The Impact of Depression on Cardiovascular Disease: A Nationwide Population-Based Cohort Study in Korean Elderly
Article information
Abstract
Background
Depression is suggested to be associated with cardiovascular disease, including ischemic heart disease and cerebrovascular disease. This study investigated the impact of depression on cardiovascular disease in the elderly population in Korea.
Methods
This retrospective cohort study was performed using the Senior Cohort database released by the Korean National Health Insurance Services from January 1, 2008 to December 31, 2012, or January 1, 2009 to December 31, 2013. The study group constituted participants newly diagnosed with depression, but not cardiovascular disease. The control group constituted participants with no past history of depression or cardiovascular disease, and were not diagnosed with depression during the follow-up period. During the 5-year follow-up period, development of ischemic heart disease or cerebrovascular disease was assessed. Depression and cardiovascular disease were identified using the International Classification of Diseases, 10th revision, Clinical Modification codes. The data was analyzed using Cox proportional hazards model.
Results
The hazard ratio (HR) between depression and ischemic heart disease was 1.38 (95% confidence interval [CI], 1.23 to 1.55) and the HR between depression and cerebrovascular disease was 1.46 (95% CI, 1.32 to 1.62), after adjusting all confounding variables.
Conclusion
Independent of other cardiovascular risk factors, depression increased the risk of ischemic heart disease by 38% and cerebrovascular disease by 46% among older adults in Korea. Since depression may increase the risk of cardiovascular disease, future research should focus on the diagnosis and prevention of cardiovascular disease in people with depression.
INTRODUCTION
Depression is one of the leading causes of ill health and disability worldwide. More than 300 million people are now living with depression, depicting an increase of more than 18% from 2005 to 2015 [1]. Cardiovascular disease, including ischemic heart disease and cerebrovascular disease, has been identified as a leading contributor to both mortality and disease burden globally [2]. In Korea, cardiovascular disease was the second (ischemic heart disease) and third (cerebrovascular disease) leading cause of death in 2016, after malignant neoplasm, leading to high morbidity and mortality [3]. Moreover, the World Health Organization (WHO) projects that depression and cardiovascular disease are expected to be the largest contributors to disease burden by 2030 [4].
The relationship between depression and cardiovascular disease has been constantly discussed, and it is thought to be bidirectional. There is mounting evidence indicating that depression increases the risk of cardiovascular disease [5,6]. Potential mechanisms that explain how depression affects cardiovascular disease include pathophysiological changes such as activation of hypothalamic-pituitary-adrenal axis (HPA axis) [7], autonomic nervous system disorder [8], platelet activation [9], endothelial dysfunction [10], and inflammatory processes [11]; and behavioral, lifestyle factors [12]. Management of cardiovascular disease focuses on traditional risk factors such as hypertension, diabetes mellitus, dyslipidemia, obesity, smoking, and physical inactivity. However, psychosocial factors are relatively neglected [13]. Since depression is a potential modifiable risk factor for cardiovascular disease, further research is required to establish the relationship between depression and cardiovascular disease.
Moreover, depression is closely related to sociocultural factors [14]. Cultural factors influence the process with which an individual conceptualizes, experiences, and presents depression. Help-seeking behaviors in depression are also influenced by cultural values. Compared to Western societies, Eastern societies such as Koreans, Chinese, and Japanese are more likely to deny symptoms of depression for fear of being stigmatized as mentally ill, and are more comfortable sharing somatic symptoms of depression [15,16]. Therefore, the impact of depression on cardiovascular disease may vary across cultures. There is a lack of evidence examining the effect of depression as an independent risk factor for cardiovascular disease in Korea. Therefore, this study investigated the impact of depression on cardiovascular disease using a large, nationwide, population based Senior Cohort data.
METHODS
1. Subjects
We conducted a retrospective cohort study using the Senior Cohort database released by the Korean National Health Insurance Services (NHIS-Senior). We selected the samples directly from the population database to prevent non-sampling errors. The database contains data for 558,000 individuals, with approximately 10% of the total population aged 60 years or older from 2002 to 2013.
