Association between Serum Folic Acid Levels and Asthma in the Korean Population: A Study Based on the 2016–2018 Korea National Health and Nutrition Examination Survey
Article information
Abstract
Background
Folic acid is involved in inflammatory reactions; however, the association between folic acid and allergic diseases, particularly asthma, remains unclear. Thus, this study aimed to evaluate the association between serum folic acid levels and asthma in Koreans.
Methods
This study analyzed the serum folic acid levels of 6,615 individuals included in the 2016–2018 Korea National Health and Nutrition Examination Survey. The prevalence of asthma was determined using a questionnaire that identified cases of physician-diagnosed asthma. The relationship between serum folic acid levels and asthma was analyzed using logistic regression analysis.
Results
Multiple logistic regression analysis showed that a 1 ng/mL increase in serum folic acid level significantly reduced the risk of asthma after adjusting for confounding factors including sex, age, household income, current smoking, current alcohol use, and body mass index (odds ratio [OR], 0.930; 95% confidence interval [CI], 0.876– 0.987; P=0.017). The relationship between the adjusted odds of asthma and serum folic acid levels were consistently inverse (OR, 2.266; 95% CI, 1.126–4.420; P for trend=0.038).
Conclusion
Serum folic acid levels are inversely associated with physician-diagnosed asthma in the Korean population.
INTRODUCTION
The prevalence of allergic diseases, particularly asthma, is on the increase. Asthma is a chronic disease with various etiologies and is expected to become more prevalent in the future. As a society develops, the prevalence and socioeconomic burden of asthma worsens. Approximately 339 million people worldwide have asthma, and in Korea, the prevalence of asthma continues to increase [1]. Factors responsible for the increase in the prevalence of asthma include increased air pollution caused by industrialization [2], changes in indoor living conditions, and exposure to allergens [3]. However, the factors that account for this trend remain unclear. Given that this trend occurs within a short period, attention should be paid to changes in environmental factors, such as dietary patterns.
One notable factor in dietary patterns is folic acid [4]. Folic acid, otherwise known as vitamin B9, is a water-soluble vitamin. It is involved in purine, pyrimidine, and amino acid synthesis, and is a source of methyl donors for DNA methylation [5]. Through gene-environment interactions, the pathogenesis of asthma causes epigenetic changes, including DNA methylation [6]. Folic acid plays a role in inflammatory reactions [7]. Low folic acid levels increase the risk of cardiovascular disease [8], inflammatory bowel disease, and rheumatoid arthritis [9]. However, the association between folic acid and allergic disease is uncertain.
Low folic acid levels are associated with increased risks of atopy and wheezing [4,10]. In Denmark, a low serum folate level is significantly associated with physician-diagnosed asthma [11]. However, other studies have reported no significant association between serum folic acid levels and physician-diagnosed asthma [4,12,13].
Folic acid and allergic diseases, including asthma, have been extensively reported, but available results are conflicting; thus, their association remains unclear. To our knowledge, research on folic acid levels and asthma among Asians with different dietary patterns from Westerners remains insufficient. Therefore, this study aimed to evaluate the relationship between serum folic acid levels and asthma in Koreans.
METHODS
1. Study Population
This study used data obtained from the 2016 to 2018 Korea National Health and Nutrition Examination Survey (KNHANES). KNHANES is a nationally representative survey that was reviewed and approved the Institutional Review Board of Pusan National University Yangsan Hospital (IRB no., 05-2021-135).
The KNHANES (2016–2018) included 7,191 patients aged >10 years whose serum folic acid levels were measured. Patients with missing values in the variables of interest and potential confounders, and those diagnosed with malignancies that may affect folic acid metabolism were excluded. Finally, 6,615 subjects were included in the analysis.
2. Data Collection and Measurements
Serum folic acid levels were measured using ARCHITECT i4000Sr (Abbott, Chicago, IL, USA) by chemiluminescent microparticle immunoassay. Asthma was confirmed if the patient was diagnosed by a physician, corresponding to the question, ‘Have you ever been diagnosed with asthma by a physician in your life?’
