Association between Undergraduate Education for Community-Based Medicine and General Practice Majors: A Longitudinal Study in Japan
Article information
Abstract
Background
There is a shortage of general practitioners in Japan. With the revision of educational guidelines, general practice (GP) education has improved. However, the amount of education on GP in medical schools remains inconsistent. This study examined the relationship between medical students’ amount of GP-related education and their subsequent choice of GP majors.
Methods
A retrospective cohort study was conducted in a teaching hospital in Japan. Participants were residents in the hospital. The exposure comprised compulsory lectures and training time for community-based medicine in medical schools. The outcome included participants choosing GP majors after their initial 2-year junior residency.
Results
Fifty-one participants were included in the final analysis. Of these, 14 majored in GP and 37 in non-GP after their initial 2-year junior residency. Of the participants who took GP lectures for 18 hours or more, 11 chose GP majors, and 18 chose non-GP majors (risk ratio, 2.78; 95% confidence interval [CI], 0.88–8.79). Of the participants who underwent training for 12 days or more, 10 chose GP majors, and 16 chose non-GP majors (risk ratio, 2.40; 95% CI, 0.87–6.68).
Conclusion
The results do not support the association between the amount of compulsory undergraduate education for community-based medicine and the subsequent increase in the number of residents choosing GP majors in Japan. Educators would do well to explore different approaches, such as improving the quality of education to increase the number of GP residents. Further research is needed to reach more definitive conclusions.
INTRODUCTION
There is a need for more general practitioners in Japan. This shortage can be explained by the expanding demand in Japan’s aging society and insufficient supply [1]. Traditionally, general practice (GP) and family medicine (FM) remain unfamiliar in Japan. Instead, specialists frequently provide primary care [2]. Furthermore, board certification for FM or GP did not exist in Japan until the Japan Primary Care Association (JPCA) introduced board certification for FM in 2009. In 2018, a new board certification for GP by an independent third-party organization, the Japanese Medical Specialty Board, was launched [1]. Residents who finish a GP residency in this new system can take the JPCA’s FM certification exam as a subspecialty. As of 2022, there are 1126 JPCA-certified family physicians in Japan and no general practitioners from the new specialty system [3]. The number of new GP residents who began residency in 2022 was 250, comprising only 2.65% of the total [4].
Undergraduate education for GP in Japan has changed over the last 20 years. Japanese medical schools require the completion of a 6-year program. Residents who receive their medical license after graduation will start a 2-year junior residency and a subsequent residency program consisting of a specialty of their choice. Medical students receive an education based on the Model Core Curriculum published by the Ministry of Education, Culture, Sport, Science, and Technology in 2000 and revised in 2007, 2010, and 2016 which serves as a guideline for medical education in Japan [5]. The curriculum’s section on GP skills has been expanded with each revision; however, there is no specific mention of the minimum education time required. Furthermore, some schools’ curricula have not been changed, while changes have been delayed in other schools [6]. Also, the contents of one-third of the educational program are designed according to the discretion of each school [6]. Therefore, there are several differences in the GP-related education offered at each medical school.
Notably, several studies have evaluated the influence of undergraduate education on students’ subsequent choice for GP majors [7]. A review published in 2015 identified two main limitations in previous studies that examined this relationship [8]. Firstly, many previous studies used substitute outcomes such as students’ career intention after GP clerkships rather than the actual number of graduates who choose GP for their career [9]. Secondly, most educational programs that showed positive outcomes were elective or used specific recruitment procedures for student selection, which may have led to a selection bias [10]. Therefore, this study aimed to examine the relationship between the amount of GP-related education taught to medical students and their subsequent choice for GP majors, using more appropriate measurements than those employed in previous studies. Thus, we used compulsory GP-related undergraduate education time as the exposure and the number of graduates who chose a GP residency program as the outcome.
METHODS
1. Study Design
We conducted a retrospective cohort study in a teaching hospital in Japan. Following the Strengthening the Reporting of Observational Studies in Epidemiology guidelines, we reported this study [11]. The Japanese Medical Specialty Board agreed on “General Medicine” as the English name for the new board; however, it covers both the competencies of general medicine in hospitals and GP in clinics. Therefore, this paper defines the certified individual as a general practitioner. Also, as the JPCA’s FM certification is categorized as a GP subspecialty, we described GP as inclusive of FM in this paper.
