The Relationship between Smoking and Unhealthy Weight Control Behaviors among Korean Adolescents: The Tenth Korea Youth Risk Behavior Web-Based Survey, 2014
Article information
Abstract
Background
Adolescent smoking is positively related to weight control attempts, especially by unhealthy methods. The co-occurrence of smoking and unhealthy weight control behaviors may cause serious health problems in adolescents. This study examined the relationship of smoking with unhealthy weight control behaviors among Korean adolescents.
Methods
This cross-sectional study involved 31,090 students of grades 7 to 12, who had tried to reduce or maintain their weight during the 30 days prior to The Tenth Korea Youth Risk Behavior Web-based Survey, 2014. Data on height, weight, weight control methods, smoking, alcohol intake, living with one's family, and perceived economic status were obtained through self-report questionnaires. ‘Unhealthy weight control behaviors’ were subcategorized into ‘extreme weight control behaviors’ and ‘less extreme weight control behaviors.’
Results
The smoking rates were 13.3%±0.4% in boys and 3.8%±0.2% in girls. Current smokers were more likely to engage in extreme weight control behaviors (odds ratio [OR], 1.47; 95% confidence interval [CI], 1.09 to 2.00 in boys, and OR, 2.05; 95% CI, 1.59 to 2.65 in girls) and less extreme weight control behaviors (OR, 1.23; 95% CI, 1.07 to 1.40 in boys, and OR, 1.47; 95% CI, 1.22 to 1.76 in girls) compared to non-smokers among both boys and girls.
Conclusion
Current smoking is independently related to a high likelihood of engaging in unhealthy weight control behaviors among Korean adolescents. This relationship is stronger for girls than for boys. Extreme weight control behaviors have a stronger relationship with current smoking than less extreme weight control behaviors.
INTRODUCTION
Health risk behaviors established during adolescence often have lasting negative effects on health across the lifespan.12) Smoking is one of the most serious risk behaviors initiated in adolescence. The smoking rate among Korean adolescents was reported to be 9.2% (14.0% in boys, 4.0% in girls) in 2014, which meant that one out of 10 adolescents were currently smoking.3) Not only does adolescent smoking lead to an increased risk of smoking-related diseases, but it also promotes adoption of other health risk behaviors such as the use of alcohol or illegal drugs.4) The co-occurrence of two or more risk behaviors may produce more deleterious effects on adolescent health.
Since adolescents are conscious of their outward appearance and body image, they are likely to attempt weight control. The Korea Youth Risk Behavior Web-based Survey (KYRBS), 2014, showed that 44.4% of Korean adolescents (33.4% of boys, 56.4% of girls) had tried to lose or maintain weight during the previous 30 days.3) Body weight perception is known to function as a mediator between body mass index (BMI) and weight control behaviors in adolescents.5) Adolescents with body shape distortion may resort to unnecessary weight control regardless of their body weight. Moreover, unhealthy weight control behaviors (UWCBs) such as using laxatives or diuretics, taking diet-pills, and vomiting after meals can provoke health problems even in healthy adolescents. 6) Engaging in excessive weight control behaviors with potentially harmful effects is considered a common health risk behavior in adolescents.7)
Many studies have evaluated the relationship between smoking and weight control behaviors in adolescents. Most available studies report a positive relationship between smoking and weight control behaviors among adolescents, and this relationship is stronger for girls than for boys. Additionally, extreme weight control behaviors (EWCBs) are more strongly related to adolescent smoking than less extreme weight control behaviors (LWCBs).789) A positive relationship between smoking and weight control behaviors among adolescents may indicate that some adolescents initiate smoking to control body weight. However, this may also be explained by the probability that both smoking and dieting behaviors co-exist in a cluster of adolescent risk behaviors.91011)
Even though it is known that the co-occurrence of smoking and UWCBs may cause serious health problems in adolescents, there is insufficient research regarding the relationship between smoking and weight control behaviors among Korean adolescents. Thus, this study was conducted to examine the relationship of current smoking with UWCBs among Korean adolescents who had attempted weight control during the previous 30 days. We expected that EWCBs such as taking diet-pills, using laxatives or diuretics, and vomiting after meals would be more strongly related to smoking compared to other weight control behaviors.