In measuring the household income levels, we divided the average monthly household income by the number of household members and classified the results as “high,” “mid-high,” “mid-low,” and “low” according to the quartile. Compared to drinkers, non-drinkers referred to those who had not been drunk at all in the past year. Cigarette smoking was indicated as “yes” for participants who were current smokers. Body mass index (BMI) was classified as normal or underweight (<23 kg/m2), overweight (23–25 kg/m2), or obese (≥25 kg/m2), according to the modified World Health Organization criteria for the Asia-Pacific region.
3. Statistical Analyses
All statistical data were analyzed using complex sample analyses according to the statistical guidelines of the Korea Centers for Disease Control and Prevention for analyzing raw data from the KNHANES. The relationship between categorical variables according to the presence of asthma was analyzed using the chi-square test. The association between serum folic acid levels and the risk of asthma was evaluated using multiple logistic regression analysis. Model A was unadjusted. Model B was adjusted for gender and age. Model C was adjusted for sex, age, household income, alcohol consumption, smoking, and BMI. The risk of asthma was also determined using multiple logistic regression analysis, separating the serum folic acid levels into quintiles. The results were expressed as odds ratios and 95% confidence intervals. All statistical analyses were performed using IBM SPSS ver. 22.0 (IBM Corp., Armonk, NY, USA). Differences with P-values <0.05 were considered statistically significant.
RESULTS
1. Study Patient’s Baseline Characteristics
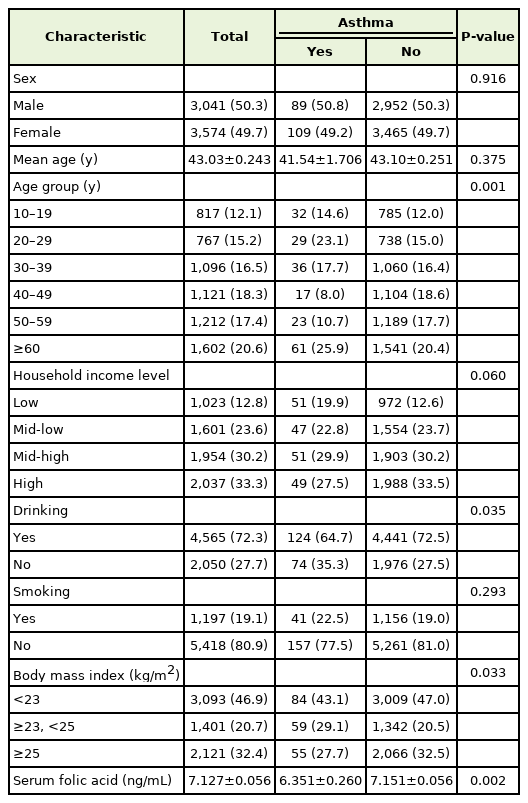
The general clinical characteristics of patients with asthma and those of controls are summarized in Table 1. The study included 6,615 participants, comprising 3,041 male and 3,574 female participants. The mean serum folate level was 7.127 ng/mL, with 6.351 ng/mL in the asthma group and 7.152 ng/mL in the non-asthma group, showing a statistically significant difference (P=0.002). The average age of the participants was 41.54 and 43.10 years in the asthma and nonasthma groups, respectively. Most participants consumed alcohol and 1,197 smoked cigarettes (19.1%). Regarding BMI, 2,121 participants (32.4%) were obese.
