Sickness Certification Behavior amongst Primary Care Physicians: A Descriptive Analysis of Indirect Measures Using the Theory of Planned Behavior
Article information
Abstract
Background
The provision of sick leave to patients in general practice often entails a complex decision-making process. Commonly, general practitioners believe that the act of providing sick leave can become confrontational. We assessed the intention, attitude, subjective norm, and perceived behavioral control of general practitioners in relation to sick leave provision at public health clinics in Malaysia.
Methods
A cross-sectional study design was implemented using data from 86 primary health care clinics in two states in Malaysia from February 2014 to March 2015. A questionnaire that comprised indirect measures were developed on the basis of the Theory of Planned Behavior. The questionnaire assessed several dimensions related to sickness certification provision viz., intention, attitude, subjective norm, and perceived behavioral control.
Results
The mean scores in this study revealed that physicians acknowledged that patient factors such as clinical symptoms (6.59±0.04), debilitating signs and symptoms of diseases (6.45±0.06), importance of illness recovery (6.07±0.07), and approval of employers (5.35±0.09) played an important role in their decision to provide sick leave.
Conclusion
The act of providing sickness certification to patients is a complex decision-making process. The findings of this study can be used to devise a targeted intervention to reduce the conflict that physicians face in issuing sick leaves.
INTRODUCTION
The need to provide patients with sick leaves is a decision most general practitioners (GPs) make on a daily basis [1-4]. Studies in various countries reported that physicians were reluctant to perform the role as a gatekeeper in the provision of sick leaves [3,5-14]. Physicians often face conflict with patients in the process of providing sick leaves, which ultimately leads to emotional strain at the workplace [5,6].
Sick leaves amounts to nearly 4.04 working days lost per worker in Malaysia [15]. This translates to a loss of more than US $2.04 billion in revenue to employers (Ringgit Malaysia 3.92 to US $1) [15]. These figures have increased when compared with the trends in previous years [16]. Approximately 591,199 man-hours were lost, amounting to 2.83% of the total working hours in a year [17]. Approximately US $2.30 billion was lost in 2012 because of the additional cost of labor and salary paid because of sick leaves [18,19]. Concurrently, similar trends were observed in sick leave practices in the United Kingdom and other European countries [1,4,6-10,12,13,20]. Current circumstances create great potential for sickness certification abuse, thus necessitating an urgent need for intervention [1-6].
This study focused on a descriptive analysis of the beliefs (indirect measures) that control sick leave-prescribing behavior among GPs. These findings were derived from a wider study that assessed sickness certification behavior among GPs in Malaysia [21]. The objective of this study was to identify areas that could be explored as avenues for targeted intervention to improve sick leave practices among GPs.
METHODS
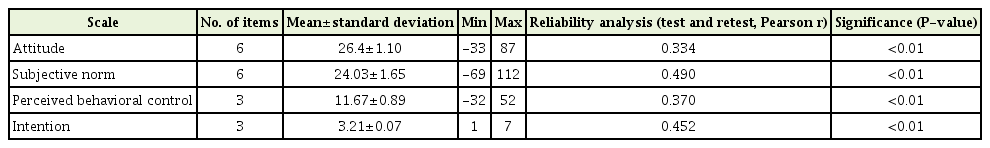
This cross-sectional study was conducted within two states (Negeri Sembilan and Selangor) in Peninsular Malaysia to represent both urban and rural population distributions across the country. A crosssectional study design was conducted using data from 86 primary health-care clinics from February 2014 to March 2015. A total of 329 primary care physicians (of the 666 physicians who were invited to participate in the study) were recruited. No details or demographics of non-responders were collected for this study. Standard guidelines for the Theory of Planned Behavior were used to generate and calculate all indirect measures in the questionnaire [22,23]. The intention related to a particular behavior is governed by three main constructs, namely attitude, subjective norm, and perceived behavioral control (PBC) [1]. The questions for all three constructs followed a 7-point extremely undesirable/desirable and not important/important dimension. The mean scores for intention ranged from 1 (strongly disagree) to 7 (strongly agree). The composite scores for attitude and subjective norm ranged from -126 to 126. The composite scores for PBC ranged from -63 to 63. The reliability of the constructs was satisfactory as determined by a statistical significance of P<0.01 using the Pearson correlation analysis (Table 1).
