Effect of Patient Empowerment Model on Smoking Cessation: Randomized Controlled Trial
Article information
Abstract
Background
Smoking is a preventable cause of chronic morbidity. Patient empowerment is a process through which people establish greater control over their health-related decisions and actions. To assess the effect of patient empowerment versus health education on the nicotine dependence score and progress of patients under different stages of smoking cessation.
Methods
This was a single-blinded randomized controlled clinical trial that included 76 smokers attending family medicine clinics. Participants were divided into two groups: empowerment and health education groups. Their nicotine-dependence score and smoking cessation stage were identified. All study participants were subjected to five health education sessions with a 3-month follow-up period.
Results
The mean nicotine-dependence score decreased significantly in both groups after the intervention. This decrease was slightly higher in the empowerment group; however, the difference was not statistically significant. After the intervention, 16.7% of the health education and 30.0% of the empowerment group transitioned from stage 1 to stages 2–4 of smoking cessation, with the change being statistically significant only in the empowerment group. There was no statistically significant difference in the number of study participants who stopped smoking between the health education and empowerment groups.
Conclusion
Both the empowerment model and traditional health education have similar positive effects on decreasing the nicotine-dependence level. There was a significant improvement in the stage of change for patients under the empowerment model, although there was no statistically significant difference between the groups regarding the number of participants who stopped smoking.
INTRODUCTION
Smoking is the most important cause of preventable morbidity and mortality in developed countries [1]. It causes a wide range of diseases, including chronic obstructive pulmonary disease (COPD), coronary heart disease, stroke, and many types of cancer [2].
Factors that cause failure to stop smoking include high dependence on nicotine and the lack of will and confidence [3]. Therefore, smoking cessation programs should include behavioral counseling to enhance motivation and support for attempts to quit along with pharmacological interventions to reduce nicotine dependence and withdrawal symptoms [4].
Despite the development of a wide and broad range of smoking cessation interventions which were considerably effective [5], behavioral interventions reach less than 5% of smokers who try to quit [6].
Anti-smoking counseling interventions may be simple and brief without a motivational aspect, which is usually how it is conducted in traditional care, or part of more intensive motivational interventions [7].
Empowerment is considered an effective approach to a variety of chronic diseases. In the sphere of health, the expression has been adopted primarily as guidance for health promotion approaches and, in recent years, as a strategy for the management of chronic conditions [8].
Empowerment means that the patient is at the center of the team, has support from their family, and is responsible for the day-to-day implementation of the treatment plan. Therapy will be most effective if the patient understands the regimen, recognizes its value, and has mastered the skills to perform the required tasks correctly [9]. The World Health Organization (WHO) has described patient empowerment as a “prerequisite for health”, encouraging patients to be proactive and adopting patient self-care strategies to improve health outcomes and quality of life [10].
Although earlier studies have assessed the effect of different modalities on smoking cessation, to the best of our knowledge, no studies have assessed the effect of the empowerment model on smoking cessation.
This research hypothesizes that the empowerment model is more effective on smoking cessation than the traditional health education model. Thus, we aimed to study the effect of empowerment on the progress of patients in terms of their stage of smoking cessation and their nicotine dependence score.
METHODS
1. Setting
This was a single-blinded randomized controlled clinical trial that was conducted on 78 current smokers visiting family medicine outpatient clinics at Cairo University Hospitals in Egypt. The study was conducted from January 2018 to May 2018.
2. Participants
The sample size was calculated using the Epi 6 program set (Centers for Disease Control and Prevention, Atlanta, GA, USA) to achieve 100% power and to detect a difference of 13.0 (5% reduction of nicotine dependence scale) between the null hypothesis (wherein both groups means are 259.0) and the alternative hypothesis (wherein the mean of group 2 is 246.0), with estimated group standard deviations of 1.0, and with a significance level (α) of 0.05000 using a two-sided two-sample t-test [11]. The suggested sample size was estimated to be 30 participants for each group; however, after anticipating a 25% dropout rate, the study was conducted on 78 participants.
Current (smoking almost every day in the past 3 months) smokers of both sexes aged between and 18–64 years who are visiting the family medicine clinic at Cairo University Hospitals for a variety of medical conditions (e.g., diabetes mellitus and hypertension) were invited to participate in the study. Subjects who agreed to participate and fulfilled the inclusion criteria were recruited. Patients who were known to have a terminal or severe illness or mental impairment were excluded.
3. Randomization
We had a sample frame consisting of a list of all clinic attendants who fulfilled the inclusion criteria. The target populations were chosen randomly, and the patients who agreed to participate in our study were randomly allocated into one of two groups (intervention or control) by picking a sealed opaque envelope containing a number. Those who drew odd numbers were allocated to the health education group, and those who drew even numbers were allocated to the empowerment group.
