Preventive Measures against the Development of Dementia in Old Age
Article information
Abstract
Dementia is a neurological condition characterized by numerous types of central nervous system diseases, which gradually deteriorates an individual’s reasoning, rational thinking, and judgment abilities. As a serious public health concern that currently affects more than 50 million older adults, dementia is one of the most significant causes of incapacity, disability, and dependency among older adults. As new cases are expected to increase exponentially in the next three decades, dementia, which is not a normal feature of healthy aging despite the fact that it generally affects older adults disproportionately, requires enormous management and care efforts due to its associated socioeconomic, psychological, and physical burdens that involve the patient, their caregivers, guardians, family members, and society at large. Presently, there is no cure for dementia; however, this condition could be prevented. This narrative review aimed to provide a broad overview of studies detailing the alternative lifestyle modification-centered preventive measures against dementia. A comprehensive search of key databases to find articles related to this topic revealed that participating in regular physical activities, healthy eating and dieting, avoiding all forms of smoking, avoiding air pollutants, halting or reducing alcohol consumption, exercising the mind and being socially dynamic, getting enough rest and establishing good sleeping habits, infection prevention, stress prevention, avoidance of injuries, preventing the effects of social isolation and lockdowns, continuing education, and depression prevention are protective measures against the development of dementia.
INTRODUCTION
Dementia is a progressive neurological condition characterized by numerous types of central nervous system diseases that tends to worsen over time; it usually deteriorates an individual’s sound reasoning, rational thinking, and judgment abilities, thereby affecting the performance of normal day-to-day functioning and activities [1]. In some cases of dementia, an individual’s motivation, emotional control, and social conduct are affected, but consciousness and alertness in individuals are not usually hampered [2-4].
As a serious public health concern, dementia is one of the major causes of incapacity, disability, morbidity, and dependency among older adults [1,2]. Statistically, over 10 million patients are newly diagnosed with dementia every year, and a total of 50 million people worldwide are affected with this condition [2].
Furthermore, the World Health Organization (WHO) projected an exponential increase of 82 million cases of dementia in the next 10 years and 152 million by the year 2050 worldwide; this considerable upsurge in estimation is inferable to the increasing numbers of people with dementia living in underdeveloped and developing regions and countries around the world [2]. To this end, with the hope of abating the number of future cases of dementia, this review aimed to provide an overview of dementia, with a primary emphasis on scientifically proven lifestyle modification-centered preventive measures.
SOURCES OF INFORMATION AND METHODOLOGY
This narrative review aimed to provide information on dementia and to determine the appropriate measures that can prevent or reduce the severity of this condition based on the current literature. The literature search commenced between March 2020 and February 2021, and only significant studies published within the last 10 years were screened based on the topic of discourse from Medline (PubMed), Google Scholar, and specific global organizations, associations, and national health organization information archives, such as the WHO, National Institute on Aging, Alzheimer Disease International, and Alzheimer’s Research United Kingdom.
The search terms used were “dementia,” “prevalence of dementia,” and “prevention of dementia.” Furthermore, each of the returned results from the automated searches on the “prevention of dementia” was additionally searched to obtain a variety of cogent literature that extensively discussed this subheading. As this was a narrative research, all types of studies were eligible for inclusion in this review, including clinical trials, meta-analyses, randomized controlled trials, systematic and viable review documents, and website data.
After gathering all the searched results, thousands of articles were obtained; however, after reviewing the available data, the most significant works published on the aforementioned themes were downloaded, carefully reviewed, summarized, and reported in a narrative way taking into account the various issues involved. After careful screening of the abstracts of each article for content and face validity and in line with the set objectives of this study, 90 articles from Medline (PubMed), five articles from Google Scholar, seven articles from website data, and one book article, with a total of 103 articles, were included in this review.