RESULTS
1. Intentions
The mean scores for the three intention items were 3.71±0.11, 3.04±0.09, and 2.87±0.09. Overall, the primary care physicians intended to provide sickness leaves for patients (3.21±0.07; range, 1 to 7).
2. Attitude toward Providing Sickness Certification to Patients
Most GPs valued the idea of providing sickness certification according to the condition of the patient determined through a clinical assessment (6.59±0.04). They also strongly believed that sickness certification should be provided to patients to allow them to recover from their illness (6.07±0.07). However, they show slight hesitation in providing sickness certification to patients because it promotes sickness leaveseeking behavior (5.13±0.10). Physicians appeared to be ambivalent toward the decision to provide sickness certification on the basis of the behavior of patients toward them (3.97±0.12). The GPs were uncertain about the genuine intention of a sickness leave request (4.21±0.10) and the reduction of the patient’s work productivity caused by sick leave (3.77±0.10). Overall, GPs had a moderate and positive attitude toward providing sickness certification to patients (26.4±1.10; range, -33 to 87).
3. Subjective Norm
The physicians believe that the approval of their patients (4.81±0.09), superiors (5.13±0.09), health managers (4.78±0.10), and employers (5.35±0.09) were valuable to them. However, they were ambivalent on whether organizational norms influence their decision to provide sickness leaves to patients (3.96±0.10). The role of colleagues in the sickness leave provision is least valued (3.29±0.10). On the whole, physicians had a moderately high and positive subjective norm (24.03±1.65; range, -69 to 112).
4. Perceived Behavioral Control over Providing Sickness Certification to Patients
Most physicians believed that patient behavior while seeking sickness leave during a consultation can be an unpleasant situation (2.72±0.09). They also strongly feel that sickness certification should be given to deserving patients who present with debilitating signs and symptoms (6.45±0.06). They were uncertain if organizational pressure influenced their sickness leave provision behavior (3.82±0.11). Overall, physicians had a weak but positive PBC toward providing sickness certification to patients (11.67±0.89; range, -32 to 56).
DISCUSSION
This study investigated the sickness certification provision among GPs working in the Malaysian public health-care system. Previous research involving sickness certification in Malaysia appeared to focus on the issues related to counterfeit sickness certification, the loss of manhours, and the loss of revenue to replace diminished man-hours due to sickness certification [16,17,24]. However, a recently published article in Malaysia showed that the behavioral beliefs of GPs also influence sick leave provision [21]. The study identified attitudes and subjective norms as predictive factors that influence a physician’s decision to provide sick leave to patients [21].
Most primary care physician appear to adhere to the biomedical philosophy of medical consultation [22,23]. Hence, although the intention to provide sickness certification to patients was high, the intention of GPs to do so was governed by the detection of symptoms that matched the biological properties of an illness. This practice seems to be congruent with another study in Singapore where physicians appeared to prescribe sickness certification on the basis of the presenting illness of patients [25].
The physicians in this study also found that the act of providing sickness certification to patients can often be a challenging situation. Likewise, 6% of 31% of Swiss GPs disclosed that the act of prescribing sick leaves can be problematic [1]. In addition, 54% of the participants claimed that they had a dispute with the patient related to the need for sick leave [26]. Therefore, it was not surprising that a modest number of sick leaves in Switzerland were prescribed out of fear that the patient will resort to switching GPs if their requests were declined [26]. Similarly, in our study, the salient factor that determined the subjective norm construct to provide patients with sick leave was highly influenced by the patient’s approval of a primary care physician’s practice or consultation.
The indirect measures in this study were limited by the low test-retest reliability value (Pearson r correlation ranging from 0.33 to 0.49 with a P-value of <0.001) (Table 1). This result indicates that the variables assessed in the study contributed only moderately to the overall temporal stability of the questionnaire. Therefore, we hypothesized that the beliefs pertinent to sickness certification by GPs might be influenced by other latent variables not accounted for in this study.
The intention to provide sickness leave to a patient is a complex decision-making process made by a primary care physician on a routine basis. Steps should be taken to assess the role of the biopsychosocial model to help unravel other salient beliefs that can help to attenuate the conflict between physicians and patients during the act of providing a sickness certification.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
We thank the director general of health for allowing this publication. We thank the National Clinical Research Centre, Malaysia (NCRC), CRC Perak, and the staff of the State Health Office of Selangor and Negeri Sembilan for their assistance during the formation stage of the research.