|
 |
- Search
| Korean J Fam Med > Volume 35(5); 2014 > Article |
Abstract
Background
Although it is known that losing weight has an effect on the treatment of non-alcoholic fatty liver disease, the studies that show how losing weight affects the non-alcoholic fatty liver disease for the normal weight male adults are limited so far. In this study, we set body mass index as criteria and investigated how the weight changes for 4 years makes an impact on the risk of non-alcoholic fatty liver disease for the male adults who have the normal body mass index.
Methods
From January to December of 2004, among the normal weight male adults who had general check-up at the Health Promotion Center of Ulsan University Hospital, 180 people (average age, 47.4 ┬▒ 4.61 years) who were diagnosed with fatty liver through abdominal ultrasonography were included in this study and were observed according to the variety of data and ultrasonography after 4 years (2008). People who had a history of drinking more than 140 g of alcohol per week or who had a past medical history were excluded from the analysis. The weight change of subjects was calculated using the formula 'weight change = weight of 2008 (kg) - weight of 2004 (kg)' and classified into three groups, loss group (Ōēż-3.0 kg), stable group (-2.9 to 2.9 kg), and gain group (Ōēź3.0 kg). The odds for disappearance of non-alcoholic fatty liver disease in those three different groups were compared.
Results
Among 180 subjects, compared with stable group (67.2%, 121 subjects), loss group (11.7%, 21 subjects) showed 18.37-fold increase in the odds of disappearance of non-alcoholic fatty liver disease (95% confidence interval [CI], 4.34 to 77.80) and gain group (21.1%, 38 subjects) showed 0.28-fold decrease in the odds of disappearance of non-alcoholic fatty liver disease (95% CI, 0.10 to 0.83).
Non-alcoholic fatty liver disease (NAFLD) indicates a wide range of liver diseases from simple steatosis of patients who do not have any alcoholic abuse history to non-alcoholic steatohepatitis, which generates inflammation and necrosis, hepatic fibrosis, and liver cirrhosis.1,2)
Metabolic syndrome and insulin resistance syndrome are known as important causes of NAFLD.3,4) Treatments include improving metabolic syndrome such as obesity, insulin resistance, diabetes and hyperlipidemia, healing oxidative stress, and other treatment including liver protective material. However, clear treatment methods for NAFLD have not been discovered yet and controlling weight is being proposed.5) Occurrence of NAFLD is increasing along with the number of overweight people. The importance of NAFLD is receiving greater recognition because fatty liver resulting from obesity may lead to further fibrosis, which can cause liver cirrhosis, loss of liver function and even hepatocellular carcinoma.4)