PREVALENCE OF DEMENTIA
More than 9.9 million patients worldwide are diagnosed with dementia annually, and at least one new case is reported every 3.2 seconds [2]. Furthermore, 50 million individuals are living with dementia, with the vast majority or 60% living in underdeveloped and developing regions of the world, and the number of cases is expected to triple in the next three decades [2,5,6]. Current data show that dementia usually manifests in adults 60 years and older, with an average confirmed dementia cases of 5%–8% at a given point in time [2]. The exponential increase and increase in the number of forecasted dementia cases worldwide are attributed to the consistent increase in the number of individuals living with dementia in underdeveloped and developing regions and countries [2,6]. With 14.9 million confirmed cases, the Asian continent is the region with the vast majority of individuals living with dementia, followed by Western Europe (7.5 million) and North America (4.8 million); however, these figures are projected to dramatically increase in the coming years [5,6].
According to income status estimates, the number of adults living with dementia in low-income countries will increase by 264% [6]. It will increase by 227% in upper-middle-income countries, 223% in lower-middle-income countries, and 116% in higher-income countries in the next 30 years [6]. However, the burden of dementia is incalculable because it not only affects those with the condition alone, but also their caregivers, families, health care organizations, and the general public as a whole [2].
In addition to the significant burden imposed by dementia, the 9th most common burdensome condition affecting individuals >60 years of age, this condition is more common in women >65 years of age than in men [7]. In terms of economic estimates, US $818 billion were spent on the treatment and management of dementia in 2015 alone, accounting for 1.1% of the world’s gross domestic product [5]. Additionally, over US $1 trillion was expected to be spent on the treatment, care, and management of people living with dementia by the year 2020 [5]. In this regard, the yearly global expenditures and expenses associated with the treatment, care, and management of dementia cases surpass the market value of some major international organizations such as Apple and Google [5].
These general findings clearly pinpoint the severity and seriousness of dementia and its immense negative impact on the general health system and financial status of underdeveloped and developing countries, as well as developed countries across the globe.
EVIDENCE BASED PROGRAM REVIEW FOR PREVENTING DEMENTIA
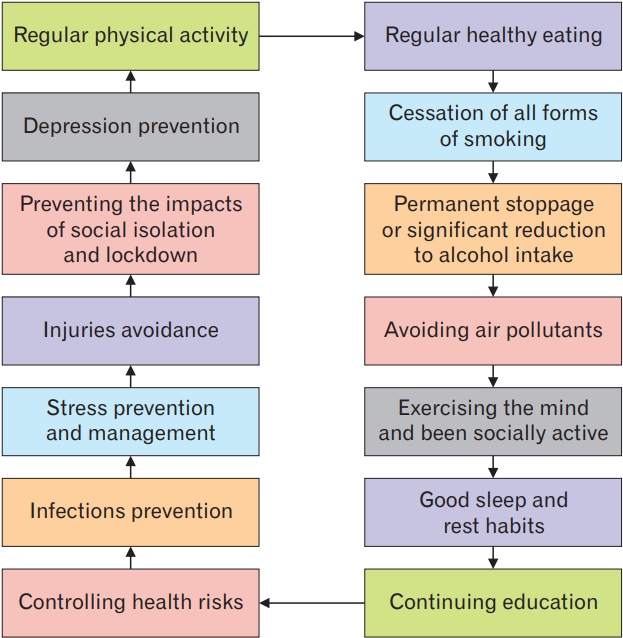
Despite the fact that advanced age is the biggest risk factor for dementia, this condition is not part of the normal aging process. Presently, there is no known cure for dementia, but research evidence firmly shows some preventive measures that could help reduce the risk of having the disease [2,4]. Thus, the following, backed by scientific studies, are discussed extensively as probable public-centered proactive measures against the development of dementia and other forms of dementia (Figure 1).