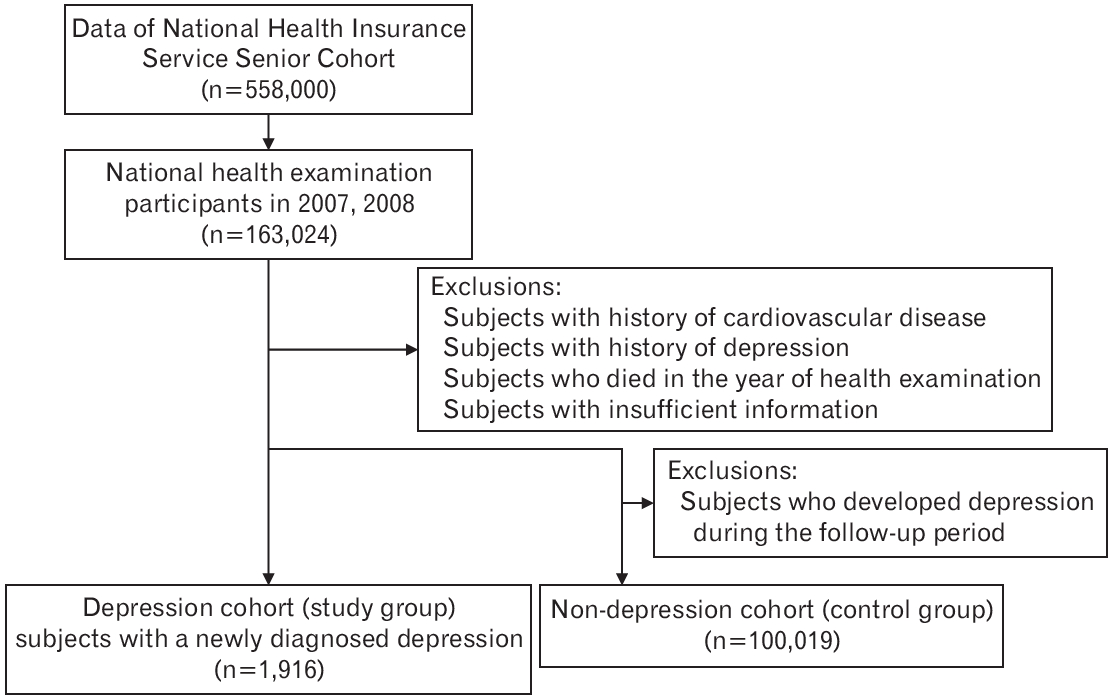
We selected 163,024 subjects from the Senior Cohort, aged 65 years or older, who participated in the national health examination program in 2007 and 2008. Among them, we excluded participants with a previous history of cardiovascular disease and depression, participants who died in 2007 or 2008, and participants with insufficient information. Further, we selected participants who were diagnosed with depression, defined using the International Classification of Diseases, 10th revision (ICD-10) codes F32 (major depressive disorder, single episode), F33 (major depressive disorder, recurrent), in the year 2007 or 2008, resulting in a total of 1,916 participants (depression group). Additionally, we excluded subjects who developed depression during the follow-up period. The remaining 100,019 participants constituted our control group (Figure 1).
2. Variables
1) Socio-demographic factors and covariates
Personal data, medical claims data, and national health examination data were collected using the NHIS database. Personal data included age, sex, household income, and mortality data. Medical claims data included diagnosis of each participant using the ICD-10, Clinical Modification (ICD-10-CM) codes. Health examination data included height, weight, smoking status, alcohol intake, and physical activity.
Age was categorized into five groups, namely 65 to 69 years, 70 to 74 years, 75 to 79 years, 80 to 84 years, and 85 years or older. Body mass index (BMI) was categorized into three groups based on the international WHO obesity classification [14], with a BMI <25.0 kg/m2 denoted as normal, a BMI between 25.0–30.0 kg/m2 as overweight, and a BMI ≥30.0 kg/m2 as obese. Alcohol consumption was categorized into three groups: less than 1 time per week, one to 4 times per week, and 5 times or more per week. Smoking status was categorized into three groups: never smoked, past smoker, and current smoker. Physical activity was categorized into three groups: no exercise, exercise 1 to 6 times per week, and exercise every day. Household income level was categorized, using NHIS health data, into three groups: household income >50%, household income ≤50%, and Medicaid as lowest income group. Comorbid hypertension, diabetes mellitus, and dyslipidemia were identified using the ICD-10-CM codes from the medical claims data. Hypertension was defined using the ICD-10-CM code I10-15, diabetes mellitus using the ICD-10-CM code E10-14, and dyslipidemia using the ICD-10-CM code E78. All of the variables above were tested and adjusted in the analyses.
2) Study endpoints
The primary endpoint was development of ischemic heart disease or cerebrovascular disease. Ischemic heart disease was defined as acute myocardial infarction, angina pectoris, or chronic ischemic heart disease using the ICD-10-CM codes I20–25. Cerebrovascular disease was defined as transient ischemic attack or stroke using the ICD-10-CM codes I60–64, I69, and G45.