4. Intervention
In the first visit, all patients were subjected to history taking, which included sociodemographic data and medical history. Questionnaires on the stage of change assessment and a nicotine dependence level assessment using the Brief Wisconsin Inventory of Smoking Dependence Motives (WISDM) scoring system were completed by the patient. After that, both groups were subjected to five educational sessions in the form of group discussions.
Both groups were subjected to sessions which had the same content and theme, duration, interval between the sessions, and educational materials. The sessions were conducted by the same researcher in both groups. Each session lasted 45 minutes, with a 1-month interval between sessions. Each group comprised 10–15 members. Attendance of a relative was required for participants in both groups. Finally, reassessments of both groups were completed using the stage of change questionnaire and nicotine dependence level questionnaire.
The contents of the five educational sessions were as follows: the first session included an introduction of the study and its objectives, obtaining patient consent, and filling the questionnaires. The second session was conducted 1 week after the first session and discussed the following items: hazards of smoking, causes of smoking cessation, and short-term and long-term benefits of smoking cessation. The third session was conducted 3 weeks after the second session, and the following items were discussed: decision on smoking cessation and how to deal with special fears about smoking cessation. The fourth session was conducted 1 month after the third session and discussed the following items: nicotine withdrawal symptoms and how to avoid this, possible causes of relapse, and how patients can prevent relapsing. The fifth session was conducted 1 month after the fourth session and aimed to reassess the patients using the stage of change questionnaire and determining their nicotine dependence score.
Group A sessions (health education model) were conducted as didactic one-way health education sessions. Participants received information on the theme of the session. Afterwards, the instructor answered the concerns raised by the patients, and the patients were invited and encouraged to follow the cessation plan suggested by the instructor.
Group B sessions (empowerment model) were conducted as two-way health education sessions. The instructor provides knowledge derived from the patients themselves, as they are considered in the empowerment model as valuable sources of experiential knowledge. The instructor first raised several questions and encouraged the patient to answer and share their knowledge. Afterwards, he responded to the concerns raised by the patients either by asking other participants about their experiences or answering questions directly. After that, he ensured that patients had sufficient knowledge and resources to overcome the expected barriers and difficulties and to make thoughtful decisions. He discussed with the patients how to make their knowledge functional and how to apply this information to their circumstances. By this stage, the patients were expected to have developed confidence, self-efficacy, and the skills to take control of their daily life, and to have taken charge of self-management. Finally, when the patients felt that they were more informed and clarified what matters most to them, they were able to establish more realistic expectations regarding the pros and cons of cessation, and they were invited to participate more in their health decision-making, planning, and implementation.
5. Tools of the Study
Our primary goals were to identify the effect of the empowerment technique on the nicotine-dependence score and on the progress of patients in stages of smoking cessation. The secondary goal was to assess the effect of empowerment versus traditional health education on the smoking cessation rate.
The questionnaires that we used in this study included a questionnaire on the stage of change assessment [12] and a questionnaire on nicotine dependence level assessment which used the Brief WISDM scoring system [13]. These were translated and back-translated. An expert translated the original questionnaire from English into Arabic. The Arabic versions were translated back into English by a bilingual individual. The translated and original versions of the questionnaire were compared. We conducted a pilot study on five cases to adjust the questions and determine the time needed to complete the questionnaires. The questionnaires were also revised by three family doctors and two nurses in family medicine. The results of the pilot study were not included in the results of this study.
The questionnaire regarding the stage of change assessment consists of 30 questions: eight questions to diagnose the pre-contemplation stage, six questions to diagnose the contemplation stage, six questions to diagnose the preparation stage, and 10 questions to diagnose the action stage. This questionnaire hinges on the trans-theoretical model, which suggests that behavioral change occurs in five consecutive stages: pre-contemplation (not planning to change within the next 6 months), contemplation (thinking about change), preparation (taking steps towards changing), action (attempting the change), and maintenance (able to sustain the change for more than 6 months and trying to avoid relapse).
The nicotine dependence level assessment using the brief WISDM assesses a wide variety of motives that might drive tobacco use in smokers. It includes 11 subscales with 37 questions. The 11 subscales include: affiliative attachment, automaticity, loss of control, cognitive enhancement, craving, cue exposure, social/environmental goads, and taste. Patients responded to each question on a Likert scale with 7 points, with answers ranging from 1 or “strongly disagree” to 7 or “strongly agree”. The total score ranged from 37 to 259, with higher scores indicating greater levels of nicotine dependence.
6. Statistical Analysis of Data
Data analysis was performed using the IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA). Qualitative data was described using frequencies and percentages, while quantitative data was presented using means, standard deviations, and interquartile ranges. A chi-square test was used to compare categorical data across groups and in repeated measures, while Fisher’s exact test was used to compare qualitative variables between groups when one expected cell or more had a value less than five. Pairwise testing was performed using paired and independent t-tests with Bonferroni adjustment for the number of comparisons. The mean difference described the changes undergone by each group with a 95% confidence interval. Mann-Whitney and Wilcoxon tests were used instead of unpaired t-test and paired t-test, respectively, to analyze non-parametric data if the standard deviation was more than 30% of the mean. Statistical significance was set at P<0.05.