ENGAGING IN REGULAR PHYSICAL ACTIVITY
Exercise has emerged as a key intervention for positively influencing comprehension and cognition as well as reducing the risk of age-related cognitive decline and dementia [8]. In addition,, performing regular physical exercise strengthens antioxidative capacity, reduces oxidative stress, and exerts anti-inflammatory effects, which further improve the endothelial function and can increase brain capillarization [9]. In addition, physical activity can counteract dyslipidemia and decrease the ceramide levels, while also improving the amyloid-β (Aβ) clearance by upregulating the Aβ transporters and increasing the basal testosterone levels [9].
Significantly, a minimum of 150 minutes of temperate aerobic physical activity every week in combination with additional resistance training is imperative to keep the brain healthy in individuals with subjective cognitive decline and mild cognitive impairment [10]. Likewise, a concentrated exercise program (specifically a 4-week program), regardless of whether this is a strength or aerobic training program, offers substantial advantages to older patients with dementia, and the serum brain-derived neurotrophic factor will be additionally enhanced by performing aerobic training [11]. Furthermore, a combination of aerobic and strength training activities is more effective than aerobic activity alone in slowing the cognitive and motor decline in adults with dementia [12,13]. Specifically, physical activity improves cognition and comprehension, particularly executive functioning and memory, and independent functioning in patients with dementia [13,14].
Findings from a large and long-term randomized controlled trial study on the effects of multidomain interventions such as diet, exercise, cognitive training, and vascular risk monitoring on the cognitive decline in high-risk older people revealed that the simultaneous performance of physical activity, nutritional counseling, vascular risk monitoring and management, and cognitive training and social activity could improve or maintain cognitive function regardless of the individuals’ characteristics [15-17]. Importantly, findings from a large study on the effect of a 2-year physical activity intervention compared with health education on cognitive outcomes in sedentary older adults revealed that a 24-month minimal intensity physical activity program did not improve the cognitive or composite measures of the participants, compared with a health education program [18]; however, these findings should not disregard the overall beneficial effects of physical activities on well-being and cognitive function.
CONSUMING A REGULAR HEALTHY DIET
In the prevention and treatment of mental disorders, the role of an appropriately adjusted eating regimen such as the consumption of fresh fruits, can significantly prevent depressive disorders as they contain high amounts of nutrients that the body needs [19,20]. For instance, increased consumption of natural fruits and vegetables, specifically berries, citrus, and green leafy vegetables, may promote higher levels of optimism and self-efficacy; reduce the level of psychological distress, ambiguity, and malignancy fatalism; and protect against depressive symptoms [20]. Moreover, the consumption of high-quality food was associated with a decreased risk of experiencing a global cognitive decline compared with consumption of low-quality food [21]. In addition, the consumption of long-term dewaxed brown rice reduces and prevents cognitive deterioration, particularly in older individuals with decreased cognitive capabilities [22].
Importantly, there is a beneficial relationship between the Mediterranean-DASH (Dietary Approaches to Stop Hypertension) Intervention for neurodegenerative delay diet and cognitive functioning, while increased consumption of saturated fatty acids could have negative impacts on age-related cognitive decline and are thus not recommended [23-25]. Furthermore, consumption of monounsaturated fatty acids and polyunsaturated fatty acids (PUFA; specifically, n-3 PUFA) decreases the risk of cognitive deterioration, decline, and impairment, and dementia [25]. On the contrary, poorer intellectual function is related to a reduced consumption of milk or dairy products, whereas the consumption of whole-fat dairy products may be associated with a higher risk of cognitive decline and deterioration among older adults [25]. Additionally, adherence to a healthy eating regimen and diet decreases oxidative stress, inflammation, and Aβ levels, which could subsequently lower the risk of dementia-like symptoms [26].