For participants who had been diagnosed multiple times, only the first diagnosis was counted. The follow-up period was defined as the time interval between either January 1, 2008 or January 1, 2009 and the initial date of diagnosis of ischemic heart disease or cerebrovascular disease, death of any cause, or December 31, 2012 or December 31, 2013, whichever came first.
3. Statistical Analysis
All statistical analyses were performed using SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA), and the statistical significance level was set at P<0.05. Baseline characteristics were compared using chi-square test and t-test. Hazard ratios (HRs) and associated 95% confidence intervals (CIs) were estimated using Cox proportional hazards models. Multivariable Cox models were used to control the known cardiovascular risk factors such as hypertension, diabetes mellitus, dyslipidemia, sociodemographic factors, including age, sex, household income, and lifestyle factors, including smoking status, alcohol consumption, and physical activity.
4. Ethical Approval
The Hallym University Dongtan Sacred Heart Hospital approved (2018-06-011) the use of these data.
RESULTS
1. Baseline Characteristics of Subjects
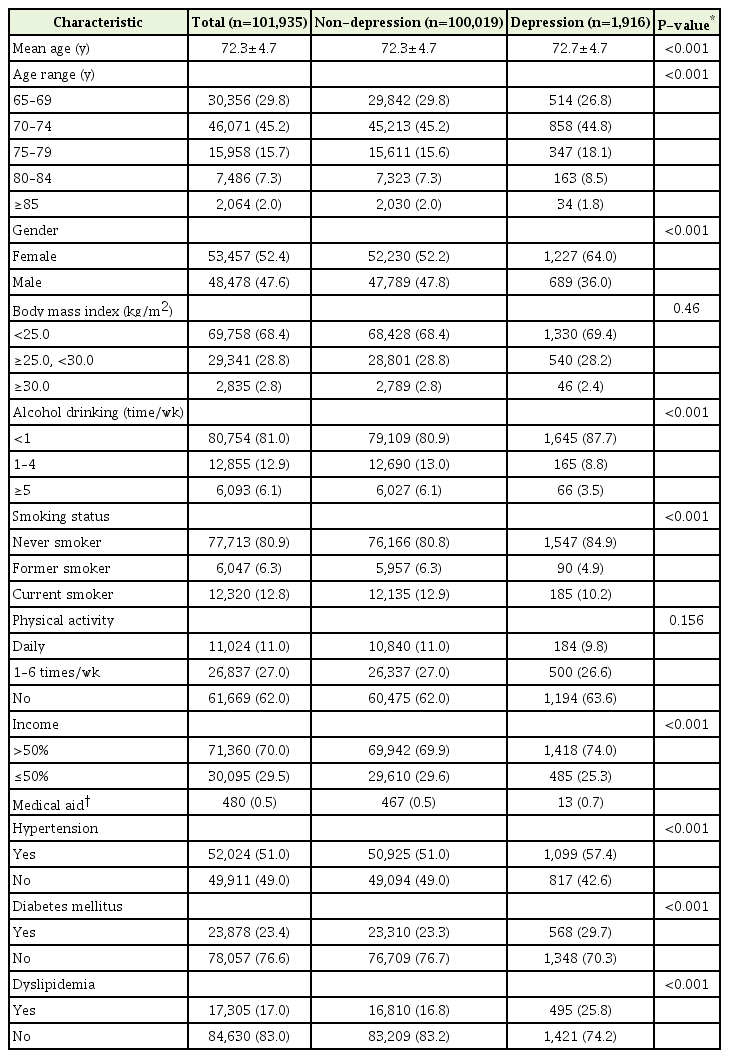
The sample constituted 101,935 participants in total, with 1,916 individuals in the depression group and 100,019 individuals in the non-depression group. The average age of the participants of the depression group was 72.7±4.7 years and the non-depression group was 72.3±4.7 years. The depression group reported a significantly higher proportion of female, high income, less frequent drinker, and never smoker as compared the non depression group, with proportion of 64.0%, 74.0%, 87.7%, and 84.9% in the depression group, and 52.2%, 69.9%, 80.9%, and 80.8% in the non-depression group, respectively (P<0.001, chi-square test). The depression group reported a significantly higher proportion of hypertension, diabetes mellitus, and dyslipidemia as compared to the non-depression group, with proportion of 57.4%, 29.7%, and 25.8% in the depression group, and 51.0%, 23.3%, and 16.8% in the non-depression group, respectively (P<0.001, chi-square test) (Table 1).
