The Effect of Having a Regular Doctor as a Primary Care Provider on Emergency Room Utilization in South Korea
Article information
Abstract
Background
Because primary care is the cornerstone of an effective health care system, many developed countries have striven to establish and strengthen their primary care systems. However, the primary care system in South Korea is not well established, and primary care research is still in its infancy. This study aimed to show the benefits of regular doctors as primary care providers in South Korea by analyzing the effect of regular doctor visits on emergency room (ER) visits.
Methods
We analyzed cross-sectional data on 11,293 adults aged 18 years and over collected from the 2013 Korea Health Panel Survey (beta version 1.0). We classified those participants with and without regular doctors into the treatment and control groups, respectively, and estimated the average treatment effect (ATE) of having a regular doctor on ER visits. We used counterfactual framework and propensity score analysis to adjust for unevenly distributed confounding covariates between treatments and control groups.
Results
The estimated conditional ATE of a regular doctor on ER visits was statistically insignificant in the general population (-0.4%; 95% confidence interval [CI], -2.0 to 1.2) and in the subgroup of patients with hypertension (-1.8%; 95% CI, -4.5 to 0.9). However, in patients with diabetes mellitus (DM), the estimated ATE was statistically significant (-5.0; 95% CI, -9.2 to -0.7).
Conclusion
In the total study population, having a regular doctor did not result in a significant difference in ER visits. However, there was a decrease in ER visits in patients with DM in South Korea.
INTRODUCTION
Because primary care is a cornerstone of effective health care systems, many developed countries have striven to establish and strengthen their primary care systems. However, the primary care system in South Korea is not yet well-established. The Korean health care system is market-oriented and focused on treatment rather than prevention, which encourages further diagnosis and utilization of the large hospital sector. This leads to medically undesirable and unnecessary health care utilization and increased costs.1) The recent outbreak of Middle East respiratory syndrome coronavirus in South Korea was also related to the failure of the Korean primary care system. Therefore, strengthening of the primary care is essential for solving many health care problems in South Korea.
Primary care is defined as care that is provided by regular doctors as a usual source of care (USC), and which is characterized by comprehensive first contact, person-focused continuity, and care coordination across health care providers.2) Internationally, a large body of research has shown the benefits of USC. Having a USC may provide more effective and equitable care,3) reduce health care costs,4) contribute to increased vaccination coverage,5) and result in better health outcomes.67) However, research related to USC in South Korea is just beginning compared to the large body of international research.8910)
The purpose of this study was to assess the benefits of a regular doctor as a USC by analyzing the effect of having a regular doctor on reducing emergency room (ER) utilization in South Korea and to provide implications for policymakers in terms of strengthening primary care in South Korea.
METHODS
1. Resources and Subjects
This study analyzed data from 11,293 adults aged 18 years and over collected from the 2013 Korea Health Panel Survey (KoHPS, beta version 1.0) after excluding seven respondents who had missing values in questions related to income and USC out of 11,300 total respondents who replied to the secondary research. Since 2012, the KoHPS has included questions related to a regular doctor as a USC, which has enabled studies related to regular doctors. In the survey questionnaire, those who responded “Yes” to the question “Do you have a doctor you usually visit if you are sick or in need of a medical check-up or advice?” was defined as having a regular doctor.
2. Analysis
1) Research variables
To analyze the treatment effect of having a regular doctor on ER visits, having a regular doctor and ER visits in the past year were considered the treatment and outcome variables, respectively. Participants with and without a regular doctor were classified into treatment and control groups, respectively.
