The Correlation between the Triglyceride to High Density Lipoprotein Cholesterol Ratio and Computed Tomography-Measured Visceral Fat and Cardiovascular Disease Risk Factors in Local Adult Male Subjects
Article information
Abstract
Background
We studied the association between the triglyceride to high-density lipoprotein cholesterol ratio and computed tomography-measured visceral fat as well as cardiovascular risk factors among Korean male adults.
Methods
We measured triglycerides, high density lipoprotein cholesterol, body mass, waist circumference, fasting plasma glucose, hemoglobin A1c, systolic blood pressure, diastolic blood pressure, visceral fat, and subcutaneous fat among 372 Korean men. The visceral fat and subcutaneous fat areas were measured by computed tomography using a single computed tomography slice at the L4-5 lumbar level. We analyzed the association between the triglyceride to high density lipoprotein cholesterol ratio and visceral fat as well as cardiovascular risk factors.
Results
A positive correlation was found between the triglyceride to high density lipoprotein cholesterol ratio and variables such as body mass index, waist circumference, fasting plasma glucose, hemoglobin A1c, visceral fat, and the visceral-subcutaneous fat ratio. However, there was no significant correlation between the triglyceride to high density lipoprotein cholesterol ratio and subcutaneous fat or blood pressure. Multiple logistic regression analyses revealed significant associations between a triglyceride to high density lipoprotein cholesterol ratio ≥3 and diabetes, a body mass index ≥25 kg/m2, a waist circumference ≥90 cm, and a visceral fat area ≥100 cm2. The triglyceride to high density lipoprotein cholesterol ratio was not significantly associated with hypertension.
Conclusion
There were significant associations between the triglyceride to high density lipoprotein cholesterol ratio and body mass, waist circumference, diabetes, and visceral fat among a clinical sample of Korean men. In the clinical setting, the triglyceride to high density lipoprotein cholesterol ratio may be a simple and useful indicator for visceral obesity and cardiovascular disease.
INTRODUCTION
Dyslipidemia is a major risk factor for cardiovascular disease, and various studies have been performed to investigate dyslipidemia as a diagnostic tool for metabolic syndrome.1) Many recent studies have shown that lipid ratios (i.e., the total cholesterol/high density lipoprotein cholesterol [HDLC] ratio, the triglyceride [TG]/HDLC ratio, the low density lipoprotein cholesterol [LDLC]/HDLC ratio, or the non-HDLC/HDLC ratio) can be used to predict cardiovascular disease more effectively than individual lipid levels. In particular, various studies have demonstrated that the TG/HDLC ratio is associated with cardiovascular disease, insulin resistance, and metabolic syndrome.234) These findings can be explained by the atherogenic properties of the TG/HDLC ratio. In other words, as the TG/HDLC ratio increases, the LDL particle size is reduced, and these small, dense LDL particles increase the fractional esterification rate of the apolipoprotein B-lipoproteins, thereby causing arteriosclerosis.5) Indeed, the TG/HDLC ratio has been reported to be correlated with increased atherosclerotic cardiovascular disease as well as overall mortality67) and is gaining more attention for its usefulness in enabling quick and simple screening for metabolic diseases and cardiovascular disease in clinical settings.78)
On the other hand, obesity, particularly abdominal obesity, is usually accompanied by hypertension, hyperlipidemia, insulin resistance, type 2 diabetes, and cardiovascular disease. Visceral fat is the leading cause of cardiovascular disease,9) and a strong correlation between the risk factors of cardiovascular disease and visceral fat has been demonstrated in domestic studies.10) Therefore, quantitative evaluation of abdominal visceral fat is important for assessing the risk of cardiovascular disease. Usually, the degree of visceral obesity is determined by measuring waist circumference and abdominal obesity, but this method is limited by its inability to determine the extent of visceral and subcutaneous fat. The most accurate method for determining the degree of abdominal visceral fat is to measure the area or volume of the visceral fat using computed tomography (CT), which can measure visceral and subcutaneous fat separately.11)
In a previous study examining the correlation between the CT-measured visceral and subcutaneous fat and cardiovascular disease, both men and women exhibited an increased risk of cardiovascular disease when the visceral fat area was more than 100 cm2. Furthermore, patients showed distinctive blood and lipid metabolic disorders with visceral fat areas greater than 130 cm2.12) Another study showed that patients with a visceral fat area/subcutaneous fat area ratio (V/S ratio) greater than 0.4 exhibited a significantly higher incidence of blood and lipid metabolic disorders than those with a V/S ratio less than 0.4.13)
Although many studies have demonstrated a correlation between the TG/HDLC ratio and outcomes such as insulin resistance, an increased risk of atherosclerotic cardiovascular disease, and metabolic syndrome, to date few studies have been performed to show a direct correlation with the visceral fat area as measured by CT. In the current study, we investigated the correlation between the TG/HDLC ratio and CT-measured visceral fat as well as cardiovascular risk factors in local adult male subjects who visited the University Hospital Health Promotion Center. We also evaluated the effectiveness of the TG/HDLC ratio as an indicator of visceral fat and cardiovascular disease risk.
