 |
 |
- Search
| Korean J Fam Med > Volume 37(2); 2016 > Article |
Abstract
Background
The purpose of this study was to compare the physical activity and caloric intake trends of lipid-lowering drug users with those of non-users among Korean adults with dyslipidemia.
Methods
This study was a repeated cross-sectional study with a nationally representative sample of 2,635 Korean adults with dyslipidemia based on the 2010ŌĆō2013 Korea National Health and Nutrition Examination Survey. Physical activity was assessed using the International Physical Activity Questionnaire, and caloric intake was estimated through 24-hour dietary recall. All statistical analyses were conducted using IBM SPSS ver. 21.0 (IBM Co., Armonk, NY, USA). The changes in physical activity and caloric intake were investigated for lipid-lowering drug users and non-users using generalized linear models.
Results
The proportion of lipid-lowering drug users in the 2010ŌĆō2013 survey population increased from 3.5% to 5.0% (P<0.001). Among adults of dyslipidemia, total of 1,562 participants (56.6%) reported taking lipid-lowering drugs, and 1,073 (43.4%) reported not taking lipid-lowering drugs. Drug users were more likely to be older and less educated and to have a diagnosis of diabetes, higher body mass index, and lower low density lipoprotein cholesterol level. Physical activity trends were tested separately for the lipid-lowering drug users and non-users, and a significant decrease was found among the drug users during the study period. Physical activity among the drug users in 2013 was 38% lower (1,357.3┬▒382.7 metabolic equivalent [MET]; P for trend=0.002) than in 2010 (2,201.4┬▒442.6 MET). In contrast, there was no statistically significant difference between drug users and non-users in the trend of caloric intake during the same period.
Dyslipidemia is a major risk factor for cardiovascular disease; total cholesterol, low density lipoprotein cholesterol (LDLC), and triglyceride levels are directly proportional to the risk of cardiovascular mortality.1) Thus, management of blood cholesterol is important to prevent cardiovascular disease.
The American College of Cardiology and the American Heart Association (ACC-AHA) and the National Institute for Health and Care Excellence guidelines for the treatment of blood cholesterol emphasized the importance of dietary changes and regular physical activity as the first line of management for dyslipidemia.2,3,4,5) In a randomized controlled pilot study, the National Cholesterol Education Program (NCEP) step 1 diet program reduced total cholesterol and LDLC levels by 5% and 13%, respectively, and the NCEP exercise program was associated with an increase in high density lipoprotein cholesterol level.6)
The use of lipid-lowering drugs has rapidly increased in Korea and the United States,7,8) and implementing the 2013 guidelines of the ACC-AHA for the management of cholesterol would increase the number of US adults who would be eligible for statin use from 37.5% to 48.6%.9) Furthermore, caloric and fat intake in Korean and US adults has increased over the past 10 years.7,10) Therefore, it is important to investigate the effects of dietary modification and physical activity on patients with dyslipidemia. In the early 2000s, a cross-sectional study, the Study of Exercise and Nutrition in Older Rhode Islanders Project, showed that participants who reported taking lipid-lowering drugs had better lipid profiles and lower caloric intake than statin non-users, but no significant difference in physical activity was reported among study subjects.11) A cross-sectional study in Sweden in 2004 investigated the perception of risk factors for cardiovascular disease among adults using statins, and found that statin users were more likely to avoid fatty foods and to eat foods with a high fiber content.12) A cross-sectional