Regarding the cure for NAFLD in overweight people, there are many studies reporting that exercise or losing weight are important and actually improve histology.5,6,7,8) It is being reported that losing weight from 0.5 to 1 kg per week is effective for treating NAFLD in overweight patients.9) However, whether losing weight is effective or not for treating NAFLD in non-overweight patients is not clear. Further, compared to western people, Asian people have a higher prevalence rate of abdominal obesity despite the fact that relatively lower body mass index (BMI) and abdominal obesity related to insulin resistance are more dangerous factors;10) thus examination of NAFLD for not-overweight patients is very meaningful for Asian people including Koreans. To investigate the impact of weight changes in NAFLD patients of normal weight, authors analyzed the relationship between four-year-weight changes and NAFLD, targeting people of normal weight who had medical checkup.
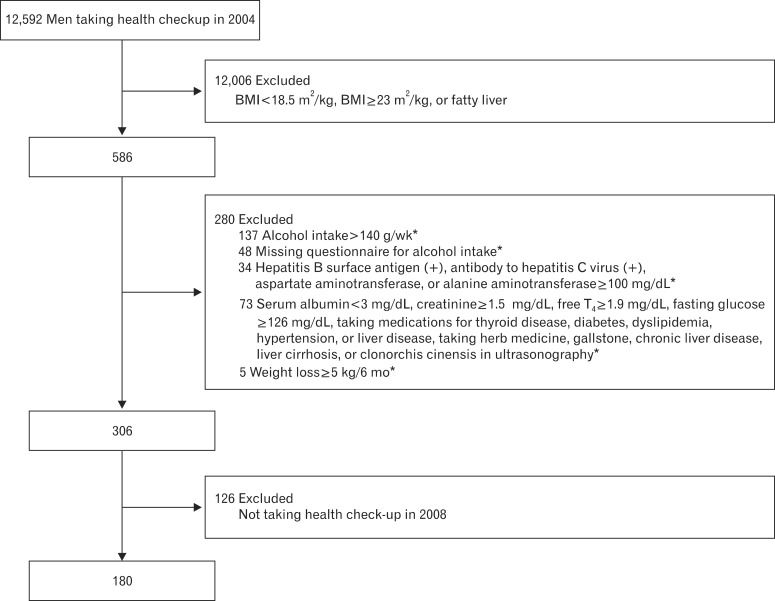
Twelve thousand five hundred and ninety-two male adults aged 19 to 84 years who had a medical checkup at Ulsan University Health Promotion Center from January 2004 to December 2004 were studied. Among the subjects, the number of people whose BMI stayed in a normal range (18.5 to 22.9 kg/m2) and ultrasonography shows fatty liver opinion was 586. Among those people, 137 people who have drinking history more than 140 g per week, 48 people who did not answer alcohol questionnaire, 27 people who had been diagnosed as positive to hepatitis B surface antigen or antibody to hepatitis C virus, 7 people whose aspartate aminotransferase (AST) or alanine aminotransferase (ALT) are 100 IU/L and above, 2 people whose serum albumins was lower than 3.0 g/dL and creatinine were more than 1.5 mg/dL, 10 people who had clinical thyroid dysfunction, 35 people who had been diagnosed with clinical diabetes, 17 people who were taking (oriental) medicine due to thyroid disease, diabetes, hyperlipidemia, blood pressure, and liver disease, 9 people who were diagnosed with gallstone disease, chronic liver disease, cirrhosis, clonorchiasis through abdominal ultrasonic wave test, and 5 people who had weight changes more than 5 kg in recent 6 months were included in the exclusion criteria. Among those 297 people in the exclusion criteria, 280 people were finally excluded since 17 people were double counted in the respective category. Among remaining 306 people, 180 people had health checkup in 2008 (Figure 1).