SMOKING CESSATION
Cigarette smoking is a major determinant of the development of dementia as it is associated with the extracellular deposition of amyloid plaques and peptides in the brain [27]. Findings on the effects of cigarette smoke components, such as nicotine, polycyclic aromatic hydrocarbons (PAHs), Cd(II), Cr(III), Pb(II), and Pb(IV) ions, on Aβ peptide aggregation revealed that all PAHs and metal ions modulated the Aβ aggregation process [27]. Furthermore, there is a significant relationship between active cigarette and tobacco smoking in older individuals with normal cognitive function and increased cerebral oxidative stress, while the association is smaller in those with dementia [27].
A study on active cigarette smoking in older individuals with normal cognitive function and possible dementia risk showed that smoking is related to increased oxidative stress in the central nervous system [28], while findings from a systematic review on the association between smoking and an increased risk of developing Alzheimer’s disease (AD) showed a relationship between smoking, nicotine exposure, and dementia-related neuropathology [29]. In addition, exposure to smoke is associated with an increased risk of negative preclinical and cognitive outcomes in younger and older adults [30], while recent evidence further implicates that medicinal nicotine is conceivably harmful to the neurodevelopmental condition in children and catalyzing processes underlying the neuropathology of AD; hence, smoking issues should be addressed by all public health workers [31,32].
AIR POLLUTION PREVENTION
Emerging evidence showed that increased exposure to airborne pollutants, such as particulate matter ≤2.5 μ, nitrogen dioxide or nitrous oxides, and carbon monoxide, was associated with an increased risk of dementia, while exposure to these air pollutants, even at low, reduced, and residential levels, was positively associated with a higher incidence of dementia [33-35]. Furthermore, findings from a longitudinal study on long-term exposure to air pollution and hospitalization due to dementia revealed a positive association between exposure to nitrogen oxides and ozone and hospitalization due to dementia [36]; meanwhile, results from similar studies on the association between fine particulate matter and ground-level ozone concentrations and amyloid positron emission tomography positivity in older adults with cognitive impairment revealed a positive association between higher fine particulate matter concentrations and brain amyloid plaques [37,38].
REDUCING/ELIMINATING ALCOHOL CONSUMPTION
Importantly, the diagnosis of an alcohol use disorder is strongly associated with a higher risk of dementia; however, the dose-response relationship between alcohol consumption and cognitive impairment remains unclear [39]. Findings from a systematic scoping review on alcohol use and dementia revealed that light to moderate alcohol use in middle to late adulthood was associated with a reduced risk of cognitive impairment and dementia, but heavy alcohol use was associated with changes in brain structures, cognitive debilitation and impairments, and an increased risk of all types of dementia [40,41]. In addition, a previous study showed that older adult drinkers are at high risk for cognitive deterioration, decline, and dementia [42], while the risk of dementia was increased in people who abstained from consuming alcohol in midlife or consumed >14 units per week [43]. The harmful amount of alcohol intake in many countries is >14 units per week; consequently, there is a proactive need for a downward revision of such guidelines to promote cognitive health in older ages [43]. In another study, total abstinence and intake of >14.0 drinks per week (compared with intake of <1.0 drink per week) was associated with reduced cognitive scores among study participants aged 72 years and older [44]. Findings from a study on the association of low to moderate alcohol drinking on cognitive functions from middle to old age among American adults revealed that <8 drinks per week for women and <15 drinks per week for men were positively associated with a consistently high cognitive function trajectory and a lower rate of cognitive decline, while low to moderate drinking was associated with decreased annual rates of total cognitive function decline, word recall, and vocabulary [45].
EXERCISING THE MIND AND SOCIAL ACTIVENESS
Engaging in stimulating activities, either intellectually, mentally, or socially, could protect individuals from developing dementia, indicating that social association, interaction, and intellectual stimulation could be pertinent in preserving mental alertness and functioning in older people [46,47]. Increasing evidence show that participation in cognitively stimulating recreational activities may help reduce the risk of cognitive impairment and dementia in the future [48-50]. Similarly, engaging in stimulating and exciting recreational activities is a protective measure against cognitive deterioration and decline and dementia in older people [51]. For instance, a study indicated that game-based interventions, specifically playing of video games, could improve cognitive abilities and functioning, such as executive functions in dementia patients and older adults. Additionally, the positive outcomes and impacts of moderate video gaming on gamers’ physical health have also been observed, for example, improvement in gait and balance [52].
