy on patients within 3 months from their death was not associated with the social characteristics of the population.
Conclusion
The patients who were referred to palliative care were found to have continued to receive chemotherapy within 3 months before death. However, only a small number of patients received chemotherapy within 1 month before death, which confirms that futile chemotherapy that extends to the end of life was less frequent. Doctors should be able to recognize the implications of excessive and aggressive use of chemotherapy and should actively communicate with patients about therapeutic choices.
The incidence of cancer in Korea has increased 3% per year from 1999 to 2007. About 160,000 new cancer cases occur every year and mortality rate exceeds 140 per 100,000 people.1) Due to ongoing development of new 'less toxic thus well tolerated' drugs, anti-cancer chemotherapy until the end-of-life is gradually increasing.2) However, an excessive chemotherapy can decrease the quality of life of patients. Therefore doctors should consider gain and loss of chemotherapy administered to terminally ill patients in the palliative care ward; whether to enforce appropriate chemotherapy in a purpose of treating patients in palliative care ward need to be discussed.3,4)
Thus it is important to know and decide when to end regimen for the quality of life of the patients. However, there is currently no clear agreement on when to terminate palliative chemotherapy. We therefore investigated the duration between the last chemotherapy and death, and associated factors affecting patients receiving palliative care after the last chemotherapy.
Subjects of this study are 309 patients who died during hospitalization in the palliative care ward in Samsung Medical Center from January 1, 2008 to May 31, 2009. Among these patients, 67 patients were excluded due to following reasons: 2 patients were non-cancer terminal illness, 62 patients never received anti-cancer chemotherapy since diagnosis of cancer and 3 patents has been initially registered in the palliative care ward then re-treated with anti-cancer chemotherapy. Thus electronic medical records of 242 patients have been studied in this investigation. These patients had been treated with anti-cancer chemotherapy more than once before referral to palliative care unit.
Throughout the retrospective investigation of electronic medical records, demographic characteristics such as age, sex and level of education were obtained along with the type of cancer, metastatic site, date of palliative care registration, Eastern Cooperative Oncology Group (ECOG) performance status upon the last hospitalization, date of death, number of palliative chemotherapy regimen, and the start and end date of the last chemotherapy regimen. We defined palliative chemotherapy as chemotherapy of which purpose is not to cure cancer but to relieve symptoms or to prolong life. End of chemotherapy is defined as the last administration of anti-cancer drug. The period between the end of chemotherapy and death was calculated as the number of days.
ECOG performance is a tool to evaluate performance status of cancer patients. It is appraised in six grades: grade 0 (fully active), grade 1 (restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature), grade 2 (ambulatory and capable of all self-care but unable to carry out any work activities. Up about more than 50% of waking hours), grade 3 (capable of only limited self-care; confined to bed or chair 50% or more of waking hours), grade 4 (completely disabled; cannot carry on any self-care; totally confined to bed or chair), grade 5 (death).
To find out relationship between survival time since the last palliative chemotherapy and patient characteristics, t-test was used for parametric test and Mann-Whitney test was used for non-parametric test. To validate univariate analysis between groups according to the length of survival, chi-square test and Fisher's exact test were used. PASW (old: SPSS) ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used to analyze data. Two-tailed test were done and significance level was set for 0.05.
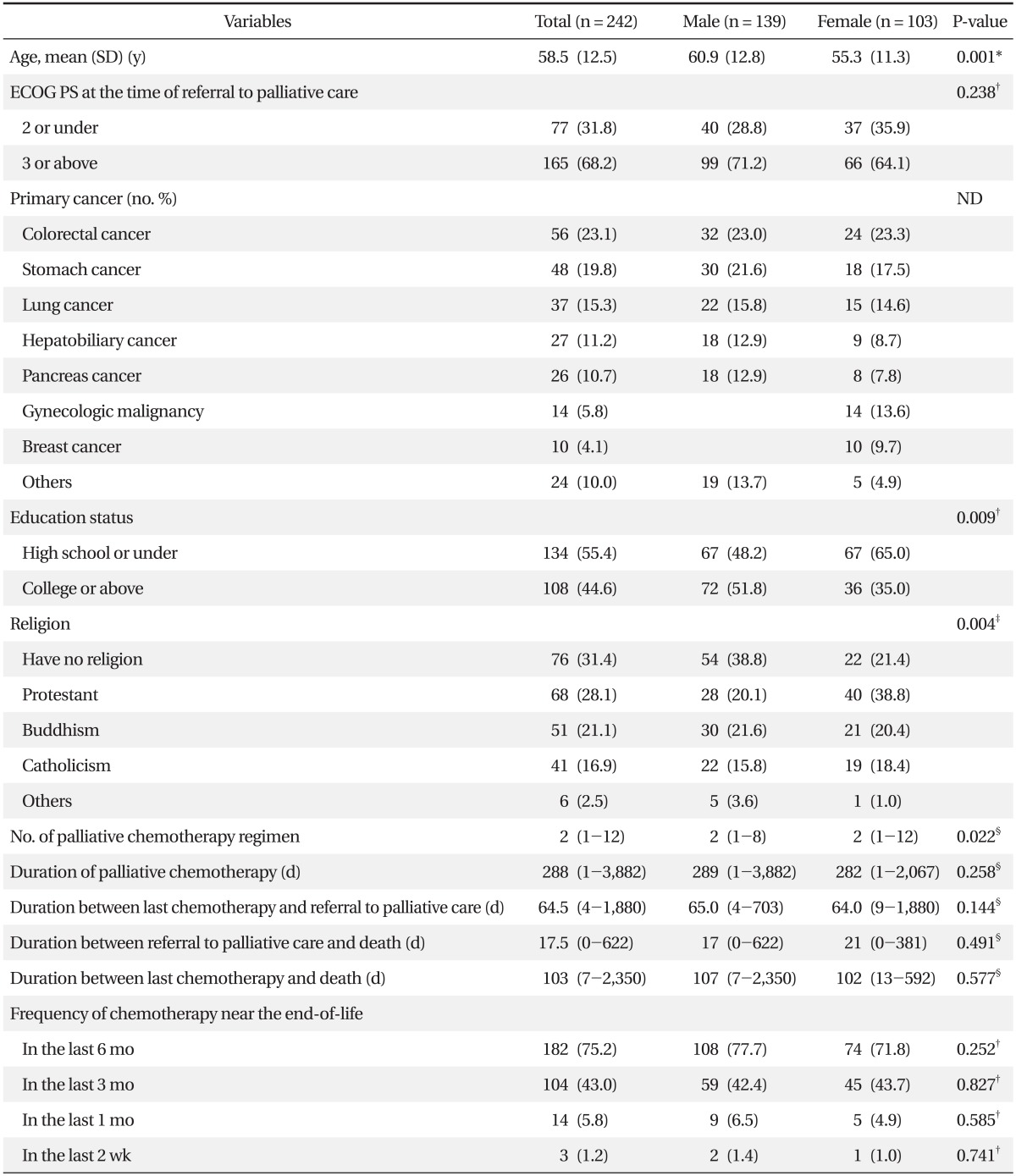