2. Impact of Depression on Ischemic Heart Disease
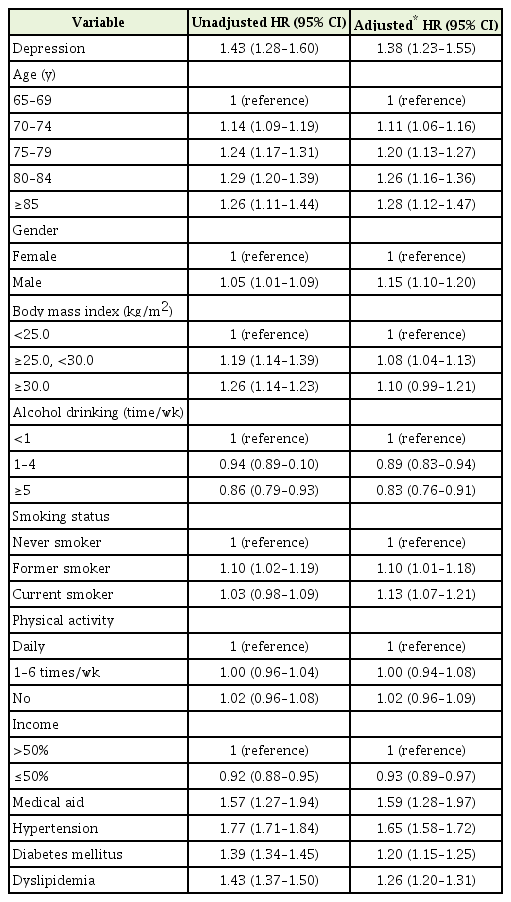
During the average follow-up period of 1,606 days, 16.1% (308/1,916) participants of the depression group developed ischemic heart disease, which was significantly higher than 11.7% (11,688/100,019) participants of the control group (P<0.05, chi-square test) (Table 2). The multivariate Cox regression analysis included depression, age, gender, BMI, alcohol consumption, smoking status, physical activity, income, hypertension, diabetes mellitus, and dyslipidemia. The HR between depression and ischemic heart disease was 1.38 (95% CI, 1.23 to 1.55) after adjusting all confounding variables. Factors such as old age, male gender, obesity, and smoking increased the risk of ischemic heart disease. Physical activity did not seem to have an effect on ischemic heart disease in this study. Hypertension, diabetes mellitus, and dyslipidemia also increased the risk of ischemic heart disease by 65%, 20%, and 26%, respectively, after adjustment (Table 3).
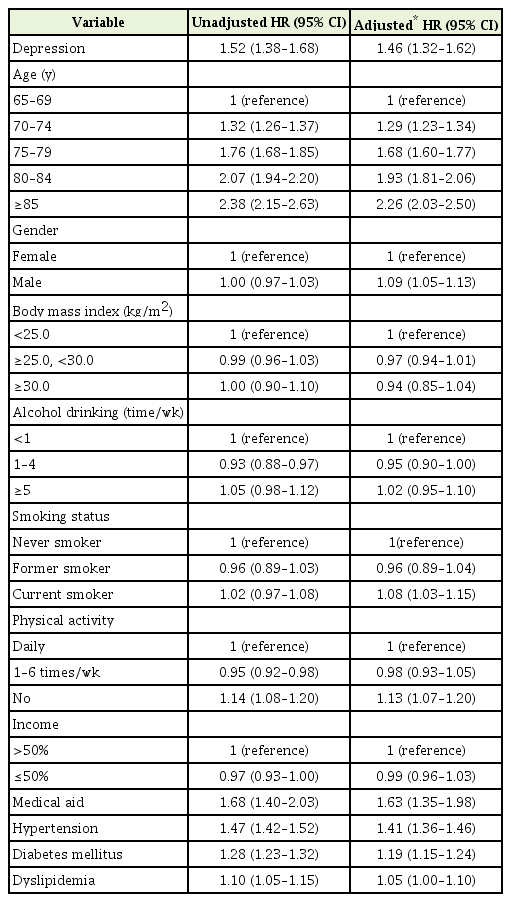
3. Impact of Depression on Cerebrovascular Disease
During the average follow-up period of 1,586 days, 20.6% (395/1,916) participants of the depression group developed cerebrovascular disease, which was significantly higher than 14.4% (14,373/100,019) participants of the control group (Table 2). The multivariate Cox regression analysis revealed that depression also significantly increased the HR for cerebrovascular disease, with a HR of 1.46 (95% CI, 1.32 to 1.62) for cerebrovascular disease after adjusting all confounding variables. Characteristics such old age, male gender, and smoking increased the risk of cerebrovascular disease. Hypertension, diabetes mellitus, and dyslipidemia also increased the risk of ischemic heart disease by 41%, 19%, and 5% respectively, after adjustment (Table 4).