METHODS
1. Study Subjects
This study was based on data from the KYRBS, 2014, conducted by the Korea Centers for Disease Control and Prevention (KCDC). It is an anonymous, self-administered, web-based survey using a stratified, multistage, cluster-sampling design to monitor health risk behaviors among Korean adolescents from the 7th to 12th grade. A total of 74,167 students from 400 middle schools and 400 high schools were selected for the survey. Among them, 72,060 students from 799 schools participated in the survey (response rate, 97.2%).3) Students whose information for age, height and/or weight was missing (n=2,101) were excluded from the study, leaving 69,959 students. Finally, we analyzed the data of 31,090 students, who responded that they had, on their own initiative, tried to reduce or maintain their body weight during the 30 days prior to the survey. The study protocol was approved by the institutional review board of Inje University Seoul Paik Hospital (IRB no. IIT-2015-378).
2. Measurements
We defined current smokers and current drinkers based on the KCDC's criteria. Current smokers and current drinkers were subjects who reported smoking at least one cigarette during the past 30 days and subjects who reported having at least one drink of alcohol during the past 30 days, respectively.3)
Weight status was assessed on the basis of the 2007 Korean National Growth Charts for Korean children and adolescents.12) BMI was calculated from self-reported weight (kg) and height (m). We classified weight status into obese (≥95th BMI percentile for age and sex or ≥25 kg/m2), overweight (<95th but ≥85th BMI percentile for age and sex), normal weight (<85th but ≥5th BMI percentile for age and sex), and underweight (<5th BMI percentile for age and sex). Subjects were asked to rate how they perceived their own body shape on a scale from ‘very thin,’ through ‘somewhat thin,’ ‘average,’ and ‘somewhat obese’ to ‘very obese.’
Respondents who had attempted to reduce or maintain their body weight during the past 30 days were asked to report what methods they had used to control their body weight during that period. The queried weight control methods were (1) regular exercise, (2) eating less food, (3) one-food diet, (4) fasting, (5) dietary supplements, (6) Korean herbal medicine, (7) prescription diet-pills, (8) nonprescription diet-pills, (9) laxatives or diuretics, and (10) vomiting after meals. UWCBs were subcategorized into EWCBs and LWCBs. EWCBs included prescription diet-pills, nonprescription diet-pills, laxatives or diuretics, and vomiting after meals, and LWCBs included one-food diet, fasting, dietary supplements, and Korean herbal medicine. Perceived economic status, whether living with family, and residential area were also evaluated as covariates.
3. Statistical Analyses
All the analyses were performed after accoungting for stratification, cluster, and sample weight based on the guidelines for use of the KYRBS's raw data. Data were expressed as mean±standard error (SE) or percentage±SE. The simple relationships between current smoking and weight control behaviors were assessed using the chi-square test. Logistic regression analyses were used to estimate the odds ratios (ORs) and 95% confidence intervals (CIs) between current smoking and weight control methods. Statistical analyses were performed using PASW SPSS ver.18.0 (SPSS Inc., Chicago, IL, USA). A P-value <0.05 was considered statistically significant.