Furthermore, playing video games could mitigate behavioral or mood disorders, and increase collaborations and interactions with friends, relatives, caregivers, guardians, and other patients; moreover, the beneficial effects of playing video games on social isolation, physical and cognitive decline, or deterioration are also impressive [53,54]. However, caution must be taken when playing video games and engaging in active gaming to prevent video game addiction, which results in health consequences that outwit the beneficial effects of moderate video gaming [55].
GOOD SLEEP HABITS
Epidemiologically, the onset of age-related neurodegenerative diseases such as AD and Parkinson’s disease is related to articulated sleep and rest disruption or disturbance, while emergent mechanistic studies propose that sleep interruption and disruption might be causally associated to the development of neurodegenerative diseases, suggesting that adequate rest and sleep may be a viable therapeutic or remedial target in preventing these events [56]. In addition, sleep disruption is a major component of early dementia because insufficient sleep facilitates the accumulation of Aβ [57,58]. Furthermore, the core manifestations of persistently disrupted sleep and circadian rhythms can weaken or impair memory and hippocampus-dependent learning; sleep disturbance is also a risk factor for early dementia [59]. Importantly, findings of previous studies on the impact of poor sleep quality on subjective cognitive decline or related functional difficulties have indicated that poor sleep quality may lead to cognitive, functional, or ability decline [60].
Habitual short (≤6 hours/night) or long (≥8 hours/night) sleep duration (against 7 hours/night) may increase the future risk for developing cognitive impairments, including dementia, independent of the vascular risk factors by 36% and 35%, respectively, in older women; meanwhile, various forms of sleep conditions or parameters such as insomnia, fragmentation, daytime dysfunction, prolonged latency, rapid eye movement sleep behavior disorder, and excessive time in bed were linked to a higher risk of all-cause cognitive disorders. Consequently, adequate sleep management is considered a viable option for dementia prevention [61-64].
Moreover, sleep apnea, which affects 17% of 50–70-year-old men and 9% of 50–70-year-old women, increases the risk of hypertension, stroke, myocardial infarction, and atrial fibrillation, and is closely linked to vascular dementia [65]. In addition, findings from studies on self-reported sleep apnea and dementia risk indicated that sleep apnea may increase the risk of dementia by 66% in the absence of the apolipoprotein E (APOE) ε4 allele, which may be helpful in the prevention of dementia or AD in older men with sleep apnea [66].
Importantly, treating various sleep problems is beneficial to improving cognitive health because treating sleep disorders in older patients prevents and delays the onset of dementia, mitigates the progression of symptoms in people who already manifest dementia symptoms, and even reverses neurodegeneration in specific brain areas [67].
CONTROLLING HEALTH RISKS
Before the midlife stage, individuals should provide adequate attention to improving their overall health. For instance, hypertension presents a higher risk factor for cognitive decline and various forms of dementia [68]. In addition, elevated concentrations of low-density lipoprotein cholesterol (>121 mg/dL), which is a risk factor for other numerous noncommunicable diseases, is a potential risk factor for AD, and this association is stronger among individuals aged 60–70 years [69,70]. Furthermore, diabetes is also a risk factor for dementia and other neurological conditions [71]. In addition, presbycusis (hearing loss) is one of the causes of various human cognitive disorders and increases the risk of dementia in older people [72].
PREVENTION OF INFECTION
A positive correlation exists between Helicobacter pylori infection and dementia [73]. Strong evidence also revealed that herpes simplex virus type 1 is a significant risk factor for AD through the intermittent reactivation of APOE gene by immunosuppression, peripheral infection, and inflammation [74]. In addition, the number of cases of human immunodeficiency virus (HIV)-related neurocognitive disorder and HIV-related myelopathy has increased in patients with advanced immunosuppression due to HIV infection [75].