2. Setting and Participants
The Okinawa Prefectural Chubu Hospital is located in Okinawa, Japan. It is a core hospital in the region; it has 559 beds and accepts approximately 30 junior residents for a 2-year junior residency program each year. The program offers 2 years of super-rotating training, which allows all junior residents to undergo basic clinical training in almost all specialties, including internal medicine, general surgery, emergency medicine, anesthesiology, obstetrics and gynecology, and pediatrics, regardless of junior residents’ desired future career. After the 2-year program, about 15 residents continue their training in the same hospital and choose a residency program. Residents who completed this initial 2-year junior residency training in Okinawa Prefectural Chubu Hospital during 2017–2021 and had chosen their residency major as of May 2021 were eligible for recruitment in this study.
3. Main Exposure
As a proxy of the amount of GP education, we established education time for “community-based medicine” as the main exposure. Currently, in Japan, there is no accurate indicator to evaluate the amount of GP education in medical school, as education by general practitioners in medical schools has not been sufficiently widespread [12,13]. However, one of the definitions of general practitioners in Japan is “doctors who serve the community.” [1] Therefore, since general practitioners play an essential role in supporting community-based medicine [14], there is considerable overlap between community-based medicine and GP regarding education [15]. Consequently, we used data on education for “community-based medicine” as the main exposure.
To collect information on participants’ educational experience with community-based medicine in medical schools, we used data from the national survey conducted by the Japanese Council for Community-based Medical Education in 2011, 2014, and 2019 [13,16,17]. As this survey gave us information on lecture and training times at each grade in each medical school, we calculated participants’ total amount of education time by adding up the numbers listed. We only collected information at three-time points, so we adopted mean values for the rest of the applicable years. Furthermore, regarding lecture time, answers were collected using “units” instead of “hours.” In this study, we used “hours” by calculating one unit as 90 minutes since almost all medical schools adopt 90 minutes as a standard for one lecture unit. We dichotomized lecture and training time by the median.
4. Outcome Measure
The primary outcome was whether participants majored in a GP residency program after their 2-year junior residency.
5. Other Explanatory Variables
We surveyed to evaluate other explanatory variables. We created an anonymized questionnaire using Google Forms (Google LLC, Mountain View, CA, USA). Next, we requested representatives from each grade to distribute the Uniform Resource Locator of the questionnaire to eligible candidates through a closed social networking system. In the questionnaire, we collected data on respondents’ age [18], gender [19], family structure, hometown [20], and parents’ occupation [18,21], which we considered as confounding factors following prior studies. Regarding their hometown, we classified participants into “metropolitan area” and “non-metropolitan area” after defining the former as a prefecture which included the central city of a metropolitan area according to the 2015 national census [22]. We also asked the candidates whether they entered their medical school through regional admission, as we thought this factor could influence both the primary exposure and the outcome following prior studies [23]. We classified all graduates from Jichi Medical University as “regional admission,” as graduates from Jichi Medical University have their obligation term wherein they are required to render a certain amount of work at designated local medical facilities like many other regional admission applicants of other universities.
In addition, we collected other data, including participants’ desired career at some point in the past [18,19], workplace preference [18,20,23], thoughts on GP, and experiences in medical school. Finally, we investigated a few factors that participants considered necessary when they chose their careers, such as intellectual curiosity [24], future potential of the career [25], high level of expertise [21], a broad spectrum of practice [20], ability to treat a wide range of patients [18], high income [26], respect from others [24], work-life balance [23,26], research opportunity [26], and continuity of care [18]. We used a five-point Likert scale for this part of the questionnaire; scores of 4 or higher were considered significant.
6. Study Size
Because of this study’s exploratory nature, we included all eligible participants.
7. Statistical Analysis
First, we performed descriptive analysis to show the participants’ demographic characteristics. We compared these characteristics by the outcome in GP residents and non-GP residents. Next, we performed univariate analysis to evaluate the relationship between the primary exposure and the outcome. In addition, as some of the graduates from Jichi Medical University in Okinawa were expected to choose GP as their major, we conducted a sensitivity analysis excluding graduates from Jichi Medical University. We used Fisher’s exact test to calculate P-values as all factors were categorical variables. Finally, we performed a logistic regression analysis. We adjusted confounders frequently found in previous studies—age [18], gender [19], hometown [20], regional admission [23], and desired working location in the future [18,20,23]. Statistical significance was set at a P-value of <0.05. The statistical analyses were performed using Stata/EP software ver. 17.0 (Stata Corp., College Station, TX, USA).