Sociodemographic variables (age, education level, and family income), lifestyle (frequency of drinking, smoking, and exercise), medical history, currently suffering disease, currently taking medicine, and family history of targeted people were identified through written questionnaires and anthropometric data (weight, height, and waist) was collected by experienced nurses. Weight and height was measured by auto body measuring instruments. Weight was measured in the unit of 1 kg after urine in light clothing without shoes and breakfast. Weight change was calculated as 'weight change = weight (kg) as of 2008 - weight (kg) as of 2004.' Three kg which is 5% of 63.3 kg (average weight of subjects) was the criteria to classify into three groups of decreasing group (Ōēż-3.0 kg), stable (-2.9 to 2.9 kg), increasing group (Ōēź3.0 kg). BMI was calculated using the formula of weight (kg)/height (m2). Waist was measured between the lower part of 12th rib and upper part of iliac crest. Blood collection was conducted after checking the empty stomach (fast for 12 hours) from 10 PM of the day before. Triglycerides, high density lipoprotein cholesterol, and fasting blood glucose were analyzed using an automatic chemistry analyzer.
Frequency of drinking per week, favorite type of alcohol, and the amount of drinking per each occasion were recorded. Smoking was classified into non-smoker, ex-smoker, and smoker. Exercise was classified into irregularly exercising group and regularly exercising (more than once a week) group.
Fatty liver was diagnosed through abdominal ultrasonic wave by radiology doctor and was classified as mild degree (mild), moderate degree (moderate), and deep degree (severe), depending on the degree of fat infiltration. Mild degree is the status of a little range of fine echo in liver parenchyme and normally shows the border of diaphragm and intrahepatic vessels. Moderate degree is the status of moderate range of fine echo in liver parenchyme and shows some damage in the image of diaphragm and intrahepatic vessels. Deep degree is the status of vast range of fine echo in liver parenchyme and hardly shows the image of diaphragm and intrahepatic vessels and the back part of right lobe liver.11) In 2004 and 2008, two abdominal ultrasonic wave tests were conducted by different radiology doctors, respectively.
SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. To analyze the results of people who had been measured in 2004 and 2008, paired t-test and one-way analysis of variance were used as continuous variables, McNemar's chisquare test was used as categorical variable. Odds ratio of NAFLD disappearance diagnosed in 2008 was calculated using logistic regression analysis and age, BMI, drinking, smoking, exercise, education level, and income level were corrected. Two sided test was performed and statistically significant level was P < 0.05.
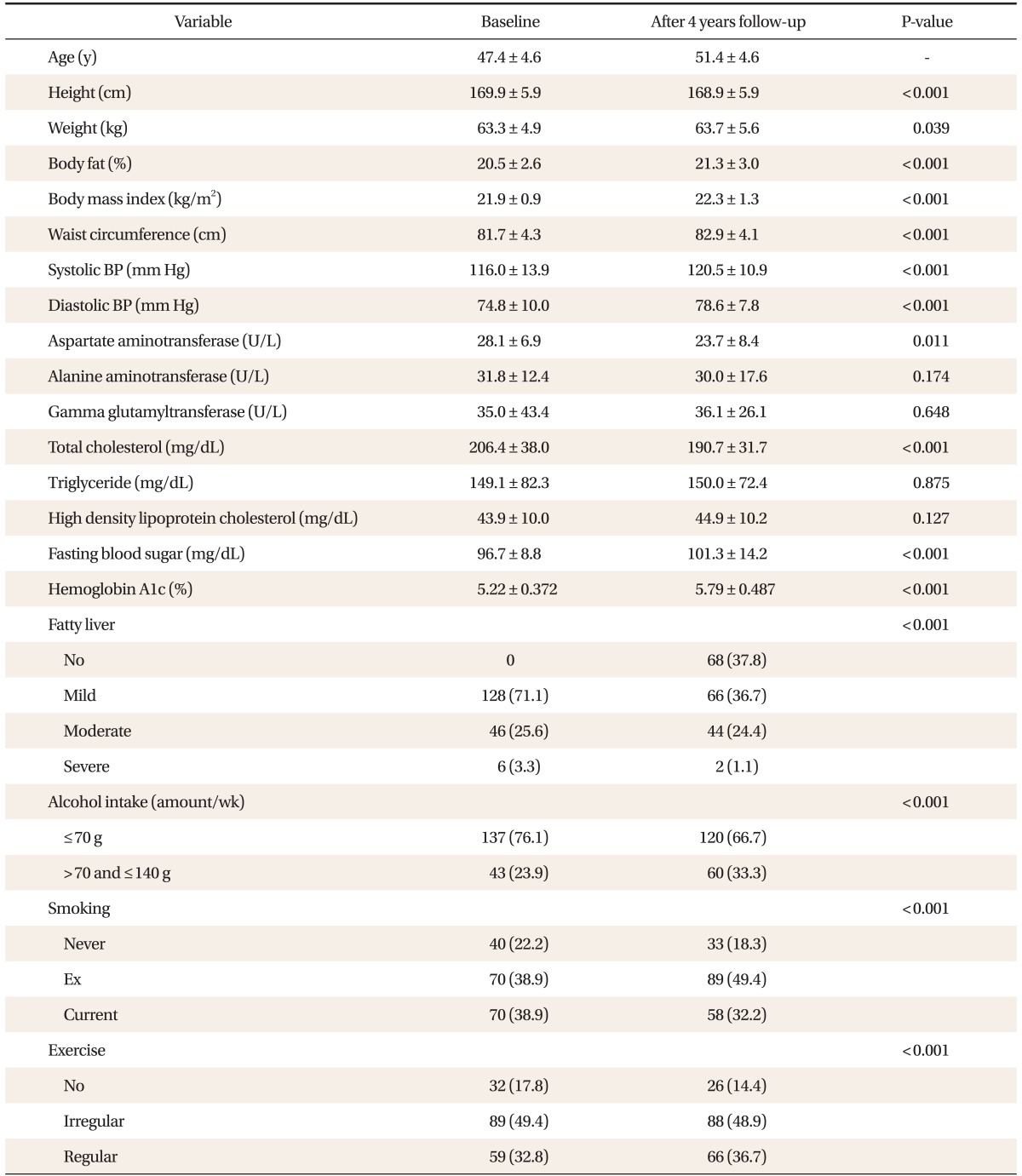
In the beginning of the study (2004), the average age of the subjects was 47.4 ┬▒ 4.6 years old (range, 26 to 63 years old). After 4 years (2008), the height of the subjects was significantly decreased (169.9 cm versus 168.9 cm, P < 0.001) while weight, body fat, and waist were significantly increased. Systolic blood pressure, diastolic blood pressure, fasting blood glucose, and glycosylated hemoglobin were significantly increased after 4 years (P < 0.001) and AST and total cholesterol were significantly decreased (P < 0.001).