METHODS
1. Study Subjects
Data were collected from 892 urban-dwelling males who visited the University Hospital Health Promotion Center and underwent medical examination and abdominal CT between March 2012 and January 2013. All subjects were informed of their autonomy as research participants and guaranteed anonymity. Written consent was received from all participants, and the study was approved by local ethics committees (IRB no. WKUH 201507-HRE-062). Those lacking a complete medical history or medication records, those with chronic diseases other than hypertension or diabetes, and those who had received cancer treatment in the past or were diagnosed with cancer were excluded. The number of subjects included in the final analysis was 372.
2. Measures
1) Questionnaire, anthropometrics, and blood pressure
Participants received a self-administered questionnaire and were interviewed by doctors. Anthropometric measurements were performed by trained nurses. Height and weight were measured using automatic measuring devices, and the body mass index (BMI) was obtained by dividing the weight by the square of the height (BMI=kg/m2). Waist circumference was measured by placing a tape measure horizontally in between the lowest part of the costal bone and the highest part of the pelvic iliac crest with the patient in the upright position, following the World Health Organization recommendations. Blood pressure was measured after 10 minutes of rest using an automatic blood pressure measurement device (BP-8800C; Colin Electronics Co. Ltd., Aichi, Japan). Blood pressure was measured again if the systolic blood pressure (SBP) was greater than 140 mm Hg or the diastolic blood pressure (DBP) was greater than 90 mm Hg. The average value of the SBP and DBP measurements was recorded.
2) Blood tests
Participants were requested to fast for at least 12 hours, and blood was collected and analyzed under fasting conditions. Glycated hemoglobin (hemoglobin A1c [HbA1c]), fasting plasma glucose, total cholesterol, TG, HDLC, and LDLC were measured using an ADVIA 1650 analyzer (Bayer Diagnostics, Tarrytown, NY, USA).
3) The abdominal fat area
A fat area was defined as an area scoring -150 to -50 Hounsfield units on the CT scan. Subcutaneous fat was defined as the fat located between the skin and the rectus abdominis muscle, obliquus abdominis muscle, and erector spinae muscle at naval height. Visceral fat was defined as the fat between the rectus abdominis muscle, obliquus abdominis muscle, quadratus lumborum muscle, psoas muscle, and lumbar vertebrae at the same height. Three horizontal, 10-mm-thick abdominal CT sections taken at the L4-L5 lumbar level were selected to calculate the averages for the visceral fat area and the subcutaneous fat area. The V/S ratio was determined by dividing the CT-measured visceral fat area by the CT-measured subcutaneous fat area.
3. Statistical Analysis
We used SPSS for Windows ver. 11.5 (SPSS Inc., Chicago, IL, USA) for the statistical analyses. Statistical significance was defined as a value of P<0.05. A multivariate regression was employed to test the correlation between visceral fat and cardiovascular disease (as continuous variables) and the TG/HDLC ratio. In groups with a TG/HDLC ratio greater than 3, visceral fat and cardiovascular risk factors were analyzed as non-continuous variables.