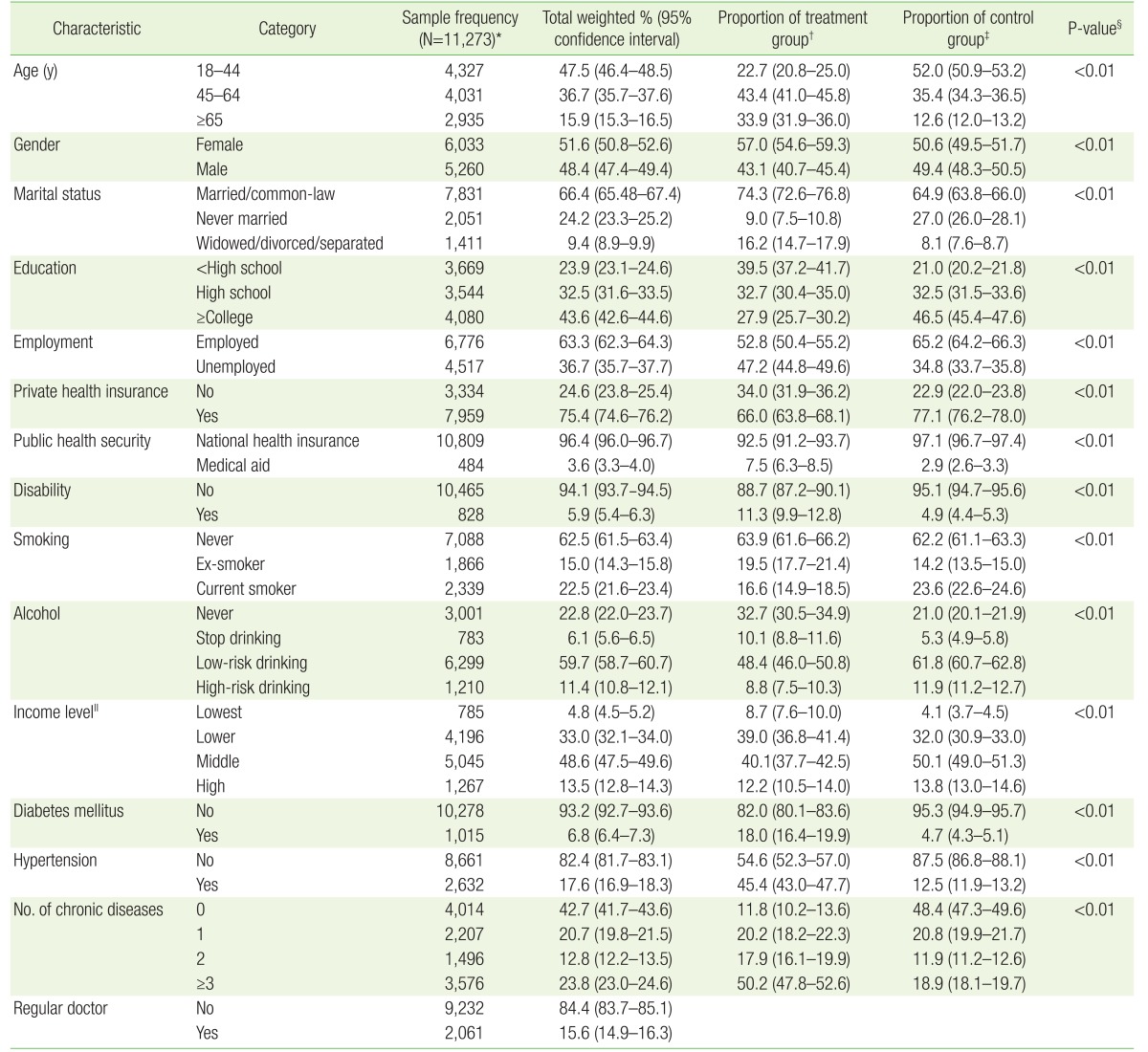
To adjust for confounding covariates, the sociodemographic and health-related characteristics of each respondent were included in the analysis, including age, gender, marital status, education level, employment status, private health insurance, type of health insurance, disability, smoking, alcohol intake, income level, and the number of chronic diseases. Regarding the variable of income level, the bottom 10% of household income was defined as the lowest, between 10% and 50% as the lower, between 50% and 90% as the middle, and the top 10% as the high. Alcohol intake of more than an average of seven drinks daily for men and five drinks daily for women at least twice a week—regardless of the kind of alcohol—was defined as the high-risk drinking (Table 1).
2) Statistical analysis
In observational studies such as the current study, differences in the distribution of observed baseline covariates between treatment and control groups may occur. (Table 1) This selection bias prevents justifiable causal inferences without controlling for the bias. To estimate the causal effect by adjusting for unbalanced confounding covariates between treatment and control groups, this study used a counterfactual framework (also known as potential outcome framework) and propensity score (PS) analysis.1112) In the PS analysis, the probability of treatment conditional on baseline confounding covariates was first estimated and these conditional probability estimates were used for estimation of treatment effect.1314) We estimated potential-outcome means (POMs) and average treatment effect (ATE) in the general population, patients with hypertension, and those with diabetes mellitus (DM) using an augmented inverse-probability-weighted (AIPW) estimator that combined elements of regression adjustment on PS and PS weighting estimation among several PS analysis methods.15) In the counterfactual framework, each subject had two potential outcomes. One outcome would manifest if the subject were exposed to the treatment and another outcome would manifest if the same subject were exposed to the control. The difference between these two means of potential outcomes was defined as the ATE. We calculated PS using logistic regression analysis with baseline covariates and applied to the AIPW estimator. We used Stata/IC ver. 14.0 (Stata Corp., College Station, TX, USA) for analysis, applied cross-sectional weights, and estimated the confidence intervals using robust standard error.