In 2004 ultrasonic wave test, the number of mild degree fatty liver was 128 (71.1%), the number of moderate degree fatty liver was 46 (25.6%) and the number of deep degree fatty liver was 6 (3.3%). In 2008 ultrasonic wave test, the number of normal people was 68 (37.8%), the number of mild degree fatty liver was 66 (36.7%), the number of moderate degree fatty liver was 44 (24.4%) and the number of deep degree fatty liver was 2 (1.1%) showing overall improvement in fatty liver opinion (Table 1).
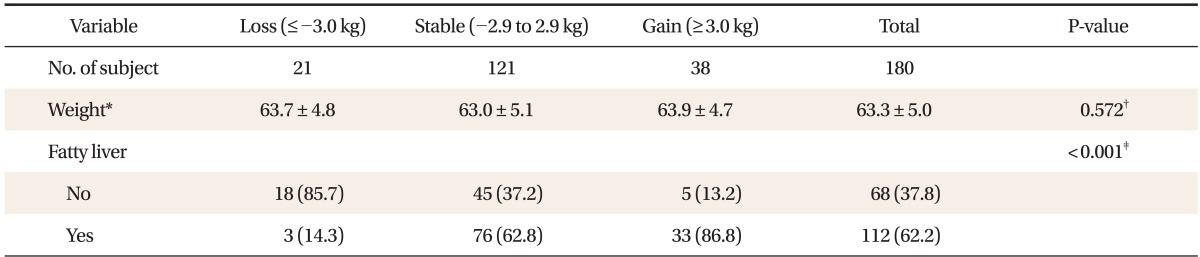
The average weight of the subjects in 2004 was 63.3 ┬▒ 4.9 kg. According to the weight change in 4 years, the subjects were classified into decreasing group, stable group, and increasing group and there was no difference in initial weight among the groups (P = 0.572). Regardless of weight change in 4 years, 37.8% of subjects showed improvement of normal opinion through ultrasonic wave test and 62.2% of the subjects remained the same in fatty liver opinion through ultrasonic wave test. 85.7% of decreasing group showed improvement of normal opinion. 62.8% of stable group and 86.8% of increasing group remained same in fatty liver opinion through ultrasonic wave test which is statistically significant (P < 0.001) (Table 2).
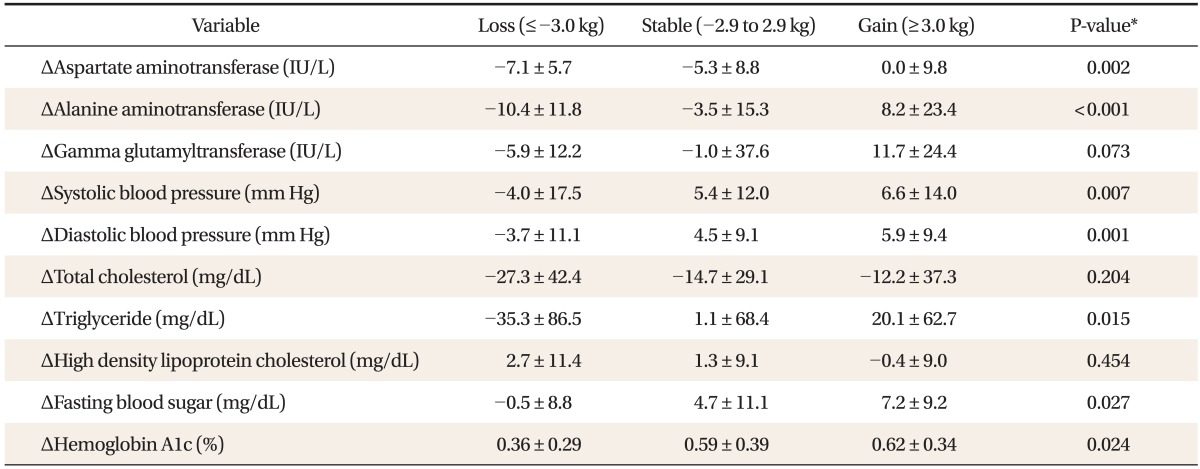
As the classification of group moves from decreasing group to increasing group, systolic blood pressure, diastolic blood pressure, AST, ALT, triglycerides, fasting glucose, and glycosylated hemoglobin increased statistically significantly (Table 3). Of particular note, change in ALT showed statistically significant difference such as decreasing group -10.4 ┬▒ 11.8 U/L, stable group -3.5 ┬▒ 15.3 U/L, increasing group 8.2 ┬▒ 23.4 U/L (P < 0.001) (Table 3). This result corresponds with the improvement in ultrasonic wave test due to weight loss.
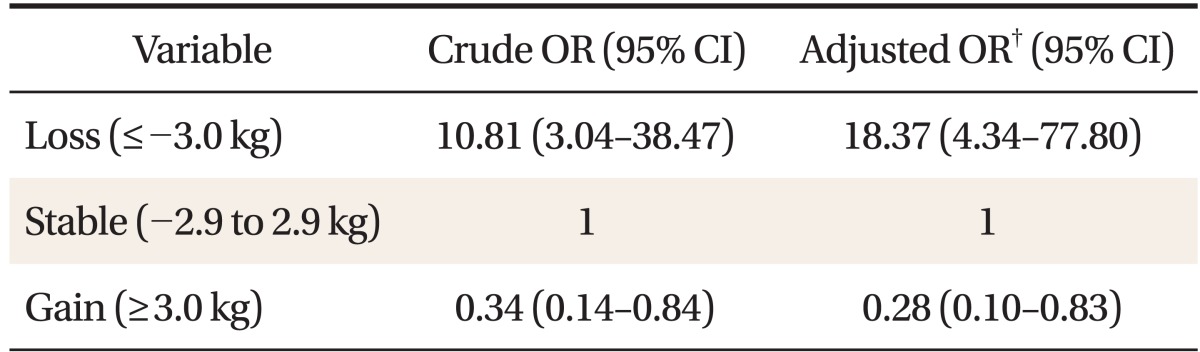
When age, weight, drinking, smoking, exercise, education level, and income level were corrected in the initial test (2004), odds ratio of NAFLD disappearance in 2008 of decreasing group shows 18.37 times (95% confidence interval, 4.34 to 77.80) greater n that of the stable group. Odds ratio of NAFLD disappearance in the increasing group shows 0.28 times (95% confidence interval, 0.10 to 0.83) smaller than that of stable group (Table 4).