2. Relationships between Serum Folic Acid Levels and Asthma
Logistic regression analysis showed that the risk of asthma decreased by 0.930 as the serum folic acid levels increased by 1 ng/mL in model A (Table 2). In models B and C, which were adjusted for confounding variables, a higher serum folic acid level was associated with lower odds of asthma (P=0.011 and P=0.017, respectively). A consistently inverse relationship was noted between the adjusted odds of asthma and quintiles of serum folic acid levels (Table 3). The lower the serum folic acid level, the higher the risk of asthma (P for trend=0.038). The ORs in the first, second, and fourth quintile groups were 2.266 (95% CI, 1.162–4.420), 2.131 (95% CI, 1.193–3.807), and 2.206 (1.126–3.646), respectively. Consequently, the odds of asthma were 2.26 times higher in the quintile group with the lowest folic acid levels than in the quintile group with the highest folic acid levels.
DISCUSSION
This study aimed to investigate the relationship between serum folic acid levels and asthma in the Korean population. We specifically examined people aged >10 years with no history of cancer affecting folic acid metabolism. Our multiple logistic regression analysis showed that the risk of asthma decreased as serum folic acid levels increased. We also observed the serum folic acid level in quintiles to assess the risk of asthma. Similarly, the asthma risk significantly increased when the serum folic acid level decreased. Therefore, serum folic acid levels were inversely associated with the risk of physician-diagnosed asthma.
Our findings are consistent with those of previous studies [11,14], which stated that serum folate levels were inversely correlated with the odds of asthma. In Denmark, a study involving 6,784 adult participants aged 30–60 years reported that folate deficiency was significantly associated with self-reported physician-diagnosed asthma (OR, 1.37; 95% CI, 1.05–1.79) [11]. In another cross-sectional study involving 8,083 children and adults aged 2–85 years in the US, serum folate levels were inversely associated with wheezing (OR, 0.6; 95% CI, 0.4–0.8) or atopy (OR, 0.7; 95% CI, 0.6–0.9), but no significant association with physician-diagnosed asthma was observed [4]. However, folate levels and asthma were not significantly associated in a case-controlled study in Egypt [12]. These differences in outcomes could be based on racial or sociological characteristics or caused by research errors; therefore, further research is required. In another Korean study, folic acid levels were not significantly different between groups with and without a history of acute asthma exacerbation in patients above the age of 65 years [15].
Some studies have reported an association between folic acid intake and asthma. A large case-control study of 1,030 UK adults found that the dietary intake of folic acid was inversely associated with physiciandiagnosed asthma (OR, 0.89; 95% CI, 0.89–0.98) [16]. In the 2019 KNHANES, the average daily folic acid intake was 80.7% of the recommended intake (men, 88.2%; women, 73.2%) [17]. Given that the association between folic acid and asthma is increasingly elucidated, folic acid intake needs to be improved.
This study had some limitations. First, the KNHANES has a crosssectional study design that makes it difficult to determine the direct causal relationship between folic acid levels and the pathophysiology and metabolism of asthma. Second, serum folic acid levels were collected once; therefore, they did not accurately reflect long-term folic acid conditions. Since it was not possible to confirm whether there was wheezing or asthma symptoms/attacks to evaluate current asthma symptoms, the study used a lifetime history of asthma, not the present. Therefore, it may be difficult to determine an exact association with the current state, which may require further investigation and research. Third, we did not examine the dietary folate intake of the participants. Fourth, comorbid conditions that could have affected folic acid were not excluded; moreover, the metabolism of folic acid is disrupted in patients with cancer [18]. Despite these limitations, the KNHANES is a strictly quality-managed program compared to other studies and data; hence, this study obtained an objective result. Furthermore, our study is a domestic study that used a large and representative sample of Koreans; thus, our research results can be generalized to all Koreans.
In conclusion, serum folic acid levels are inversely associated with asthma in Koreans above the age of 10 years. However, further research is needed to determine the cause-and-effect relationship between folate and asthma, and the potential role of folate supplementation in the primary prevention and treatment of allergic diseases.
Notes
CORRECTION
This article was corrected on November 29, 2023 for an author affiliation.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported by a 2021 research grant from Pusan National University Yangsan Hospital.