7. Ethical Considerations
Ethical approval was obtained from the research committee of the Faculty of Medicine, Cairo University. Informed written consent was obtained from all patients after a full explanation of the nature of the study, benefits, and possible harms of the study.
RESULTS
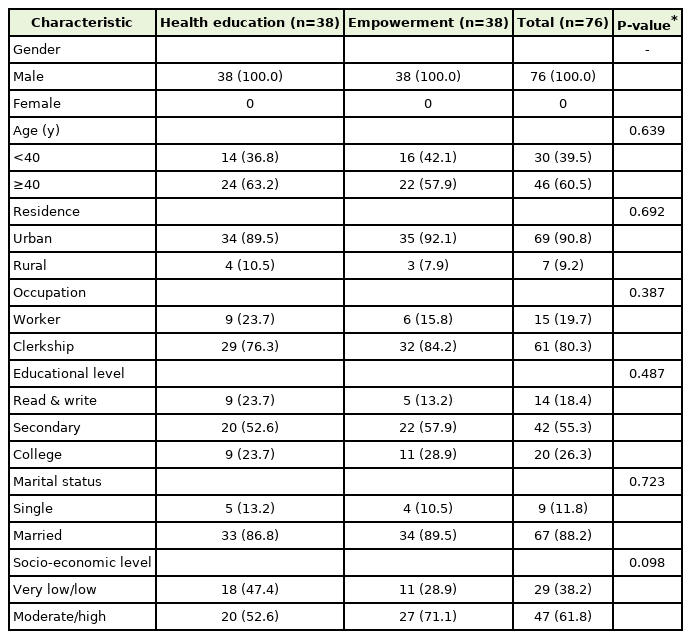
As shown in Table 1, all study participants were men. There were no statistically significant differences between the health education and empowerment groups in terms of residence, occupation, education, and socioeconomic level.
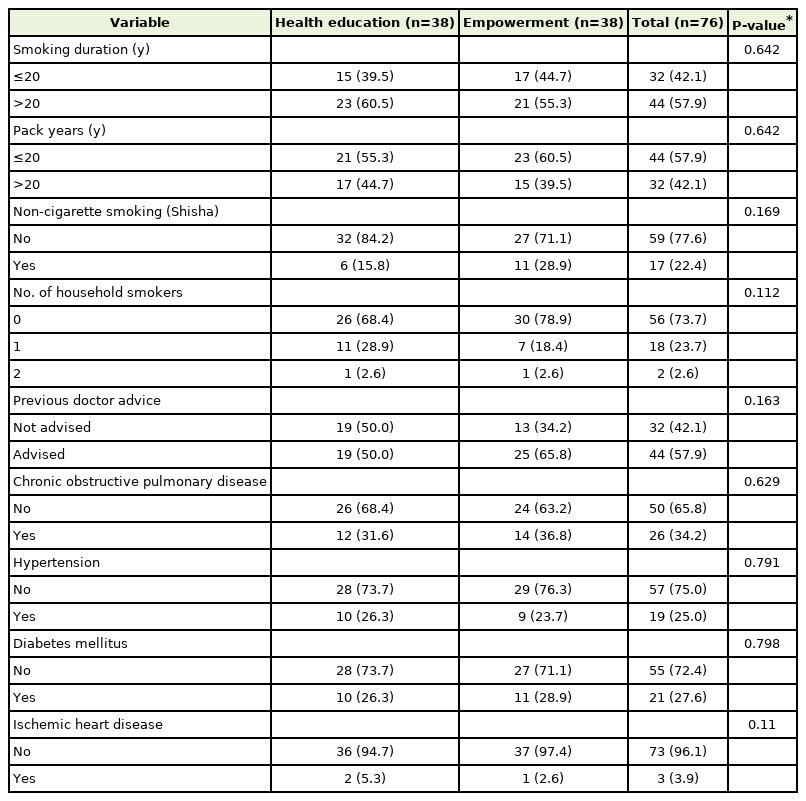
COPD was the most common chronic disease among our participants. There were no statistically significant differences in terms of previous doctor advice and chronic medical diseases between the health education and empowerment groups (Table 2).
Table 3 shows that there was no statistically significant difference in the number of smoked packs per year between the health education and empowerment groups. The mean number in the health education group was (26.58±21.35) and in the empowerment group, it was (26.61±23.52).
Before the intervention, there was no statistically significant difference in the nicotine dependence score between the health education and empowerment groups, as shown in Table 4. The mean nicotinedependence score decreased significantly in both groups after the intervention.
