 |
 |
- Search
| Korean J Fam Med > Volume 41(1); 2020 > Article |
|
Abstract
Background
Methods
Results
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported. Seoul National University Hospital had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit for publication.
SUPPLEMENTARY MATERIALS
Supplementary Table 1.
Supplementary Table 2.
Supplemental Figure 1.
Figure. 1.
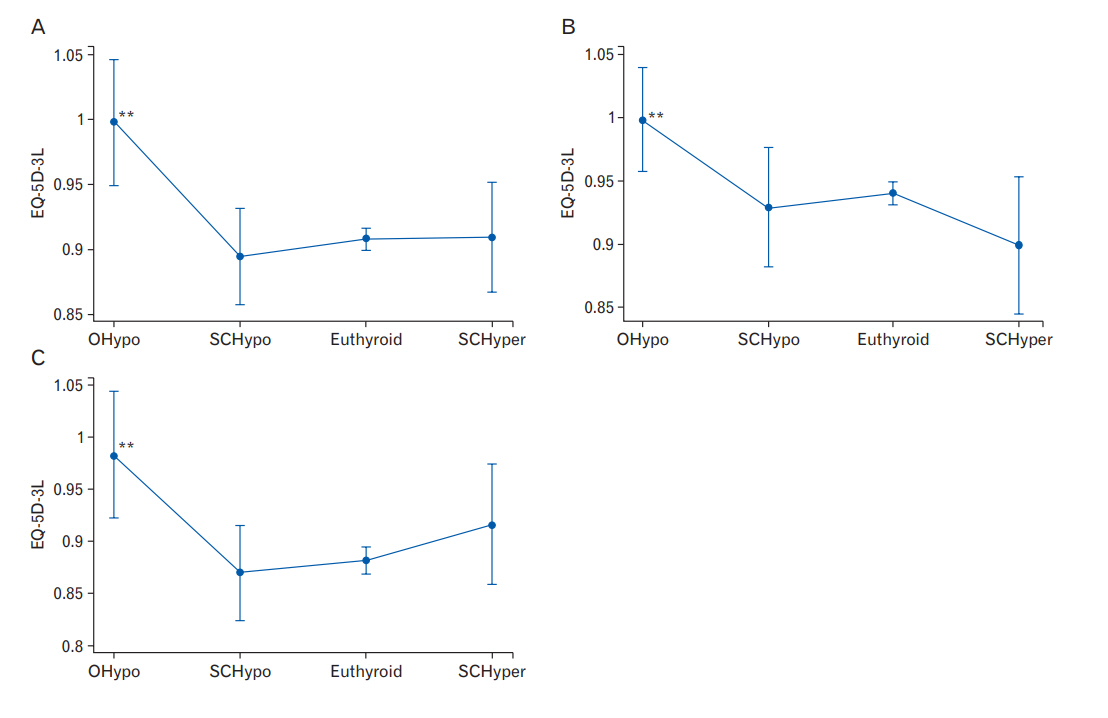
Table 1.
| Characteristic | Category | Overt hypothyroid | Subclinical hypothyroid | Euthyroid | Subclinical hyperthyroid | P-value |
|---|---|---|---|---|---|---|
| No. of participants | 10 | 31 | 987 | 32 | ||
| Age (y) | 65±3.9 | 66.1±4.6 | 65.4±3.8 | 65.5±4.9 | 0.778 | |
| Sex | Male | 4 (40.0) | 11 (35.5) | 510 (51.7) | 17 (53.1) | 0.296 |
| Female | 6 (60.0) | 20 (64.5) | 477 (48.3) | 15 (46.9) | ||
| Body mass index | Nonobese | 3 (30.0) | 22 (71.0) | 618 (62.6) | 17 (53.1) | 0.085 |
| Obese | 7 (70.0) | 9 (29.0) | 369 (37.4) | 15 (46.9) | ||
| Household income | Lower half | 6 (60.0) | 15 (48.4) | 614 (62.2) | 21 (65.6) | 0.450 |
| Upper half | 4 (40.0) | 16 (51.6) | 373 (37.8) | 11 (34.4) | ||
| Education | ≤6 y | 5 (50.0) | 14 (45.2) | 475 (48.1) | 17 (53.1) | 0.932 |
| >6 y | 5 (50.0) | 17 (54.8) | 512 (51.9) | 15 (46.9) | ||
| Employment status | Unemployed | 8 (80.0) | 18 (58.1) | 511 (51.8) | 16 (50. 0) | 0.301 |
| Employed | 2 (20.0) | 13 (41.9) | 476 (48.2) | 16 (50.0) | ||
| Smoking status | Nonsmoker | 7 (70.0) | 24 (77.4) | 520 (52.7) | 16 (50.0) | 0.034 |
| Current and past smoker | 3 (30.0) | 7 (22.6) | 467 (47.3) | 16 (50.0) | ||
| Drinking status | Nondrinker | 4 (40.0) | 17 (54.8) | 364 (36.9) | 12 (37.5) | 0.244 |
| Drinker | 6 (60.0) | 14 (45.2) | 623 (63.1) | 20 (62.5) | ||
| Physical activity* | Does not meet requirements | 2 (20.0) | 19 (61.3) | 481 (48.7) | 21 (65.6) | 0.033 |
| Meets requirements | 8 (80.0) | 12 (38.7) | 506 (51.3) | 11 (34.4) | ||
| Hypertension | No | 8 (80.0) | 18 (58.1) | 562 (56.9) | 17 (53.1) | 0.499 |
| Yes | 2 (20.0) | 13 (41.9) | 425 (43.1) | 15 (46.9) | ||
| Dyslipidemia | No | 8 (80.0) | 21 (67.7) | 713 (72.2) | 26 (81.3) | 0.595 |
| Yes | 2 (20.0) | 10 (32.3) | 274 (27.8) | 6 (18.7) | ||
| Diabetes | No | 8 (80.0) | 27 (87.1) | 813 (82.4) | 27 (84.4) | 0.900 |
| Yes | 2 (20.0) | 4 (12.9) | 174 (17.6) | 5 (15.6) | ||
| Hemoglobin level | 13.2±0.8 | 13.4±1.1 | 14.0±1.3 | 13.9±1.3 | 0.011 | |
| Thyroid peroxidase antibody level† | Normal | 8 (80.0) | 27 (87.1) | 906 (91.8) | 30 (93.8) | 0.422 |
| High | 2 (20.0) | 4 (12.9) | 81 (8.2) | 2 (6.2) | ||
| EuroQol three-level version | 0.9497±0.1029 | 0.8985±0.1004 | 0.9063±0.1397 | 0.8844±0.1316 | 0.599 |
Table 2.
Adjusted mean values calculated using linear regression after adjustments for age, sex, body mass index, income, education, employment status, smoking status, drinking status, physical activity, hypertension, dyslipidemia, diabetes, hemoglobin level, and thyroid peroxidase antibody level.
CI, confidence interval.
REFERENCES
- TOOLS
-
METRICS

- Related articles in KJFM
-
Association between Abdominal Obesity and Oxidative Stress in Korean Adults2019 November;40(6)
Association between C-Reactive Protein and Metabolic Syndrome in Korean Adults2019 March;40(2)
The Association between Vitamin D and Health-Related Quality of Life in Korean Adults2016 July;37(4)