RESULTS
1. General Characteristics of the Study Subjects
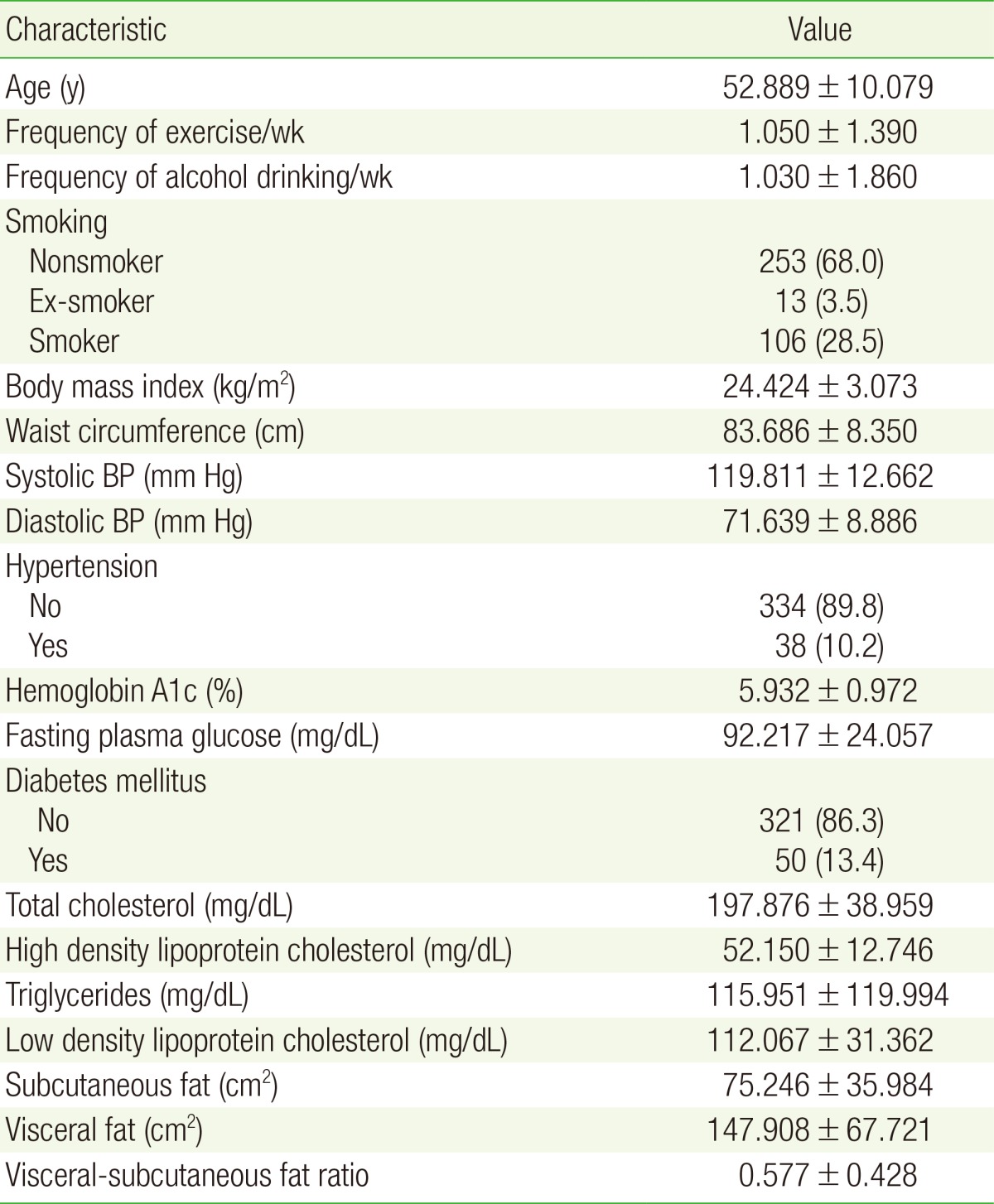
All of the 372 subjects were male, and the average age was 52 years old. Subjects engaged in exercise an average of 1.050±1.390 times per week and drank alcohol an average of 1.030±1.860 times per week. Among the total sample, 106 individuals were smokers (28.5%). With respect to cardiovascular risk indicators, the average BMI fell within the upper limit of the normal range, the mean waist circumference fell within the normal range, the average SBP and DBP fell within the prehypertensive level, the mean HbA1c, fasting plasma glucose, total cholesterol, HDLC, TG, and LDLC fell within the upper limit of the normal range, and the average subcutaneous and visceral fat area and V/S ratio was above the normal range. There were 38 hypertensive patients (10.2%) and 50 patients with diabetes (13.4%) (Table 1).