8. Ethical Considerations
The research ethics committee of the Okinawa Prefectural Chubu Hospital approved this study (reference number: 2021 中部研究倫理第8号). Before using the data from the national survey conducted by the Japanese Council for Community-based Medical Education, we contacted the council for approval. As these data did not include any personal information, we received approval upon explaining the purpose of the study to the council. The questionnaire used in the survey was anonymized; we obtained participants’ informed consent before they responded to the survey.
RESULTS
1. Baseline Characteristics
Residents who had completed the 2-year junior residency program at Okinawa Prefectural Chubu Hospital during 2017–2021 and had chosen their residency program in the hospital as of May 2021 were the study’s target group. Of these 76 residents, 51 were included in the final analysis as study participants (Figure 1). One research administrator was excluded before the research started, 23 candidates did not respond to the questionnaire, and one had graduated from a foreign medical school and was excluded as we did not have the school’s educational information.
Table 1 describes the characteristics of the study participants. We show the demographic characteristics according to the main outcome. Of the 51 participants, 14 were GP residents, and 37 were non-GP residents. There were no missing data for any of the variables. There were no significant differences between the two groups in the post-graduate year, age, gender, family structure, hometown, parents’ occupation, and timing of career decision.
Furthermore, 8 (57%) of the 14 GP residents and 8 (22%) of the 37 non-GP residents entered their medical schools via regional admission. Regarding participants’ desired careers during medical school and the junior residency program, three GP residents and two non-GP residents wanted to choose GP as their major in their first year of medical school. However, six GP residents and one non-GP resident wanted to major in GP in the first year of the junior residency program. Therefore, the number of candidates for GP residency increased from three to six during medical school and from six to 14 during the junior residency program.
Table 2 shows the results for participants’ workplace preferences, thoughts on GP, and reflections on their time in medical school. Eight participants (57%) in the GP-residents group and 6 (16%) in the non-GP residents’ group (risk ratio, 3.52; 95% confidence interval [CI], 1.49–8.34) preferred working in remote areas. Further, 12 (86%) of the GP residents and 8 (22%) of the non-GP residents chose to work in clinics or small hospitals rather than large hospitals or other institutions (risk ratio, 9.30; 95% CI, 2.32–37.24). As for participants’ opinions on the future of GP, 13 of the GP residents (93%) and 27 of the non-GP residents (73%) thought it was promising. For the item on whether participants knew seniors in medical school who exhibited a good understanding of GP, eight of the GP residents (57%) and 26 of the non-GP residents (70%) answered “yes.” Conversely, 10 GP residents (71%) and 20 non-GP residents (54%) had heard negative opinions about GP from their seniors. Regarding their education in medical school, less than half of each group—five GP residents (36%) and 15 non-GP residents (41%)—thought they had enough opportunities to learn about GP.

Participants’ workplace preferences, thoughts on GP, and reflections on their time in medical school
Table 3 shows the factors that influenced participants’ career choices. There were no differences between GP and non-GP residents regarding the future potential of their career, high level of expertise, a broad spectrum of practice, ability to treat a wide range of patients, respect from others, work-life balance, research opportunity, and continuity of care. However, intellectual curiosity and high income were considered more important among non-GP residents, compared with GP residents—as indicated by 34 (92%) and 11 (30%) non-GP residents, and 9 (64%) and zero (0%) GP residents, respectively.
2. Main Outcome
Table 4 describes the study’s primary. We calculated lecture and training time for community-based medicine in each participant’s medical school. We evaluated the association between the amount of undergraduate education and residents’ subsequent choice for a GP major. The median dichotomized lecture time and training time, as distributions were skewed and did not follow a normal distribution. The median lecture time was 18 hours, and the median training time was 12 days.