Mean age of the study subjects was 58.5 (┬▒ 12.5) years. Median days from the end of chemotherapy to registration of palliative care were 64.5 days. Survival time after registration in palliative care was 17.5 days and survival time after the end of chemotherapy was 103 days. There were significant differences between male and female in the number of palliative chemotherapy regimen, level of education, and religion. However there were no significant differences between male and female in length of palliative chemotherapy, period from the end of chemotherapy to the date of registration in palliative care, ECOG performance at the time of registration in palliative care, survival time after the end of chemotherapy and length of survival after registration in palliative care. The highest number of patients suffered from gastrointestinal cancers including colorectal and stomach, which were 104 patients (43%), followed by 37 lung cancer patients (15.3%), 27 hepatobilliary cancer patients (11.2%) and 26 pancreatic cancer patients (10.7%) (Table 1). Three patients (1.2%) were treated with anti-cancer chemotherapy within two weeks before death, 14 patients (5.8%) within one month, 104 patients (43.0%) within three months and a new regimen of anti-cancer drug was administered to a total of 56 patients (23.1%) within three months before death.
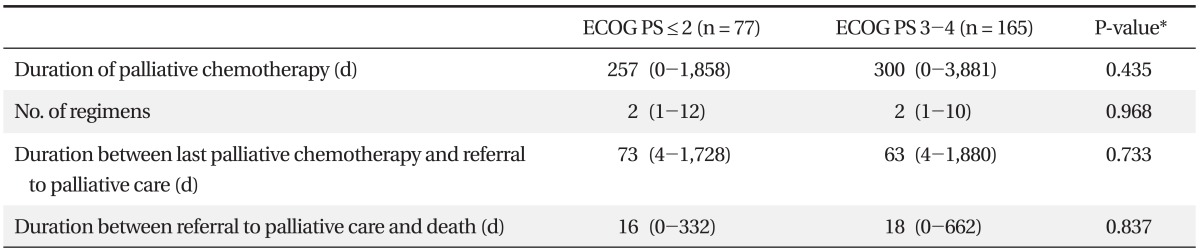
We analyzed the difference of survival duration after the last chemotherapy by the patients' characteristics. There were no significant differences of survival duration in age, sex, religion, level of education, number of chemotherapy regimen, and type of cancer between the group who survived more than 90 days and the group who survived less than 90 days. However, 24 patients (23.1%) in the group who survived more than 90 days and 53 patients (38.3%) in the group who survived less than 90 days had ECOG performance grade 2 or under on the day of registration at palliative care (Žć2 = 6.42, P = 0.011) (Table 2). This finding suggested that the patients having more survival duration had a relatively better performance status, but there were no significant differences between better performance status group (ECOG 2 or under) and poor performance status group (ECOG 3 or above) in terms of duration of palliative chemotherapy, number of chemotherapy regimen, duration from the last chemotherapy to referral to palliative care and survival duration after referral (Table 3).
We found that 43% of terminally ill patients have received chemotherapy within three months before death and 23% started new regimen of chemotherapy within three months before death. These findings were similar to the other previous studies. Several studies have discussed chemotherapy near the end of life. Earle and the colleagues reported that 11.6% of 210,000 patients had received chemotherapy within two weeks before death5) and Kao et al found that 8% and 18% of 750 terminally ill cancer patients had received chemotherapy within 2 weeks and 4 weeks before death, respectively.6) In Korea, a retrospective multicenter study showed that 43.9% and 30.9% of 3,750 patients had received chemotherapy within three and one month before death, respectively.7) Another study by a tertiary care hospital in Seoul showed that 50.3% and 5.7% of 298 patients had received chemotherapy within 2 months and 2 weeks before death, respectively.8) However, our study showed that 1.2% of patients received chemotherapy within two weeks before death and 5.8% within one month before death, compared with the other study showing up to 20% of patients did so within 2 weeks before death.9) This difference may be explained by the fact that our patients were referred to palliative care center thus treated less aggressively,7,10) but the patients from other studies might not have an access to palliative care. We found that the patients referred to palliative care had few futile chemotherapy near the end of life. However, it remains to be confirmed whether this finding had some impact on improved survival or quality of life of patients.
The previous studies showed various relationships between patient's factors and persistent chemotherapy near the end of life and differed by socio-cultural conditions. Patients who were older, female, and had an access to palliative care, received less aggressive chemotherapy.2) Married patients received less aggressive chemotherapy than unmarried patients.5) Patients who were younger and had chemotherapy-sensitive tumors such as gastrointestinal cancer, received more aggressive chemotherapy. However, men rather than women received less aggressive chemotherapy.6) Patients, who were symptomatic, under the age of 45 and were not referred to palliative care, were likely to continue receiving chemotherapy.10) College graduate chose less aggressive treatment near the end of life in a study carried out in Korea,7) but there were no relationship between educational level and choice of chemotherapy in terminally ill cancer patients in a study done in Netherlands.11)