NAFLD is easily found through regular abdominal ultrasonic wave test and prevalence rate is increasing all over the world. Through many studies obesity, type 2 diabetes, and hyperlipidemia have been well known as risk factors for change into fatty liver so far. However, there have been insufficient studies on how weight-change affects improvement of NAFLD in the normal weight group. The author's study tried to figure out how post-weight change affects the change of fatty liver for the NAFLD patient of normal weight. The result of 4-year tracking observation of 180 male adults in normal weight who were diagnosed with NAFLD showed that compared to the stable and increasing group, not only fatty liver opinion by ultrasonic wave test but also liver enzymes, fasting glucose, and triglycerides were significantly decreased in the decreasing group.
As obesity is the important cause for NAFLD, losing weight is the only treatment which has reasonable basis for the benefits and safety.9) Since losing weight involves increase of activity and improvement of liver enzymes, histology, serum insulin levels, and quality of life, losing weight is recommended for all the NAFLD patients who are overweight or obese.12,13,14,15,16) As for the way of losing weight, correction of life style is mainly suggested. Drug therapy and surgical therapy are also suggested.
As the study for the effect of losing weight for NAFLD patients of normal weight, there was a recent study of liver transplantation donors which checked the improvement of fatty liver through biopsy after 10-week exercise and dietary control.17) In this study, improvement caused by losing weight was reported not only for the overweight or obese but also for the normal weight subjects. Even though this study targeted Korean people, normal weight was defined as BMI 18.5 to 24.9 kg/m2 which actually included overweight BMI 23 to 24.9 kg/m2 in Korea. Thus, this study is limited in its ability to prove the effect of losing weight for NAFLD patient of normal weight. Though additional studies are necessary, in the study of NAFLD prevalence rate of not-fat Asian and risk cause, Liu18) expected that correction of life style is the most important method for NAFLD treatment and it will have a similar effect on NAFLD patients of normal weight. NAFLD treatment should be conducted with the treatment of liver disease and metabolic disease such as obesity, hyperlipidemia, insulin resistance, and diabetes.19) In the authors' study, the decreasing group showed significant decrease in AST, ALT, triglycerides, and fasting glucose which proved losing weight has an influence on the improvement of liver disease, hyperlipidemia, and diabetes even for the NAFLD patient of normal weight.
In this study, mechanism of treatment by losing weight for the NAFLD patient of normal weight is expected to be similar to the mechanism of overweight or obese NAFLD patient. Jin et al.17) suggested that reducing body fat, especially visceral fat, resulting from weight-loss is the primary factor in the improvement of fatty liver of the NAFLD patient of normal weight. This can be checked by further studies including body fat and waist. As another mechanism, the relationship between the improvement of metabolic diseases such as hyperlipidemia and insulin resistance resulted from losing weight and the improvement of fatty liver might be considered. This corresponds with the authors' study result which showed the significant reduction in triglycerides and fasting glucose.