study using the data of the National Health and Nutrition Examination Survey (NHANES) conducted during 1999ŌĆō2010 compared the trend of caloric and fat intake between statin users and non-users over time and found a significant increase in the caloric and fat intake of statin users.13) To our knowledge, no studies have examined the cross-sectional relationship between physical activity and the use of lipid-lowering drugs among Korean adults with dyslipidemia. The purpose of the present study was to compare physical activity and caloric intake trends of lipid-lowering drug users with those of non-users among Korean adults with dyslipidemia.
The Korea National Health and Nutrition Examination Survey (KNHANES), first conducted in 1998, is a nationally representative survey that assesses the health and nutritional status of the Korean population. The survey is conducted by the Korea Centers for Disease Control and Prevention. It has three different components: a health interview survey, health examination, and nutrition survey. The health interview survey is used to collect information regarding housing characteristics, socioeconomic status, and physical activity using face-to-face interviews and self-administered questionnaires. The health examination includes body measurements and laboratory tests (blood and urine). The nutrition survey is conducted using face-to-face interviews and collects information regarding dietary behaviors, dietary supplement use, food frequency, and food intake.
In the fifth and sixth KNHANES (2010ŌĆō2013), of 33,553 participants, 30,918 subjects were excluded. Subjects were excluded from this study if they were less than 20 years old or pregnant women. Also excluded were those without dyslipidemia or those with missing data regarding dyslipidemia and lipid-lowering drug use. The final sample size for this study was 2,635.
Subjects were considered to have dyslipidemia if they reported a diagnosis of dyslipidemia by a doctor in the health interview survey. We defined lipid-lowering drug users as participants with dyslipidemia who had been taking lipid-lowering drugs, and we categorized the subjects into two groups: lipid-lowering drug users and non-users.
Food intake was measured through 24-hour dietary recall in the KNHANES. The dietary questionnaire was administered during face-to-face interviews and included the type, amount, and frequency of foods or drinks consumed during the previous day.
Physical activity was assessed using the Korean version of the International Physical Activity Questionnaire (IPAQ).14,15) The IPAQ includes questions regarding the duration (minutes per day) and frequency (days per week) of vigorous, moderate-intensity, and walking activities, such as the following question: "During the last 7 days, on how many days did you perform vigorous physical activities such as heavy lifting, heavier gardening or construction work, chopping wood, aerobics, jogging/running, or fast bicycling? How much time did you usually spend doing vigorous physical activities on one of those days?" The number of hours was weighted by the specific metabolic equivalent (MET) score for each activity.
We extracted the data for sociodemographic characteristics including age, sex, level of education, and marital status. Subjects were classified into the following age groups: 20 to 39 years, 40 to 59 years, and 60 years or older. Level of education was classified into less than elementary school (Ōēż6 years), less than high school graduation (Ōēż12 years), or high school graduation or more (>12 years).
Self-reported health status was classified into good, intermediate, or bad. We categorized alcohol intake into 2 groups: less than once a month or once or more than once a month. Smoking status was classified into non-smoker or current smoker. Body mass index (BMI), calculated as weight in kilograms divided by height in meters squared, was categorized into 3 groups: <18.5 kg/m2, 18.5ŌĆō25 kg/m2, or >25 kg/m2.16)