DISCUSSION
The results revealed that depression increased the risk of both ischemic heart disease and cerebrovascular disease. A systematic review of depression as a risk factor for coronary heart disease, reviewing 30 cohort studies, reported a pooled relative risk of 1.30 (95% CI, 1.22 to 1.40) [15], which is consisted with our results that reported an adjusted HR of 1.38 (95% CI, 1.22 to 1.40) for ischemic heart disease. Another systematic review of depression as a risk factor for stroke, reviewing 28 cohort studies, reported a pooled adjusted HR of 1.45 (95% CI, 1.29 to 1.63) [5], which is also consisted with our results that reported an adjusted HR of 1.46 (95% CI, 1.32 to 1.62).
The proposed potential mechanisms that influence the impact of depression on cardiovascular disease include pathophysiological changes and behavioral, lifestyle factors, and it is likely to be multifactorial. Depression is involved in the stress-induced activation of the HPA axis [7]. Elevated levels of cortisols have been repeatedly found in patients with depression, thereby increasing visceral fat mass, hyperlipidemia, and glucose intolerance [16,17], which increases the risk of cardiovascular disease, and diabetes, and also drives sympathetic activation [18]. Moreover, depression may lead to autonomic nervous system disorders such as decreased heart rate variability, increased heart rate, excessive heart rate response to physical stress, and increased ventricular depolarization variability, thereby increasing the risk of cardiovascular disease [8]. Depression is also associated with increased platelet activation and endothelial dysfunction [10]. Increased platelet activity increases the risk of thrombus formation and arterial occlusion [19]. Prolonged mental stress, which is common in depression has been shown to induce endothelial dysfunction, and is associated with many cardiovascular risk factors [20]. Further, patients with depression reported elevated levels of inflammatory markers, such as C-reactive protein and proinflammatory markers, such as interleukin 1, 2, 6, and tumor necrosis factor [11]. Inflammatory pathways play a major role in the development of atherosclerosis, leading to higher risk of cardiovascular disease [11]. Patients with depression tend to engage in unhealthy behaviors such as smoking, alcohol use, unhealthy diet, poorer medical adherence, and physical inactivity leading to obesity [12]. Patients with depression are also less motivated to engage in lifestyle modification.
Consistent with our results, past findings confirmed that factors such as old age, male gender, hypertension, diabetes mellitus, dyslipidemia, obesity, smoking, and lack of physical activity are well-known risk factors for cardiovascular disease [21-24]. However, obesity reported no significant effect on cerebrovascular disease. This finding may be explained by the concept of obesity paradox in older adults [25]. Lack of physical activity is a well-known risk factor [26], but our results reported no significant relationship between lack of physical activity and cardiovascular disease. Light to moderate alcohol consumption is suggested to decrease the risk of ischemic heart disease [27], which is also consistent with our results.
This study has several limitations. First, the definition of depression was based only on ICD-10 codes, without any screening tools or prescription information. Depression is underestimated especially in the elderly population because they often encounter somatic complaints instead of depressive moods and are reluctant to receive psychiatric care. Therefore, the number of participants with depression may have been underestimated. Second, the severity of depression was not determined. Third, the effects of antidepressants on cardiovascular disease were also not considered in this study.
Despite its limitations, this study has several strengths. First, to the best of our knowledge, this study was the first cohort study in Korea to investigate the impact of depression on cardiovascular disease. There was an observational study based on Korean adults who visited a university hospital for health examination that reported depression was significantly related with hypertension and dyslipidemia [28], while another study based on Korean adults, using Korea National Health and Nutrition Examination Survey, reported that depression was only associated with dyslipidemia in males [29]. Second, we included data regarding behavioral risk factors including smoking status, alcohol consumption, and physical activity, obtained through the health examination data in the form of self-report questionnaires. Major risk factors for cardiovascular disease were included and adjusted using Cox proportional hazard model. Third, since the sample size of this study is large, and based on the Senior Cohort database of NHIS, the sample may represent the general elderly population in Korea.
In conclusion, we found that, independent of other cardiovascular risk factors, a confirmed diagnosis of depression increases the risk of ischemic heart disease and cerebrovascular disease by 38% and 46% among older adults in Korea, respectively. Since depression may be a high-risk factor for cardiovascular disease, future research should focus on the diagnosis and prevention of cardiovascular disease in people with depression.
Notes
No potential conflict of interest relevant to this article was reported.