2. Correlation between the Triglyceride/High Density Lipoprotein Cholesterol Ratio and Visceral Fat and Cardiovascular Risk Factors (as Continuous Variables)
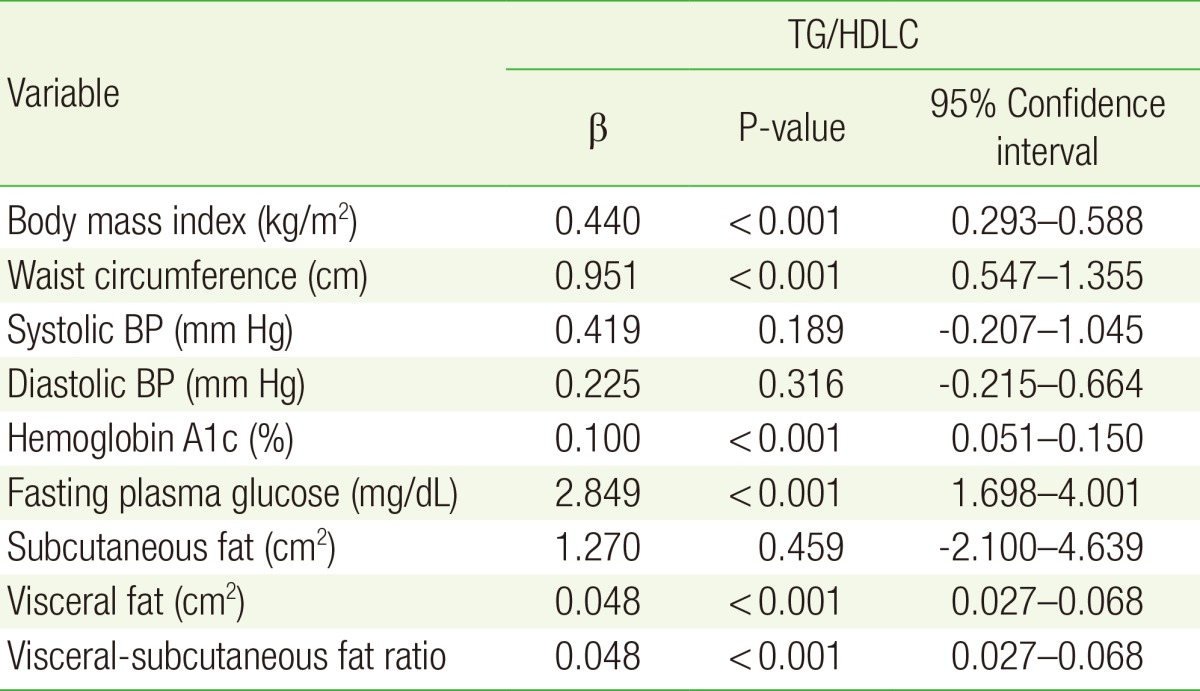
The visceral fat area, V/S ratio, BMI, and waist circumference as well as the HbA1c and fasting plasma glucose levels all showed a positive correlation with the TG/HDLC ratio (P<0.001 for all correlations); however, SBP, DBP, and subcutaneous fat showed no statistically significant association (Table 2).