To diagnose NAFLD, there should be no significant alcohol consumption. However, conducted studies have different points of view in the criteria which vary from less than 10 g to less than 40 g per day. Main organizations such as American Gastroenterological Association, American Association for the Study of Liver Disease and American College of Gastroenterology recommend less than 21 drinks (1 drink = 12 ounce beer) per week for men and less than 14 drinks per week for women.19) In the authors' study, significant alcohol consumption was defined as consuming more than 140 g per week (criteria = 20 g per day) and was excluded from the analysis.
This study has several limitations. First, people who had serial health checkup in Ulsan University Hospital were targeted as subjects and most of the subjects were composed of workers in one company, thus, it is hard for them to represent the general population. Second, since self-writing questionnaire was used for the subjects, there is a possibility of variance in the amount of drinking due to bias which can lead to inaccurate NAFLD diagnosis.
Third, in the diagnosis of NAFLD, without biopsy, the convenient and useful ultrasonic wave test was used which can also lead to inaccurate NAFLD diagnosis.20) Fourth, most of the ultrasonic wave tests for fatty liver were conducted by different radiology doctors in 2004 and 2008, thus, there might be bias in the observers. Last, due to the small number of samples, three groups classified by the degree of weight change have a limit to check the detailed difference. In the future, expanded sample size and detailed grouping will help to acquire better understating in the degree of losing weight to improve fatty liver.
This study has meaning in that family medicine doctors suggested treatment strategies by analyzing the effect of losing weight in NAFLD patients of normal weight who can be commonly seen in the primary health care setting. Through this study, even for normal weight people, the fact that losing weight is an effective way to improve the condition of NAFLD was confirmed. Thus, it is necessary to suggest losing weight to NAFLD patients of normal weight. To make a more detailed suggestion, a large scale of additional studies based on an accurate NAFLD diagnosis will be required.
References
1. Bugianesi E, Leone N, Vanni E, Marchesini G, Brunello F, Carucci P, et al. Expanding the natural history of nonalcoholic steatohepatitis: from cryptogenic cirrhosis to hepatocellular carcinoma. Gastroenterology 2002;123:134-140. PMID: 12105842.