RESULTS
1. Baseline Characteristics of the Study Population
Overall, 15.9% (95% confidence interval [CI], 15.3 to 16.5) of the study population was 65 years of age and over, 51.6% (95% CI, 50.8 to 52.6) were women, 15.6% (95% CI, 14.9 to 16.3) had a regular doctor, 6.8% (95% CI, 6.4 to 7.3) had DM, 17.6% (95% CI, 16.9 to 18.3) had hypertension, and 23.8% (95% CI, 23.0 to 24.6) had more than three chronic diseases (Table 1).
2. The Effect of Having a Regular Doctor on Emergency Room Visits
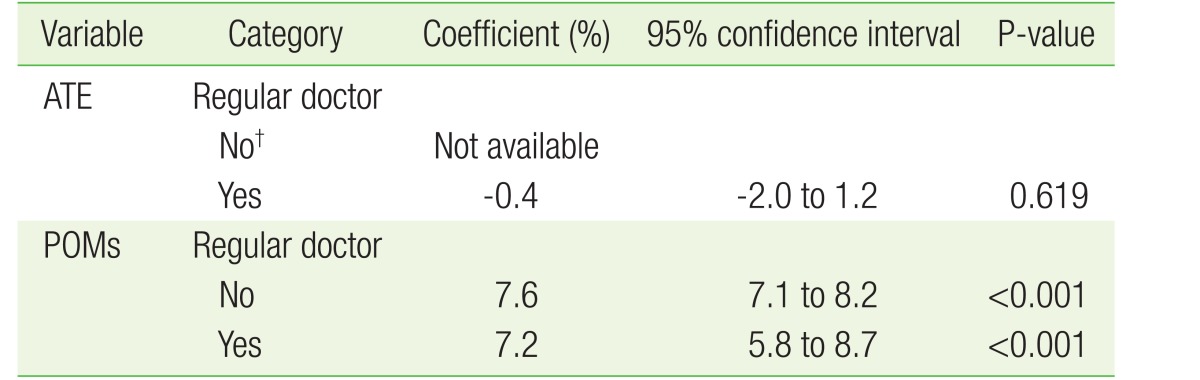
In the general population, the POMs of ER visit rates of the treatment and control groups were 7.2% and 7.6%, respectively. The group with a regular doctor had a 0.4% lower visit rate than the control group, but the difference in 95% CI between the groups was not statistically significant (ATE, –0.4%; P-value=0.619) (Table 2).
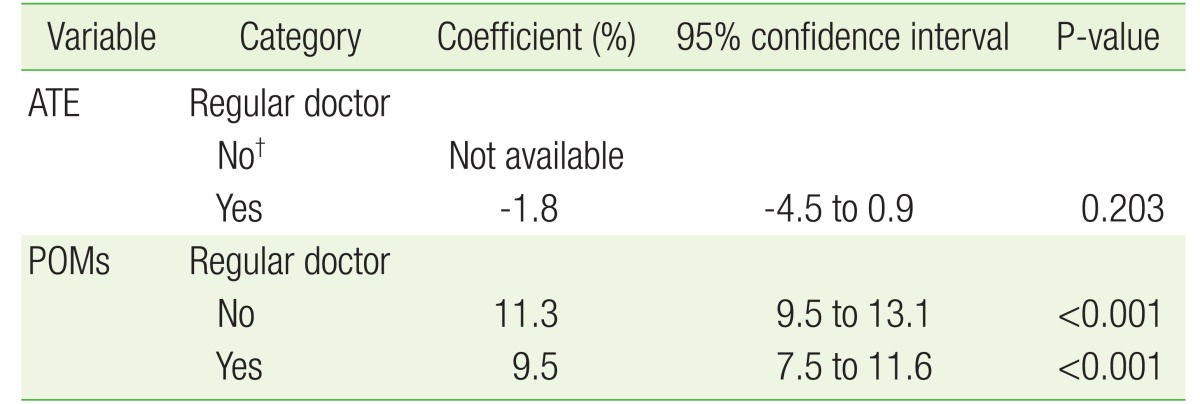
In patients with hypertension, the POMs for ER visit in the treatment and control groups were 9.5% and 11.3%, respectively. The group with a regular doctor had a 1.8% lower ER visit rate than the control group, but the differences in 95% CI also did not differ significantly (ATE, –1.8%; P-value=0.203) (Table 3).