Findings from a meta-analytic study revealed that Toxoplasma gondii infection could be considered as a risk factor for AD and could exacerbate its symptoms [76], while infections caused by Botrytis cinerea, Cryptococcus curvatus, Alternaria, Botrytis, Candida, Cladosporium, and Malassezia are major risk factors for AD [77].
Furthermore, cytomegalovirus and herpes simplex virus type 1 are risk factors for the development of AD through their probable effects on the immune system [78]. Likewise, neurosyphilis, a bacterial infection caused by Treponema pallidum, can cause significant variations in neuropsychiatric signs and symptoms in individuals [79]; meanwhile, parasitic infestations mostly found in places with poor sanitation, which can cause neurocysticercosis in the brain, is also a risk factor for dementia [80].
STRESS PREVENTION
Several studies have highlighted the association between stress and dementia. The risk of dementia is higher in persons with stress disorders than in those without, while a higher rate of dementia was recorded in men with stress disorders than in women who had higher rates of posttraumatic stress disorder [81]. In addition, midlife work-related stress increases the risk of mild cognitive impairment, dementia, and AD in later life [82]. Furthermore, post-traumatic stress disorder and depressive disorders are associated with an increased risk of dementia [83]. To this end, the implementation of appropriate stress management measures will help mitigate these effects [84].
AVOIDANCE OF INJURIES
There is a long history linking traumatic brain injury (TBI) with the development of dementia. TBI occurs when a force transmitted to the head causes neuropathologic damage and impairment of brain function, which increases the risk of developing AD, Parkinson’s disease, and chronic traumatic encephalopathy, and is also a risk factor for sporadic amyotrophic lateral sclerosis [85]. In summary, through several potential mechanisms, a single moderate-to-severe TBI increases the risk of AD, repetitive and mild TBI increases the risk of chronic traumatic encephalopathy, and TBI may be a risk factor for other neurodegenerative disorders that are associated with dementia [86].
PREVENTING THE IMPACTS OF SOCIAL ISOLATION AND LOCKDOWN
As social isolation or loneliness is associated with a 40% increased risk of dementia regardless of gender, race, ethnicity, education, and genetic risk [87], people, especially older adults should not be neglected or left alone. In addition, perceived loneliness is a significant risk factor for all-cause dementia, especially for AD; hence, paying attention to the subjective reports of loneliness among older adults could help prevent this condition, while the lack of social interaction with others is also associated with risks of dementia [88,89]. To this end, the general prevention of loneliness and isolation is essential in achieving overall cognitive health [90].
PREVENTION OF DEPRESSION
The odds of developing all-cause dementia is higher in people with a history of depression and anxiety than in those with no history of these conditions, while a high level of depressive symptoms is associated with a 50% increased risk of dementia [91,92]. In addition, depressive symptoms may be both a risk factor for and a harbinger of dementia, as an increase in the number of depressive symptoms is associated with a higher risk of dementia than a decrease in the number of depressive symptoms [93,94]. In addition, findings from previous studies on the association of depressive symptoms with a decline in cognitive function-Rugao longevity and aging revealed that people with deteriorating levels of depression tended to experience a rapid decline in cognitive and intellectual abilities than those with steady depression [95].
Furthermore, major depressive disorder is a significant risk factor for the onset and aggravation of dementia, and patients with this type of condition exhibiting different subtypes of mild cognitive impairment typically show beta-amyloid deposition on brain imaging; a high prevalence of minimal cognitive impairment was also evident among older depressed patients, and depressed patients with minimal cognitive impairment showed heterogeneously elevated 18F-florbetapir retention compared with depressed patients without minimal cognitive impairment [96,97]. These findings support the hypothesis that a higher amyloid burden is associated with poorer memory performance and higher susceptibility to the development of AD in the future.