2. Angelico F, Del Ben M, Conti R, Francioso S, Feole K, Maccioni D, et al. Non-alcoholic fatty liver syndrome: a hepatic consequence of common metabolic diseases. J Gastroenterol Hepatol 2003;18:588-594. PMID: 12702052.


3. Bayard M, Holt J, Boroughs E. Nonalcoholic fatty liver disease. Am Fam Physician 2006;73:1961-1968. PMID: 16770927.

4. Clark JM. The epidemiology of nonalcoholic fatty liver disease in adults. J Clin Gastroenterol 2006;40(Suppl 1):S5-S10. PMID: 16540768.

5. American Gastroenterological Association. American Gastroenterological Association medical position statement: nonalcoholic fatty liver disease. Gastroenterology 2002;123:1702-1704. PMID: 12404244.


6. Sanyal AJ. American Gastroenterological Association. AGA technical review on nonalcoholic fatty liver disease. Gastroenterology 2002;123:1705-1725. PMID: 12404245.


7. Ueno T, Sugawara H, Sujaku K, Hashimoto O, Tsuji R, Tamaki S, et al. Therapeutic effects of restricted diet and exercise in obese patients with fatty liver. J Hepatol 1997;27:103-107. PMID: 9252081.


8. Harrison SA, Fincke C, Helinski D, Torgerson S, Hayashi P. A pilot study of orlistat treatment in obese, non-alcoholic steatohepatitis patients. Aliment Pharmacol Ther 2004;20:623-628. PMID: 15352910.


9. Sheth SG, Chopra S. Natural history and management of nonalcoholic fatty liver disease in adults. UpToDate. In: Post TW, editor. UpToDate [Internet]. Waltham (MA): UpToDate; 2014. [cited 2014 Feb 14]. Available from: http://www.uptodate.com
10. Hsieh SD, Yoshinaga H, Muto T, Sakurai Y, Kosaka K. Health risks among Japanese men with moderate body mass index. Int J Obes Relat Metab Disord 2000;24:358-362. PMID: 10757631.


11. Mittelstaedt CA. General ultrasound. New York: Churchill Livingstone; 1992.
12. Hickman IJ, Jonsson JR, Prins JB, Ash S, Purdie DM, Clouston AD, et al. Modest weight loss and physical activity in overweight patients with chronic liver disease results in sustained improvements in alanine aminotransferase, fasting insulin, and quality of life. Gut 2004;53:413-419. PMID: 14960526.



13. Dixon JB, Bhathal PS, Hughes NR, O'Brien PE. Nonalcoholic fatty liver disease: improvement in liver histological analysis with weight loss. Hepatology 2004;39:1647-1654. PMID: 15185306.


14. Petersen KF, Dufour S, Befroy D, Lehrke M, Hendler RE, Shulman GI. Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes 2005;54:603-608. PMID: 15734833.



15. Promrat K, Kleiner DE, Niemeier HM, Jackvony E, Kearns M, Wands JR, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology 2010;51:121-129. PMID: 19827166.



16. Keating SE, Hackett DA, George J, Johnson NA. Exercise and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Hepatol 2012;57:157-166. PMID: 22414768.


17. Jin YJ, Kim KM, Hwang S, Lee SG, Ha TY, Song GW, et al. Exercise and diet modification in non-obese non-alcoholic fatty liver disease: analysis of biopsies of living liver donors. J Gastroenterol Hepatol 2012;27:1341-1347. PMID: 22554085.


18. Liu CJ. Prevalence and risk factors for non-alcoholic fatty liver disease in Asian people who are not obese. J Gastroenterol Hepatol 2012;27:1555-1560. PMID: 22741595.


19. Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology 2012;142:1592-1609. PMID: 22656328.


20. Lewis JR, Mohanty SR. Nonalcoholic fatty liver disease: a review and update. Dig Dis Sci 2010;55:560-578. PMID: 20101463.


Figure┬Ā1
Selection of study subjects from men having health checkup in 2004. BMI: body mass index. *Categories not mutually exclusive.
Table┬Ā2
The baseline body weight and the status of fatty liver by weight change group after 4 years
Table┬Ā3
Mean changes and SD of liver function and metabolic morbidities by weight change groups for 4 years
- TOOLS
-
METRICS

- Related articles in KJFM
-
The Clinical Implication of Non-alcoholic Fatty Liver Disease.2003 June;24(6)
The Relation of Nonalcoholic Fatty Liver Disease to Metabolic Syndrome.2004 October;25(10)
The Association of Nonalcoholic Fatty Liver Disease with Metabolic Syndrome.2007 September;28(9)
The Association of Non-alcoholic Fatty Liver Disease and Physical Activity.2008 July;29(7)