All statistical analyses were performed using IBM SPSS ver. 21.0 (IBM Co., Armonk, NY, USA). In order to represent the Korean population, stratified random sampling (kstrata), cluster sampling (psu), and sampling weights (wt_itvex) were used. Data analyses were performed to account for the complex sample design.
We analyzed the differences in categorical variables (such as level of education, marital status, alcohol intake, and smoking status) using chi-square tests and continuous variables (total cholesterol level and LDLC level) using t-tests in complex sample analysis. General linear models were used to estimate the trends of physical activity and caloric intake among Korean adults with dyslipidemia, after adjusting for sex, age group, level of education, marital status, BMI, and diagnosis of diabetes. P-values <0.05 were considered statistically significant.
In the 2010ŌĆō2013 KNHANES, the weighted proportion of adults with dyslipidemia increased from 6.1% (2010) to 8.7% (2013, P for trend<0.001), and the percentage of lipid-lowering drug users significantly increased from 3.5% to 5.0% (P for trend<0.001) (Table 1).
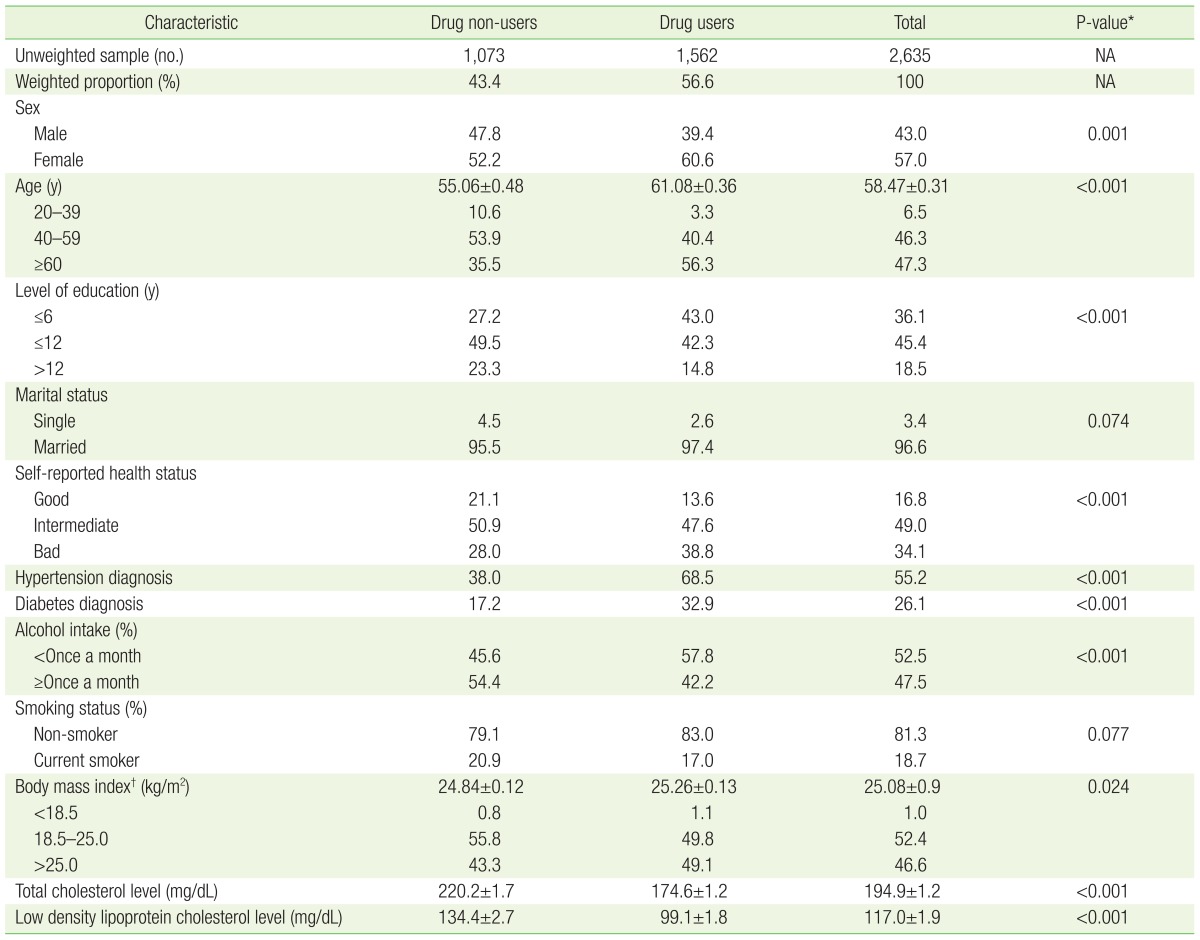
A total of 2,635 participants reported a diagnosis of dyslipidemia. Of this population, 1,562 (Weighted proportion, 56.6%) reported taking lipid-lowering drugs, and 1,073 Weighted proportion (43.4%) reported not taking lipid-lowering drugs (Table 2).
There were significant differences between the two groups for the different variables we examined with the exception of smoking and marital status. The mean age of participants was 58.47┬▒0.31 years; the average age of drug users was 61.08┬▒0.36 years, which was significantly older than that of non-users (55.06┬▒0.48 years, P<0.001).
Lipid-lowering drug users were more likely to be older, female, and less educated, and to have a diagnosis of diabetes, higher BMI, and lower LDLC level. The BMI of drug users was 25.26┬▒0.13 kg/m2, which was higher than that of non-users (24.84┬▒0.12 kg/m2, P=0.024). Drug users had significantly lower levels of total cholesterol and LDLC than non-users (P<0.001).
In Table 3 and Figure 1, adjusted for sex, age group, level of education, marital status, BMI, and diagnosis of diabetes, we examined the trends of physical activity and caloric intake separately for lipid-lowering drug users and non-users by year in the 2010ŌĆō2013 study period.
The physical activity of drug users was 2,201.4┬▒442.6 MET in 2010, 1,521┬▒406.6 MET in 2011, 1,480.8┬▒674.6 MET in 2012, and 1,357.3┬▒382.7 MET in 2013, which was 38% lower than that of 2010. Thus, the physical activity of drug users significantly decreased from 2010 to 2013 (P for trend=0.002). The physical activity of non-users decreased from 2010 (2,090.4┬▒425.0 MET) to 2013 (1,846.1┬▒430.5 MET), but this decrease was not statically significant (P for trend=0.50). There was no significant trend in caloric intake during 2010ŌĆō2013 for either drug users (P for trend=0.10) or non-users (P for trend=0.97).
Among Korean adults with dyslipidemia, physical activity significantly decreased for lipid-lowering drug users, which was not observed among non-users in the KNHANES 2010ŌĆō2013 period.