CONTINUING EDUCATION
A previous study showed that cognitively stimulating activities performed during middle adulthood might have a protective effect on the brain by boosting the cognitive reserve; results of available studies further demonstrate that cognitive reserve is increased through continuing education, which lowers the incidence of dementia [98]. Furthermore, findings from a previous study on education and adolescent cognitive ability as predictors of dementia revealed that continuing education and maintaining a good cognitive ability can decrease the risk of dementia independently of one another, and an increase in educational attainment may offset the dementia risk due to improved cognitive abilities [99].
DISCUSSION
Over the years, scientists have been able to proffer some alternative preventive measures for dementia; nevertheless, by 2030 and 2050, 82 million and 152 million people worldwide, respectively, are predicted to be living with dementia due to the rising number of cases in underdeveloped and developing countries. Again, these statistics affirm the envisaged future seriousness and additional medical burdens likely to ensue from the condition.
Presently, as the coronavirus disease 19 pandemic continues, social isolation and lockdowns are some of the measures implemented to abate the spread of the virus [100]; however, these measures might increase or aggravate the number of dementia cases worldwide. While most cases of dementia are reported in Asia, Western Europe, and North American countries, future cases are expected to soar in the coming years in other regions and continents of the world; thus, concerted efforts of all health practitioners are needed to mitigate this occurrence.
As a neurological and chronic condition, dementia exerts both financial and mental health burdens on the patients and their loved ones. The primary healthcare system and nursing homes are also exhausted and impacted in dealing with cases of dementia; furthermore, the healthcare budgetary allocations of some specific countries for the treatment and management of dementia cases are also increasing on a yearly basis.
Although dementia mostly affects older populations, this condition should not be associated or mistaken as a normal part of aging. Dementia is commonly caused by a damage in the brain or its components. There are other numerous factors that can cause dementia; some are reversible once the conditions are treated, while others cannot be reversed but can be prevented.
Importantly, AD is well documented as the most common type of dementia. The stages of AD vary and can be described hierarchically, that is, low to moderate to severe, and includes: no cognitive impairment, very mild cognitive decline, mild cognitive decline, moderate cognitive decline, moderately severe cognitive decline, severe cognitive decline, and very severe cognitive decline. In most cases, non-pharmacological interventions are mostly beneficial in reversing, delaying, and improving the health conditions of patients in most stages of AD, except in patients with extremely severe cognitive decline as they tend to lose their ability to communicate or respond to their environment [101,102].
Since the attention and priorities of health practitioners are to repress the occurrence of dementia globally, joint efforts should be geared toward the prevention of this condition as there are no effective pharmacological interventions available for the permanent treatment of dementia. Notably, preventive interventions for dementia are less expensive, adoptable, and effective, and only involve behavioral and lifestyle changes. The changeable risk factors for dementia are usually the main focus in the probable and workable preventive efforts of health educators and other health practitioners in order to manage dementia; other cognitive problems, summaries, and key points to this effect are provided in Table 1.
CONCLUSION
There is a growing emphasis on strategies to prevent dementia globally [103]. This review concludes that participating in regular physical activities, healthy eating and dieting, avoiding all forms of smoking, avoiding air pollutants, halting or reducing alcohol consumption, exercising the mind and being socially dynamic, getting enough rest and establishing good sleep habits, infection prevention, stress prevention, avoidance of injuries, prevention of the effects of social isolation and lockdowns, continuing education, and depression prevention are viable protective measures against the development of dementia.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
Great thanks and appreciations to my mentor Prof. R. Marks, Teachers College, Columbia University, New York, the United States who helped to proofread the initial full manuscript for appropriateness, and offered valuable suggestions. Thanks and appreciations go to all the scientists whose studies have been discussed in this article; also, great appreciation is given to the anonymous reviewers of this journal for their valuable suggestions.