Before the intervention, there was no significant difference in the distribution of subjects in either group among the stages of change. After the intervention, there was still no significant difference in the distribution of subjects in either group among the stages of change. The number of participants from the empowerment group who progressed from pre-intervention to post-intervention was significantly higher than that in the health education group (P=0.04) (Table 5). In terms of smoking cessation, 2.6% and 5.3% of study participants stopped smoking in the health education and empowerment groups, respectively, with no statistically significant difference between the groups.
DISCUSSION
Although giving simple advice will positively affect smoking cessation, the actual behavioral modification requires the patients to take initiative and recognize that they are the center of their health decision, which can be achieved through the empowerment technique. This explains why in the empowerment group, the number of participants who progressed from pre-intervention to post-intervention was significantly higher than that in the health education group (P=0.04). In this study, after the intervention, about 16.7% of the health education group and 30.0% of the empowerment group moved from the precontemplation stage to more advanced stages of change. By the end of the study, the rates of smoking cessation were 2.6% and 5.2% in the health education and empowerment groups, respectively.
These findings can be attributed to the fact that progression through stages of change does not merely necessitate changes in knowledge but also requires changes in attitudes and beliefs. For example, an individual must be persuaded and recognize that their behavior is detrimental to their health in order to move from the pre-contemplation stage to the contemplation stage.
The current study found that the mean nicotine dependence score (WISDM) decreased significantly in both groups after the intervention (P=0.000). The decrease in nicotine dependence was slightly higher in the empowerment group (5.2%) than in the health education group (2.4%), but the difference was not statistically significant. This rate may have increased if the follow-up period were longer.
The positive findings that we found in both groups can be explained by conducting these sessions as group discussions and asking participants to bring a relative to these sessions. We asked all the participants in both groups to bring one of their relatives who they were living with and found that the presence of relatives augmented and extended the effect of sessions.
We conducted group discussions in the two groups and noticed that it was an effective method for achieving behavioral change; it is also considered more cost-effective than individualized interventions for every smoker and makes better use of the trainers’ time. Furthermore, it promotes social learning where there is a chance to share experiences, encourage, and support each other while potentially establishing supportive social networks among the members, which may contribute to higher cessation rates.
Our findings regarding the empowerment model agreed with those of Ghasemi et al. [14] in 2018, who studied the effect of the family-centered empowerment model on methamphetamine users. The results showed that after partaking in empowerment sessions for 3 months, there was a significant improvement in the severity of damage caused by drug abuse [14].
In addition, the findings of the current study were consistent with the study of Ebrahimi et al. [15] in 2016, in which they studied the effect of the empowerment model versus routine education on metabolic controls of 103 type 2 diabetic patients. After an 8-week follow-up period, the results showed that applying the empowerment model had positive effects on the metabolic control indicators of their participants [15].
The WISDM provides information on different motives that might drive tobacco use in smokers; it reflects the function of dependence and tolerance processes. Although nicotine dependence has been recognized as an important factor in predicting smoking behaviors in adults, behavioral changes occur very gradually. During the early stages, people are usually reluctant or resistant to change. Even when they adopt a proactive and committed approach to change a certain behavior, conflicts may make them struggle and they become uncertain about their ability to overcome these motives. This stage may last for an extended period.
Thus, we considered that when the stage of change progresses, nicotine- dependent motives diminish more after a while. This resembles a small step toward the goal of smoking cessation. This point may explain why there was a significant improvement in the progression of the stage of change for participants under the empowerment group, while there was no significant difference between the groups in terms of their WISDM score following intervention.
1. Limitation and Strength
All study participants were men. Smoking among females is uncommon in our culture, with a much lower prevalence compared to males. In addition, the duration of patient follow-up was 3 months, which may not have been long enough to change health behavior significantly. This study was single-blinded; however, the questionnaires were completed by the patients. The sessions were held by the same instructor, which may have affected the results because of the researcher’s interest, although the researchers established a protocol for the instructors to follow during the session. Although we assessed smoking index before the study, unfortunately, we did not assess the smoking index after the intervention.
To our knowledge, this study is the first to examine the effect of the empowerment model versus the traditional health education model in smoking cessation. The participants in both groups were well matched. Both groups underwent sessions that had the same instructor, content, duration, and educational materials.
2. Implications for Practice and/or Research
More studies are necessary to evaluate the cost-effectiveness of the application of this model on one-to-one education in everyday practice.
3. Conclusion
In the context of group-based education for smoking cessation, traditional health advice and empowerment have similar positive effects on decreasing the nicotine dependence level. The empowerment group showed significant improvement and progression in terms of the stage of smoking cessation. However, there was no significant difference between the groups regarding the distribution of patients across the stages of change after intervention.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
We would like to express our appreciation to the participants who helped us conduct our study.