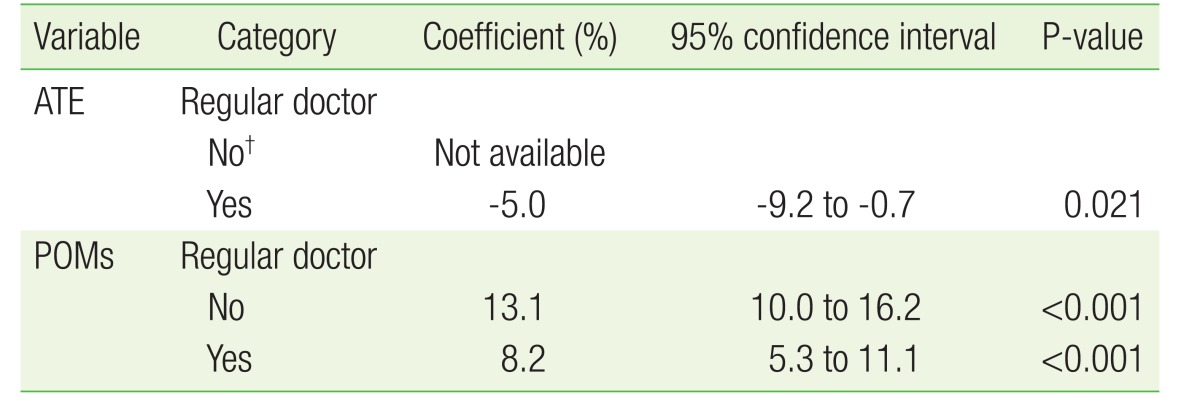
In patients with DM, the POMs of ER visit rates in the treatment and control groups were 8.2% and 13.1%, respectively. The group with a regular doctor had a 5.0% lower ER visit rate than the control group, and the differences in 95% CI were statistically significant (ATE, –5.0%; P-value=0.021) (Table 4).
DISCUSSION
This study used 2013 KoHPS (beta version 1.0) data to analyze the effect of having a regular doctor as a USC on ER visits.
The rates of having a regular doctor in countries with well-established primary care systems, were 88% in Australia, 84% in Canada, 92% in Germany, 100% in the Netherlands, 89% in New Zealand, 89% in the United Kingdom, and 80% in the USA.16) These rates are much higher than the 15.6% rate in South Korea observed in this study.
Having a USC has been associated with improved receipt of preventive services (pap smear, clinical breast exam, mammogram, and prostate cancer screening) compared with no USC.17181920) Comparison of a regular doctor and having a regular site as USC revealed that a regular doctor was more effective than a regular site for providing blood pressure checks, cholesterol level checkups, and influenza vaccines.21)
Countries with strong primary care may have lower overall health care costs and healthier populations.22) Strong primary care has been related to adequate primary care physician supply and long-term relationships between primary care physicians and decreased hospitalization for chronic ambulatory care-sensitive conditions.23)
Long-term relationships were also related to substantially lower costs of inpatient and outpatient care.24) Patients with insufficient USCs, particularly the uninsured and Medicaid enrollees, have a tendency to rely on the ER.25) And patients who are dissatisfied with their USC or experience access barriers to their USC more likely to have a non-urgent ER visit.26) Domestic studies also indicate that participants with a USC have higher smoking cessation rates, are more often advised to stop smoking,27) and show significantly reduced unmet medical needs.28)
The current study has several limitations. First, although the counterfactual framework and PS analysis allow justifiable causal inferences by adjusting for sample selection bias, it is not complete without controlling for the problem of endogeneity. Endogeneity is kind of omitted variable bias that comes from unobserved confounding variables. In our study, participants with poor health may have had a higher probability of having a regular doctor as well as a higher rate of ER visits. Thus, the insignificant ATE in the general population and patients with hypertension may be due to this problem. In order to make more causal inferences, this problem should be controlled. Second, we did not consider the fact that the qualities and characteristics of the regular doctor such as comprehensiveness, care coordination, and individual-focused continuity may affect ER visits. Therefore, further research on the effect of these characteristics is required.
There are few studies in Korea on visits to the ER when there is a USC available.2930) Chai et al.29) used annual data from the 2009–2011 KoHPS.
In that study, logistic regression analysis for ER use in the research group revealed that the group without USC visited the ER 0.78 times less often.29) Subjects with a USC or with chronic diseases may more often visit the ER because of concerns about their health or due to poor health conditions. Furthermore, limited access to primary care leads to more frequent ER visits.31)
Lee et al.30) performed a panel analysis utilizing data from the 2012-2103 KoHPS, showing the effect of having a regular doctor in adult patients with DM on ER visits. The relationship between having a USC and ER visits in patients with DM varied depending on the USC characteristics (medical institutions versus physician), but having a regular doctor was related to fewer ER visits. After controlling confounding variables (income level, health conditions, medical security type), the panel analysis showed that having a regular doctor reduced the incidence of ER visits.30)
There are some limitations to this study. We did not reach the perfect causal inference because of unobserved Heterogeneity and Endogeneity partly. In the overall study population, having a regular doctor resulted in no difference in ER visits. However, there was a decrease in ER visits among patients with DM. For a more complete causal inference, studies that control unobserved Heterogeneity and Endogeneity in the future need to proceed.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.