RESULTS
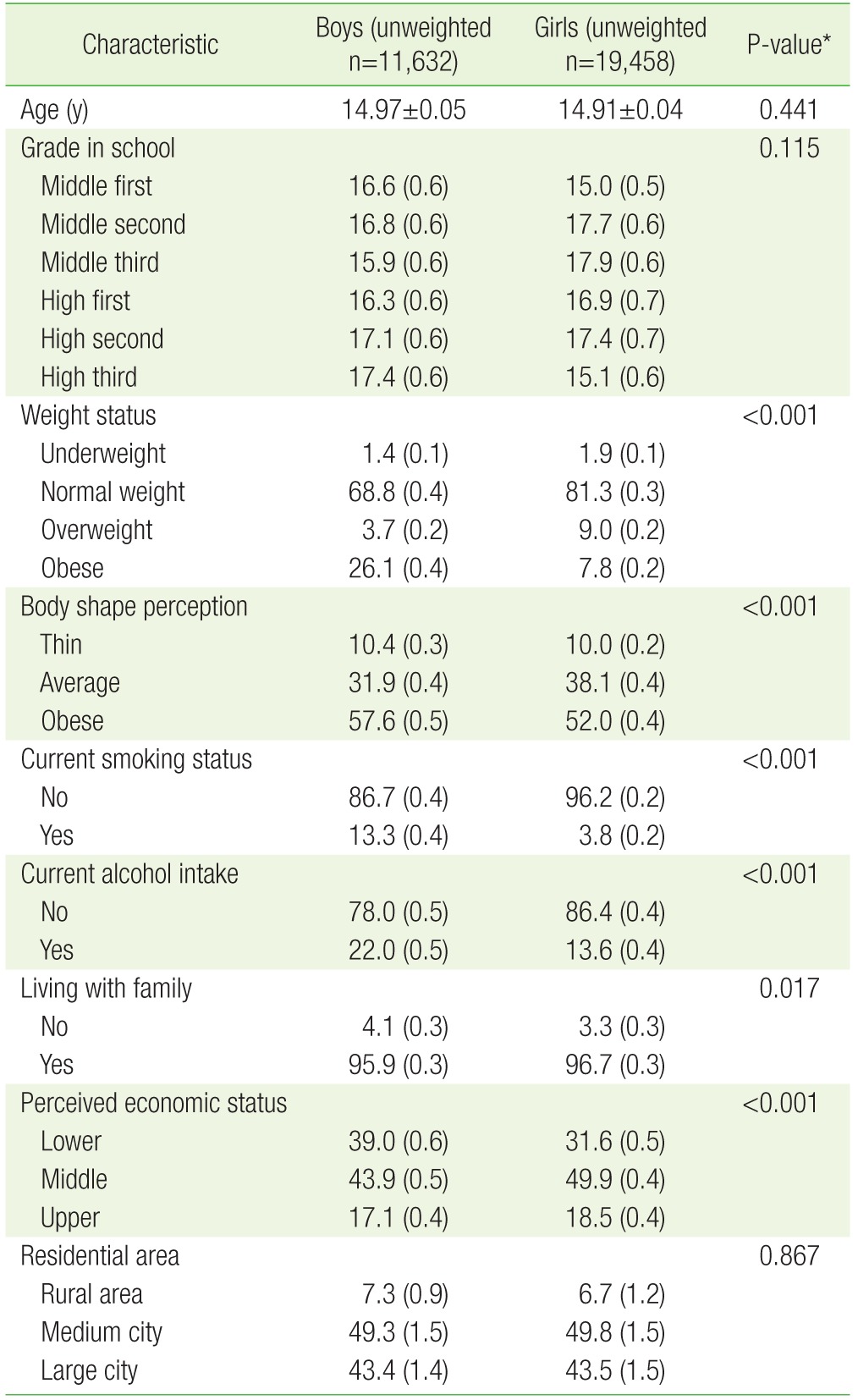
The study subjects were Korean adolescents who responded in the KYRBS, 2014, that they had tried to control their body weight during the past 30 days. The general characteristics of the study subjects are presented in Table 1. The mean ages of boys and girls were 14.97±0.05 years and 14.91±0.04 years, respectively. The smoking rates based on the KCDC's definition were 13.3%±0.4% in boys and 3.8%±0.2% in girls. Obesity was diagnosed according to the BMI criteria in 26.1%±0.4% in boys and 7.8%±0.2% in girls but more than half of both boys and girls perceived their own body shape as obese.