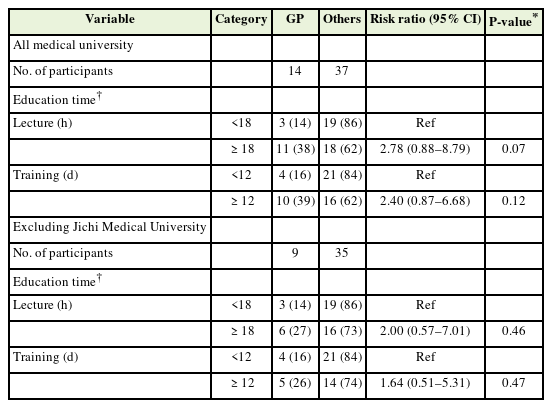
Association between the amount of education for community-based medicine in medical schools and students’ choice for a GP major after residency
Of the participants with lecture times of 18 hours or more, 11 chose a GP major, and 18 chose a non-GP major (risk ratio, 2.78; 95% CI, 0.88–8.79). Of the participants who underwent training for 12 days or more, 10 chose a GP major, and 16 chose a non-GP major (risk ratio, 2.40; 95% CI, 0.87–6.68).
We then conducted a sensitivity analysis excluding graduates from Jichi Medical University. In total, 44 participants were included in this analysis. Of the participants with lecture times of 18 hours or more, six chose a GP major, and 16 chose a non-GP major (risk ratio, 2.00; 95% CI, 0.57–7.01). Similarly, among the participants who underwent training for 12 days or more, five chose a GP major, and 14 chose a non-GP major (risk ratio, 1.64; 95% CI, 0.51–5.31). In the logistic regression analysis, the adjusted odds ratio was 1.02 (95% CI, 0.98–1.05) for lecture time and 1.07 (95% CI, 0.98–1.20) for training time.
DISCUSSION
1. Main Results
We conducted a retrospective cohort study in a teaching hospital in Japan. Lecture and training times for community-based medicine were not associated with increased residents’ choice of GP residency programs. Therefore, the findings of this preliminary study do not support an association between the amount of compulsory education for community-based medicine in medical schools and the subsequent increase in the number of residents choosing GP majors in Japan.
2. Comparison with Existing Literature
Notably, several foreign studies have addressed similar research questions to those of this study. In New Zealand, a university introduced a 7-week rural undergraduate practice in one of its three medical schools and examined the number of graduates working in a rural area 10 years later [27]; the results showed no significant differences among schools vis-à-vis the proportion of graduates working in rural areas (6% in the experimental group versus 14% and 4% in the control group, P=0.155). These results are consistent with ours. In Germany, an observational study conducted in a medical school showed positive associations between undergraduate GP course participation and GP career choice; the courses included a pre-clinical GP elective (odds ratio, 2.6; 95% CI, 1.3–5.3), a 4-week GP clerkship (odds ratio, 2.6; 95% CI, 1.3–5.0) and a 4-month GP clinical rotation during the final year (odds ratio, 10.7; 95% CI, 4.3–26.7) [18]. The study showed positive results; however, there might have been a selection bias because the GP courses were elective. In other words, medical students who wanted to become general practitioners might have chosen undergraduate GP courses. An ecological study in the United Kingdom found a statistically significant association between the quantity of GP teaching in medical schools and the proportion of graduates who selected GP training programs in 2014 (correlation coefficient=0.41, P=0.027) and in 2015 (correlation coefficient=0.3, P=0.044) [28]. In the study, the influence of outliers could be significant. In addition, it only showed a correlation but not a causal relationship. A meta-analysis conducted in 2021 showed that medical students who participated in pre-clerkship GP placements were more likely to choose an FM residency compared with matched controls (risk ratio, 1.62; 95% CI, 1.03–2.55; I2=74%) [7]. However, among the 11 studies analyzed, 10 were conducted in the United States, and eight were published more than 10 years ago. Therefore, we cannot directly adapt their results to present-day Japan.
3. Result of Other Demographic Data
It is difficult to conclude from the results of variables other than the main factor. Nevertheless, when we compared some of the participants’ characteristics with those of previous studies, some items showed the same tendency as those in previous studies.