3. Correlation between the Triglyceride/High Density Lipoprotein Cholesterol Ratio and Visceral Fat and Cardiovascular Risk Factors (as Non-Continuous Variables)
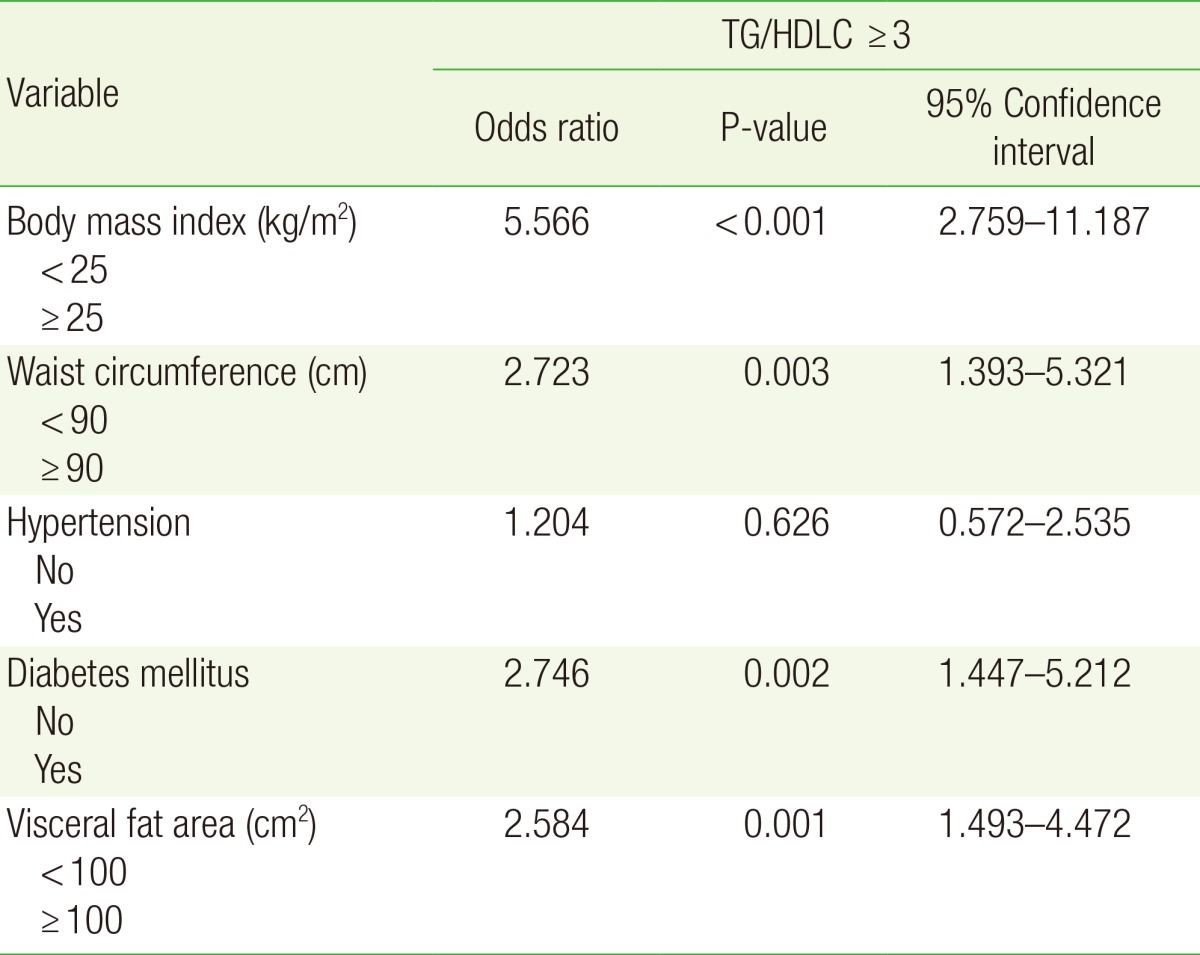
In patients with a TG/HDLC ratio of 3 or higher, having a visceral fat area of ≥100 cm2, a BMI of ≥25 kg/m2, a waist circumference of ≥90 cm, and diabetes were significantly associated with the TG/HDLC ratio (P=0.001, P<0.001, P=0.003, and P=0.002, respectively); however, hypertension showed no significant association (Table 3).
DISCUSSION
It has been well documented that middle-aged Korean men are threatened by ailments such as type 2 diabetes, hypertension, hyperlipidemia, and cardiovascular disease. It has also been shown that the recent dramatic increase in the incidence of obesity is a major cause of these chronic progressive diseases. However, although the average waist circumference and BMI of Koreans is lower than those found in Western populations, the risk of cardiovascular disease is higher in Koreans due to the higher incidence of abdominal obesity.14) Moreover, Korean men have higher rates of smoking and alcohol consumption than Korean women and higher levels of visceral fat than women with the same degree of obesity or waist circumference.10) Therefore, the TG/HDLC ratio may be a useful assessment tool for identifying visceral obesity and cardiovascular disease among this population.