The frequencies of weight control methods that they had used to control their body weight during the 30 days prior to the survey are shown in Table 2. The most commonly used methods for weight control were regular exercise in boys and eating less food in girls. Among both boys and girls, current smokers engaged more frequently in EWCBs (5.8%±0.6% vs. 3.6%±0.2%, P-value<0.001 in boys; 15.1%±1.3% vs. 5.2%±0.2%, P-value<0.001 in girls) and LWCBs (21.9%±1.0% vs. 17.2%±0.4%, P-value<0.001 in boys; 38.2%±1.8% vs. 22.6%±0.3%, P-value<0.001 in girls) compared to non-smokers. The frequencies of individual weight control behaviors stratified by current smoking status were assessed. It was seen that, among boys, current smokers attempted all the queried weight control methods except regular exercise and use of Korean herbal medicine significantly more frequently than non-smokers. Among girls, current smokers attempted all the queried weight control methods except regular exercise more frequently, compared to non-smokers.
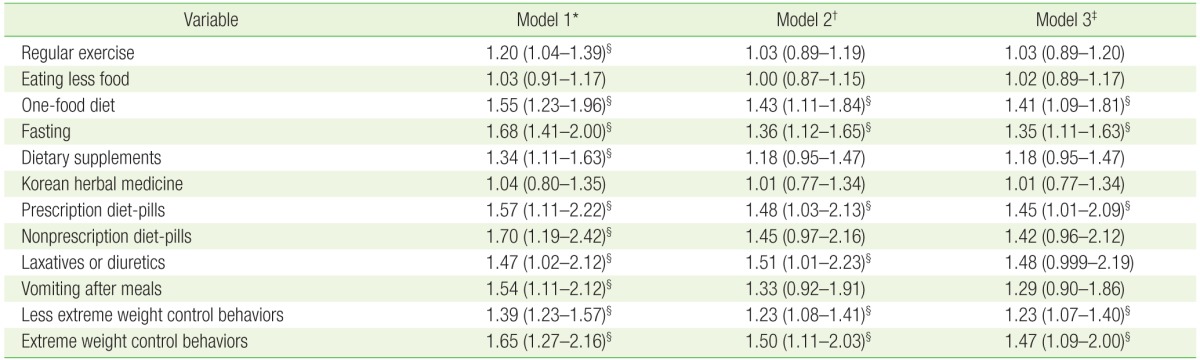
Adjusted ORs and 95% CIs of current smoking on EWCBs and LWCBs were estimated using logistic regression analyses. Current smokers were more likely to engage in EWCBs (OR, 1.47; 95% CI, 1.09 to 2.00 in boys; OR, 2.05; 95% CI, 1.59 to 2.65 in girls) and LWCBs (OR, 1.23; 95% CI, 1.07 to 1.40 in boys; OR, 1.47; 95% CI, 1.22 to 1.76 in girls) compared to non-smokers among both boys and girls. Adjusted ORs and 95% CIs of current smoking on individual weight control methods were also obtained. Among boys, current smokers were more likely to attempt a one-food diet (OR, 1.41; 95% CI, 1.09 to 1.81), fasting (OR, 1.35; 95% CI, 1.11 to 1.63), and use of prescription diet-pills (OR, 1.45; 95% CI, 1.01 to 2.09) compared to non-smokers (Table 3). Among girls, current smokers were more likely to attempt a one-food diet (OR, 1.45; 95% CI, 1.12 to 1.88), fasting (OR, 1.88; 95% CI, 1.52 to 2.33), use of dietary supplements (OR, 1.30; 95% CI, 1.04 to 1.62), use of prescription diet-pills (OR, 2.10; 95% CI, 1.34 to 3.30), use of nonprescription dietpills (OR, 2.23; 95% CI, 1.56 to 3.19), use of laxatives or diuretics (OR, 2.15; 95% CI, 1.38 to 3.33), and vomiting after meals (OR, 2.15; 95% CI, 1.52 to 3.04) than non-smokers (Table 4).