Our study did not find significant age differences in residents’ final choice for a GP major; however, the literature suggested that those who pursued a GP program were older than those who did not [18]. A study reported that women were more likely to aspire to become general practitioners [19], but this was not the case in our study. As in a previous study [23], the present study found that participants who entered their respective schools through regional admission were more likely to major in GP. A study found that students who majored in GP had chosen their major earlier than those who did not [19]; however, we did not observe such a tendency in this study. Regarding workplace preference, prior studies have indicated that “rural,” “small towns,” and “less hospital-oriented” areas were preferred by those majoring in GP [18,20,23]; similar results were observed in the present study.
Furthermore, our survey included questions on the attitude of senior doctors in medical schools toward GP. Notably, previous studies suggested that good mentors had positive effects. However, senior doctors’ comments about GP negatively affected residents’ preference for GP majors [29]; this study found no significant differences.
Regarding factors that participants considered necessary when they chose their career, “ability to treat a wide range of patients,” “work-life balance,” and “continuity of care” showed higher percentages in the GP group than the non-GP group. In particular, the “ability to treat a wide range of patients” and “continuity of care” relate to the philosophy of primary care, especially regarding comprehensiveness and continuity. Therefore, it is unsurprising that these items were considered necessary by those who majored in GP; these results are consistent with a prior study [18].
4. Strengths and Limitations
Regarding this study’s strengths, this is the first longitudinal study in Japan examining the relationship between community-based medicine education in medical schools and students’ subsequent choice for GP majors. We calculated students’ total education time for community-based medicine based on raw data from each medical school. In addition, we set up our primary outcome as the actual number of residents who chose a GP residency, as opposed to students’ career intentions.
This study has some limitations. First, due to the lack of similar prior literature in Japan, we could not calculate the sample size in advance, and it may be that the size was insufficient to detect significant differences in the results. Second, as this study was a single-center study, the generalization of our results to other Japanese residency programs is limited. However, as education during students’ initial 2-year junior residency program could constitute another confounding factor, conducting this study in a single site helped eliminate this potential factor. Third, regarding the national survey conducted by the Japanese Council for Community-based Medical Education, the interpretation of “community-based medicine” may have differed among respondents from different medical schools; education time which was not considered as community-based medicine in one medical school, may have been considered as such in another. Fourth, although we performed a logistic regression analysis to adjust possible confounders, events per variable were <10. This could influence the stability of the logistic regression model. Fifth, we could not collect data on the characteristics of those who did not respond to the questionnaire. Sixth, we assumed that the impact of education at each grade was equivalent; therefore, we simply summed up the education time at each grade in this study. However, the weight of educational influence may increase at higher grades.
In addition, we could not assess the quality of the education offered, which has been identified as an important prognostic factor in prior studies [30]. Finally, we used education for “community-based medicine” as a proxy for GP education. We recognize that these categories are not identical; therefore, this study would have been better if we had generated and measured an indicator that could accurately measure undergraduate GP education in Japan.
5. Implications for Practice and Research
This preliminary study does not support an association between the quantity of compulsory education for community-based medicine in medical schools and the increased number of residents choosing a GP residency. To increase the number of residents who prefer a GP residency program, educational program directors in each medical school should not just focus on increasing the amount of time spent on education for community-based medicine but complement this effort from different perspectives, such as the distribution of education programs throughout the school curriculum or the quality of education.
Regarding future research, given the inconsistent results of previous studies and our study’s several limitations, further research is needed on the relationship between the amount of GP-related education and the subsequent increase in the number of residents choosing a GP major. Moreover, we used education time for community medicine as the study’s main exposure since we currently do not have an accurate indicator to evaluate the amount of GP education in medical schools in Japan. Therefore, future researchers need to create an accurate indicator to measure the quantity and quality of GP education in medical schools.
6. Conclusion
In conclusion, the results of this preliminary study do not support the association between the quantity of compulsory education for community-based medicine in medical schools and the increased number of residents choosing a GP residency in Japan. Educators in medical schools would do well to adopt different approaches to implement better distribution of GP-related education in the curriculum or improve its quality to increase the number of residents who choose a GP residency. Further research is necessary to reach more definitive conclusions.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
We would like to thank all the participants from the Okinawa Chubu Hospital residency program, especially Tetsuya Kikuchi MD, Miyu Yoshimi MD, Masato Nimura MD, and Yuya Higuchi MD for their assistance in data collection. We also thank the Japanese Council for Community-based Medical Education for data provision. We acknowledge the support of Editage (www.editage.com) for the English editing of this manuscript.