In this study, we could not find any association between chemotherapy near the end of life and many patient factors such as age, sex, religion, level of education, site of cancer and socio-demographic factors only except performance status at the time of registration in palliative care. This could be explained by a small sample size. There were only 14 patients who underwent chemotherapy during the last month of life and the number of events was too small to find the related factors. Another explanation is that the patients of our study already opted for palliative care. Selection of palliative care can be a strong factor to deny chemotherapy near the end of life. It is also consistent with a previous study on patients with metastatic cancer, which showed that patients considering a quality of life were likely to receive fewer chemotherapy and getting chemotherapy had no significant association with gender, age, and level of education.11)
We could not analyze the effect of physician factors on chemotherapy near the end of life, but the role of physician is important in doing aggressive chemotherapy until the end of life in Korea, considering that referral to palliative care is mostly done when there are no further chemotherapy options available.12) One study reported that doctors felt uncomfortable in offering palliative care to advanced cancer patients but felt easier in discussing another chemotherapy options.13) Also a study on 95 incurable advanced cancer patients showed that only 39% of patients were told of their prognosis by their physician even though they were already getting palliative chemotherapy.14) As physician's lack of effort to communicate with patients can cause futile chemotherapy near the end of life, further study is needed on the association of physician factors with chemotherapy near the end of life.
It is difficult to generalize our findings as this was a retrospective study conducted at a single tertiary hospital. Another limitation of this study is that impact of chemotherapy near the end of life on the quality of life cannot be evaluated directly. However, several studies have already reported that there was more harm in doing chemotherapy near the end of life.3,4) Also we could not obtain objective data on purpose and effectiveness of palliative chemotherapy as wells as reason for starting or continuation of chemotherapy, thus it was impossible to assess whether the chemotherapy were appropriate or excessive.
Nevertheless, this study has advantages as it examined patients receiving palliative care and discussed differences with other existing studies. The existing studies reported that availability of palliative care2) or providing information on palliative care10) played an important role in patient's decision-making on treatment and reduced likelihood of receiving aggressive chemotherapy. Thus it is thought to be meaningful to find out current situation of chemotherapy near the end of life among the patients at palliative care unit.
In conclusion, authors found there was no difference on administration of chemotherapy within 3 months before death between palliative care group in this study and usual care group from other studies. However, less chemotherapy were administered to the patients within one month before death in this study. It is postulated that earlier referral to palliative care would add survival duration without aggressive chemotherapy and thus improve patient's quality of life. Effectiveness of palliative care should be confirmed in randomized controlled study comparing survival and quality of life among incurable advanced cancer patients undergoing palliative chemotherapy with or without palliative care service. In addition, awareness and attitude of each patient are more important than socio-demographic characteristics in decision-making of chemotherapy near the end of life and this can be affected by proper communication between heath care professionals and patients regarding to purpose, benefits and harms of treatment. This also suggests a need for future study to identify a relationship of proper communication and patient's quality of life.
References
1. Cancer statics [Internet]. National Cancer Information Center. c2011. [cited 2010 May 20]. Seoul: National Cancer Information Center; Available from: http://www.cancer.go.kr/cms/statics
2. Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, Weeks JC. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol 2004;22:315-321. PMID: 14722041.