To our knowledge, there are no other published studies in Korea examining the trends of physical activity and caloric intake among adults with dyslipidemia. In the 1999ŌĆō2010 NHANES, the caloric and fat intake of statin users during the 1999ŌĆō2004 study period was lower than that of statin non-users. However, statin users increased their caloric and fat intake over time until it was higher than in statin non-users.13) These results correspond with our findings that dietary modifications were not observed. In the Rhode Island cross-sectional study during the early 2000s, the caloric intake of statin users among adults older than 60 was lower than in statin non-users.11) The cross-sectional study in Sweden in 2004 showed statin users consumed higher-fat foods than statin non-users.12) This appears to corroborate the aforesaid report that caloric intake of statin users was lower than in the statin non-users in the NHANES during the early 2000s. A cohort study in primary care clinics in the US examined patients who received their first prescription for statins in 2005. These researchers found that 76% of the participants wanted to reduce dietary fat intake; however, no significant change in caloric and fat intake was reported during the 6-month observation period.17) This study had the advantage of being a longitudinal cohort study in which causal relationships may be inferred, but the 71-participant sample size was too small and the observation period of 6 months was too short to confirm the behavioral change associated with statin use. We examined the trends of physical activity and caloric intake through a nationwide cross-sectional study using the KNHANES.
In the guidelines of blood cholesterol management, lifestyle modification is a key component of controlling blood cholesterol and preventing cardiovascular disease.2,3,4,5) A decrease in physical activity and higher BMI among statin users compared to non-users shows that lifestyle management among lipid-lowering drug users is not satisfactory. There are three possible hypotheses to explain these results. First, the improved levels of total cholesterol and LDLC after taking lipid-lowering drugs could weaken patients' motivation to follow the recommended physical activity program. Second, patients who are unwilling to make lifestyle changes may prefer to take lipid-lowering drugs, while physically active patients may prefer not to take the drugs. Third, recent dyslipidemia guidelines emphasize pharmacological treatment; thus, patient education regarding lifestyle modifications could be weak.13)
This study had several limitations. Physical activity and caloric intake data were obtained through the self-report questionnaires used in the KNHANES; thus, there is a risk of self-report bias. In addition, elderly patients may have difficulty remembering their physical activities and food intake. However, the reliability and validity of the IPAQ were proven in 14 centers from 12 countries.14,15) The second limitation is that the questionnaire used in the KNHANES investigated only whether patients were taking any lipid-lowering drugs, not the specific drug ingredients. Third, this study is a repeated cross-sectional study rather than a cohort study; thus, the participants differed during each study period.13) Even though we cannot infer that the physical activity of individual study participants decreased over time, the nationally representative surveillance data of the KNHANES was a strength of this study.
This study found a statistically significant decrease in the physical activity of Korean patients who reported taking lipid-lowering drugs, which was not observed among the non-users during the 2010ŌĆō2013 study period. Based on this result, we suggest that the implementation of lifestyle modifications is insufficient. Physicians should stress the importance of physical activity along with lipid-lowering drugs for lipid-lowering drug users. In addition, pharmacological therapy for the treatment of cardiovascular and chronic disease is increasing; thus, future studies examining the association between taking drugs and lifestyle modification may be needed.
References
1. Bezafibrate Infarction Prevention (BIP) study. Secondary prevention by raising HDL cholesterol and reducing triglycerides in patients with coronary artery disease. Circulation 2000;102:21-27. PMID: 10880410.


2. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143-3421.


3. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(25 Suppl 2):S1-S45. PMID: 24222016.


4. Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63(25 Pt B):2960-2984. PMID: 24239922.


5. National Clinical Guideline Centre for Acute and Chronic Conditions, National Institute for Health and Care Excellence. Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. London: National Clinical Guideline Centre; 2014.
6. Lalonde L, Gray-Donald K, Lowensteyn I, Marchand S, Dorais M, Michaels G, et al. Comparing the benefits of diet and exercise in the treatment of dyslipidemia. Prev Med 2002;35:16-24. PMID: 12079437.


7. Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention. The fifth and sixth Korea National Health and Nutrition Examination Survey guide book (KNHANES V-VI 2010-2013). Cheongju: Korea Centers for Disease Control and Prevention; 2013.
8. Kuklina EV, Carroll MD, Shaw KM, Hirsch R. Trends in high LDL cholesterol, cholesterol-lowering medication use, and dietary saturated-fat intake: United States, 1976-2010. NCHS Data Brief 2013;(117):1-8. PMID: 23759124.

9. Pencina MJ, Navar-Boggan AM, D'Agostino RB Sr, Williams K, Neely B, Sniderman AD, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med 2014;370:1422-1431. PMID: 24645848.


10. Centers for Disease Control and Prevention (CDC). Trends in intake of energy and macronutrients--United States, 1971-2000. MMWR Morb Mortal Wkly Rep 2004;53:80-82. PMID: 14762332.


11. Lofgren I, Greene G, Schembre S, Delmonico MJ, Riebe D, Clark P. Comparison of diet quality, physical activity and biochemical values of older adults either reporting or not reporting use of lipid-lowering medication. J Nutr Health Aging 2010;14:168-172. PMID: 20126967.



12. Lytsy P, Burell G, Westerling R. Cardiovascular risk factor assessments and health behaviours in patients using statins compared to a non-treated population. Int J Behav Med 2012;19:134-142. PMID: 21494820.


13. Sugiyama T, Tsugawa Y, Tseng CH, Kobayashi Y, Shapiro MF. Different time trends of caloric and fat intake between statin users and nonusers among US adults: gluttony in the time of statins? JAMA Intern Med 2014;174:1038-1045. PMID: 24763487.



14. Hagstromer M, Oja P, Sjostrom M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr 2006;9:755-762. PMID: 16925881.


15. Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381-1395. PMID: 12900694.


16. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157-163. PMID: 14726171.


17. Mann DM, Allegrante JP, Natarajan S, Montori VM, Halm EA, Charlson M. Dietary indiscretion and statin use. Mayo Clin Proc 2007;82:951-957. PMID: 17673064.


Figure┬Ā1
Trends of adjusted* physical activity among adults with dyslipidemia over study period, 2010-2013 KNHANES. *Adjusted for sex, age category, level of education, mariatal status, body mass index, and diagnosis of diabetes. ŌĆĀP for trend were using general linear model in complex sample analysis.

Table┬Ā1
Weighted proportion of adults with dyslipidemia* and lipid-lowering drug users, 2010ŌĆō2013 KNHANES
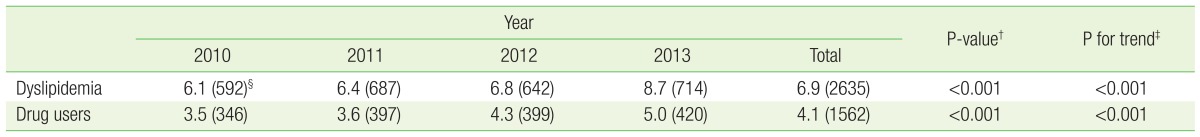
Values are presented as % (number).
KNHANES, Korea National Health and Nutrition Examination Survey.
*Reported the diagnosis of dyslipidemia, 2010ŌĆō2013 KNHANES. ŌĆĀCalculated using chi-square tests in complex sample analysis. ŌĆĪCalculated using linear-by-linear association in complex sample analysis. ┬¦Unweighted sample number.
Table┬Ā2
Characteristics of lipid-lowering drug users and non-users among Korean adults with dyslipidemia
- TOOLS