The current study investigated the correlation between the TG/HDLC ratio and CT-measured visceral fat and cardiovascular disease risk factors in local adult males. The results indicated that the TG/HDLC ratio is positively correlated with BMI (P<0.001), waist circumference (P<0.001), visceral fat (P<0.001), and the V/S ratio (P<0.001), but not with the amount of subcutaneous fat. Previous studies support our results and have shown that visceral fat is correlated with metabolic risk factors including a reduction in HDLC as well as an increase in TG and insulin resistance, but not with abdominal subcutaneous fat.1516) Many studies have also reported a positive correlation between the TG/HDLC ratio and waist circumference;171819) however, the correlation between the TG/HDLC ratio and BMI has been inconsistent.181920)
In this study, the TG/HDLC ratio was associated with diabetes and showed a positive correlation with fasting plasma glucose and HbA1c. Although the TG/HDLC ratio in Caucasians and Koreans has shown a positive correlation with insulin resistance,1721) no such correlation is found in African Americans,22) indicating differences according to race. Furthermore, studies examining the association between the TG/HDLC ratio and diabetes reported that the TG/HDLC ratio was an independent risk factor for type 2 diabetes.23) Similar studies have also shown that the TG/HDLC ratio indicates hyperinsulinemia in men and can predict type 2 diabetes,24) findings that support the results of our study.
However, although dyslipidemia is a risk factor for hypertension in men,25) and studies have identified the TG/HDLC ratio as a predictor of hypertension,2426) our findings showed no significant correlation between the TG/HDLC ratio and hypertension. Given these conflicting results as well as the small number of subjects in this cross-sectional study, prospective studies with a large number of participants are required to elucidate the correlation between the TG/HDLC ratio and hypertension.
Furthermore, previous studies indicated a higher risk of cardiovascular disease when the TG/HDLC ratio was greater than 3.1727) Therefore, we examined the correlation between cardiovascular disease risk factors in those exhibiting a TG/HDLC ratio higher than 3 using a multivariate logistic regression analysis. When the TG/HDLC ratio was greater than 3, a strong correlation was observed with a BMI of 25 kg/m2 or higher, a waist circumference of 90 cm and above, a visceral fat area of 100 cm2 and greater, and diabetes. A BMI of 25 kg/m2 (indicating obesity),28) a waist circumference of 90 cm (indicating male abdominal obesity),29) a visceral fat area of 100 cm2 (indicating an increased risk of cardiovascular disease),12) and diabetes are all risk factors for cardiovascular disease. We were able to validate previous studies showing that a TG/HDLC ratio higher than 3 is strongly correlated with a high risk for cardiovascular disease. 728) However, considering that this TG/HDLC ratio cutoff has been studied in limited ethnic groups only and is known to differ by sex and race,830) we suggest that a large-scale study covering various ethnic groups, including Koreans, be conducted in the future.
Our study has several limitations. First, a selection bias limits the generalizability of our study. For example, only men were included in the analyses, indicating that our results cannot be applied to females. In addition, only those who underwent abdominal CT as a means of health screening were included indicating that the participants represent a Korean adult male population that is relatively more interested in their health care than the general population. As such, the results may not apply to all Korean adult males. Furthermore, we did not consider factors (such as smoking, drinking, diet, exercise, and stress) that could affect the TG/HDLC ratio; thus, we were not able to identify a causal relationship between the TG/HDLC ratio and the visceral fat area. Therefore, in order to accurately assess the correlation between the TG/HDLC ratio and visceral fat and cardiovascular risk factors, a multi-institution, large-scale prospective study that complements the previously mentioned points is needed.
Our study is significant because it is the first domestic study showing the correlation between the TG/HDLC ratio and CT-measured visceral fat in urban-dwelling men. Moreover, we demonstrated that the TG/HDLC ratio is related to BMI, waist circumference, fasting plasma glucose, HbA1c, and diabetes. Since the TG/HDLC ratio can be easily and inexpensively obtained, it can be effectively employed in clinical settings. However, further studies are needed to identify the TG/HDLC ratio cutoff level for selecting high-risk groups for cardiovascular disease and visceral obesity in Koreans.
ACKNOWLEDGMENTS
This study was supported by a Wonkwang University 2015 grant.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.