DISCUSSION
This study was aimed at investigating the relationship between weight control behaviors and current smoking among Korean adolescents. We used data from the KYRBS, 2014, from subjects who had attempted weight control during the 30 days prior to the survey. We found that current smoking was independently related to engaging in UWCBs among Korean adolescents. This relationship was stronger for girls than for boys. EWCBs were more strongly related to current smoking than LWCBs. These findings were consistent with results of previous studies conducted in Western countries regarding the relationship between adolescent smoking and weight control behaviors.9)
In this study, subjects were asked to report all the methods that they had used to control their body weight during the past 30 days. Ten weight control behaviors were considered and categorized into healthy weight control behaviors, LWCBs and EWCBs with reference to the classifications of weight control behaviors in adolescents which were used by Eaton et al.,13) Johnson et al.,14) Neumark-Sztainer et al.,15) and Crow et al.16) Eaton et al.13) and Johnson et al.14) included exercise and eating less food, fewer calories, or foods low in fat among healthy weight control behaviors. Neumark-Sztainer et al.15) and Crow et al.16) included taking diet-pills, self-induced vomiting, using laxatives and using diuretics among EWCBs and included fasting and using food substitutes among LWCBs. One-food diet and using Korean herbal medicine were not investigated in previous studies, but were classified as LWCBs in this study. This classification may be controversial. However, there were no significant differences in study results, even if those methods were excluded from LWCBs.
It has been reported that while smoking is inversely related to body weight among adults, smoking has a positive association with body weight among adolescents.917) This may be because some overweight adolescents initiate smoking to control their body weight. Klesges et al.18) observed that almost 40% of seventh grade students at the Memphis city schools endorsed the belief that smoking could help control their body weight, and approximately 12% (8% of boys, 18% of girls) of the respondents with an active smoking history indicated that they smoked to control their body weight. Body weight perception rather than actual BMI predicts weight control behaviors in adolescents.19) Kim et al.5) reported that body weight perception was a potential mediator between BMI and UWCBs among Korean adolescents. Psychological factors including body shape dissatisfaction and the belief that smoking supports weight control are involved in the relationship between adolescent smoking and weight control.2021) There are differences in psychological aspects related to smoking and weight control between boys and girls. These gender differences may plausibly explain the finding that the relationship between smoking and UWCBs is stronger for girls than for boys.
Adolescent smoking is regarded as a problem behavior violating social norms in Korea, such that it is illegal to sell tobacco to youth under the age of 19. Regular smoking among adolescents is related to abuse, family violence, depressive symptoms, and stressful life events,22) and is likely to cluster with other problem behaviors such as drinking, drug use, sexual intercourse, violence or delinquency.41123) Furthermore, smoking at an early age may provide a gateway to a wider range of risk behaviors.242526) According to Jessor's Problem Behavior Theory, risk behaviors in adolescence co-occur as a result of shared common underlying causes.27) EWCBs are adopted so as to achieve rapid weight reduction without requiring constant effort, despite the risk of harmful side effects; they should therefore also be considered risk behaviors that are common among adolescents who have a propensity for risk-taking and sensation-seeking.28) Our finding that current smokers are more likely to engage in UWCBs compared to non-smokers could be interpreted as clustering of risk behaviors.9)
We acknowledge several limitations of this study. It is a cross-sectional study using the KYRBS data that does not address temporal or causal inferences. We defined current smokers as subjects who reported smoking at least one cigarette during the past 30 days. Even though this definition is based on the KCDC's criteria and has been widely used, it does not reflect the heterogeneity of adolescent smoking behavior. 29) Moreover, electronic cigarette use is increasing rapidly among Korean adolescents30) but was not considered in this study. Weight status was assessed based on self-reported anthropometric data in this study. Using self-reported weight and height could lead to a considerable underestimation of obesity prevalence. However, we felt that relying on self-reported anthropometric data would not affect the results of our study because its aim was to evaluate the relationship between smoking and weight control behaviors rather than that between smoking and obesity. Despite these limitations, our study is of value, being the first study to evaluate the relationship between smoking and UWCBs among Korean adolescents using a large nationally representative sample of middle and high school students.
Adolescence is a critical period for the establishment of health risk behaviors such as smoking, drinking, lack of exercise, and skipping breakfast. Adolescent risk behaviors are likely to cluster, further threatening adolescent health. Our study showed that, among Korean adolescents, current smokers were more likely to engage in UWCBs such as taking diet-pills, using laxatives or diuretics, and vomiting after meals, compared to non-smokers. This result suggests that psychosocial factors underlying clustering of smoking and UWCBs should be considered in order to develop and implement more effective health promotion programs for Korean adolescents.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.