3. Borras JM, Sanchez-Hernandez A, Navarro M, Martinez M, Mendez E, Ponton JL, et al. Compliance, satisfaction, and quality of life of patients with colorectal cancer receiving home chemotherapy or outpatient treatment: a randomised controlled trial. BMJ 2001;322:826PMID: 11290635.



4. Harrington SE, Smith TJ. The role of chemotherapy at the end of life: "when is enough, enough?". JAMA 2008;299:2667-2678. PMID: 18544726.



5. Earle CC, Landrum MB, Souza JM, Neville BA, Weeks JC, Ayanian JZ. Aggressiveness of cancer care near the end of life: is it a quality-of-care issue? J Clin Oncol 2008;26:3860-3866. PMID: 18688053.



6. Kao S, Shafiq J, Vardy J, Adams D. Use of chemotherapy at end of life in oncology patients. Ann Oncol 2009;20:1555-1559. PMID: 19468033.


7. Yun YH, Kwak M, Park SM, Kim S, Choi JS, Lim HY, et al. Chemotherapy use and associated factors among cancer patients near the end of life. Oncology 2007;72:164-171. PMID: 18097167.


8. Keam B, Oh DY, Lee SH, Kim DW, Kim MR, Im SA, et al. Aggressiveness of cancer-care near the end-of-life in Korea. Jpn J Clin Oncol 2008;38:381-386. PMID: 18411260.


9. Murillo JR Jr, Koeller J. Chemotherapy given near the end of life by community oncologists for advanced non-small cell lung cancer. Oncologist 2006;11:1095-1099. PMID: 17110629.


10. Hashimoto K, Yonemori K, Katsumata N, Hotchi M, Kouno T, Shimizu C, et al. Factors that affect the duration of the interval between the completion of palliative chemotherapy and death. Oncologist 2009;14:752-759. PMID: 19596665.


11. Koedoot CG, de Haan RJ, Stiggelbout AM, Stalmeier PF, de Graeff A, Bakker PJ, et al. Palliative chemotherapy or best supportive care? A prospective study explaining patients' treatment preference and choice. Br J Cancer 2003;89:2219-2226. PMID: 14676798.



12. Moon DH, Lee MA, Koh SJ, Choi YS, Kim SH, Yeom CH. Doctor's attitudes toward hospice and palliative care for terminal cancer patients. Korean J Hosp Palliat Care 2006;9:93-100.
14. Koedoot CG, Oort FJ, de Haan RJ, Bakker PJ, de Graeff A, de Haes JC. The content and amount of information given by medical oncologists when telling patients with advanced cancer what their treatment options are: palliative chemotherapy and watchful-waiting. Eur J Cancer 2004;40:225-235. PMID: 14728937.