Tobacco Use among School-Age Adolescents in Indonesia: Findings from the 2015 Indonesia Global School-Based Student Health Survey
Article information
Abstract
Background
Although Indonesia has a considerable proportion of adolescent smokers, nationally representative studies of its determinants remain limited. The 2015 Indonesian Global School-Based Student Health Survey (GSHS) was conducted with school-age adolescents and provided information about smoking behavior. This study aimed to examine the prevalence, determinants, and correlates of tobacco use among adolescents in Indonesia using the GSHS survey.
Methods
A secondary data analysis of a cross-sectional study was conducted using data from the 2015 Indonesian GSHS. Multivariate logistic regression was used to assess the determinants and correlates of tobacco use.
Results
Our analysis showed that 9.1% of school-age adolescents had used tobacco products in the past 30 days. Most were 13–15 years (61.7%) and had attempted to stop smoking (92.4%). After adjusting for covariates, significant risk factors associated with tobacco smoking were older age groups (prevalence odds ratio [POR], 3.01–9.40; 95% confidence interval [CI], 1.71–23.1), male (POR, 13.7; 95% CI, 8.71–21.5), psychological distress (POR, 1.41; 95% CI, 1.05–1.90), smoking exposure (POR, 1.98–2.15; 95% CI, 1.35–3.42), and when both parents smoked (POR, 2.96; 95% CI, 1.78–4.94). In addition, tobacco use was associated with other risky behaviors, including sex with multiple partners, using drugs, drinking alcohol, and being involved in physical fights.
Conclusion
Tobacco use is high among Indonesian adolescents. This prevalence highlights the need for a more stringent tobacco control policy and tailored cessation programs for adolescents by considering important modifiable determinants of tobacco use among adolescents, including risky smoking-related behaviors.
INTRODUCTION
The increasing trend seen in Indonesia of smoking tobacco is alarming. In the last 2 decades, the prevalence of smokers increased from 53.4% in 1995 to 66% in 2013 [1]. In 2018, one in every two Indonesian adult males was a smoker (55.8%), while 1.9% of Indonesian females were smokers [2]. The increasing prevalence of smoking has also been observed in adolescents. Starting with a prevalence of 7.1% in 1995, the prevalence of adolescent smokers (15–19 years old) tripled to 20.5% in 2013 [3]. These numbers are devastating given that smoking increases the risk of noncommunicable diseases such as cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes, leading to massive economic losses due to the subsequent increases in using healthcare services and productivity loss from smokers [3-5].
Approximately half of the smokers in Indonesia (52.8%) began smoking in their adolescence, and curiosity was found to be an important driver for experimentation with tobacco [2,6]. The World Health Organization (WHO)-based tobacco survey, the Global Youth Tobacco Survey (GYTS) 2014, reported that 88.2% of young smokers in Indonesia were interested in quitting smoking and 81.8% had even attempted to do so [7]. However, only 24% of young smokers receive appropriate smoking cessation services from professionals [7]. To date, a limited number of studies are available regarding the services offered to the remaining proportion (76%). Thus, it is reasonable to assume that the current smoking cessation services in Indonesia are neither accessible nor appropriate for adolescent smokers [8].
Understanding the determinants of tobacco smoking and its correlations with other risky behaviors among Indonesian adolescents is important for providing the best interventions for tobacco cessation. Previous studies in Indonesia showed that personal and behavioral determinants of tobacco smoking among adolescents are mainly influenced by the environment, including peers, family, social factors, and cigarette advertising [6,9,10]. Tobacco use is also associated with other risky behaviors such as psychological distress, current alcohol drinking, use of drugs, being bullied, early pregnancy and parenthood, and having multiple sex partners [11-15]. However, previous research was conducted using a small non-generalizable sample from certain parts of Indonesia, mostly from Java Island, which may not be applicable to the entire country; additionally, limited determinants were investigated and the association of tobacco use with other risky behaviors was not explored [6,9,10,16].
Therefore, our study aimed to examine the prevalence of tobacco use among school-age adolescents, explore the determinants of using tobacco, and investigate the correlation between tobacco use and other risky behaviors using a nationally representative survey, the 2015 Indonesia Global School-Based Student Health Survey (GSHS). This survey was designed to include issues not covered in another national survey, the National Basic Health Research (Riset Kesehatan Dasar) [1]. Understanding the profile of tobacco use among Indonesian adolescents has become an important investment, as it will support future programs by reducing the prevalence of smokers in Indonesia.
METHODS
1. Data and Sample
The first stage involved selecting both public and private schools using a probability proportional to the enrolment size approach, while the second stage involved the selection of students who were enrolled in classes randomly selected by the study team. The survey questionnaire was developed by the WHO and translated, validated, and modified as needed by the Indonesian Ministry of Health study team [1,17]. The survey response rate is 100% and 94% for the school and students response rate, respectively. After excluding data owing to missing observations of clinically relevant characteristics, our study used observations from 7,663 participants.
Informed consent was obtained from the schools, parents, and students [1]. Ethical approval for the GSHS was obtained from the ethics review boards of the Ethics Commission for Health Research and Development. The GSHS dataset can be accessed publicly on its official website (https://extranet.who.int/ncdsmicrodata/index.php/catalog/489/datafile/F2) [18].
2. Variables
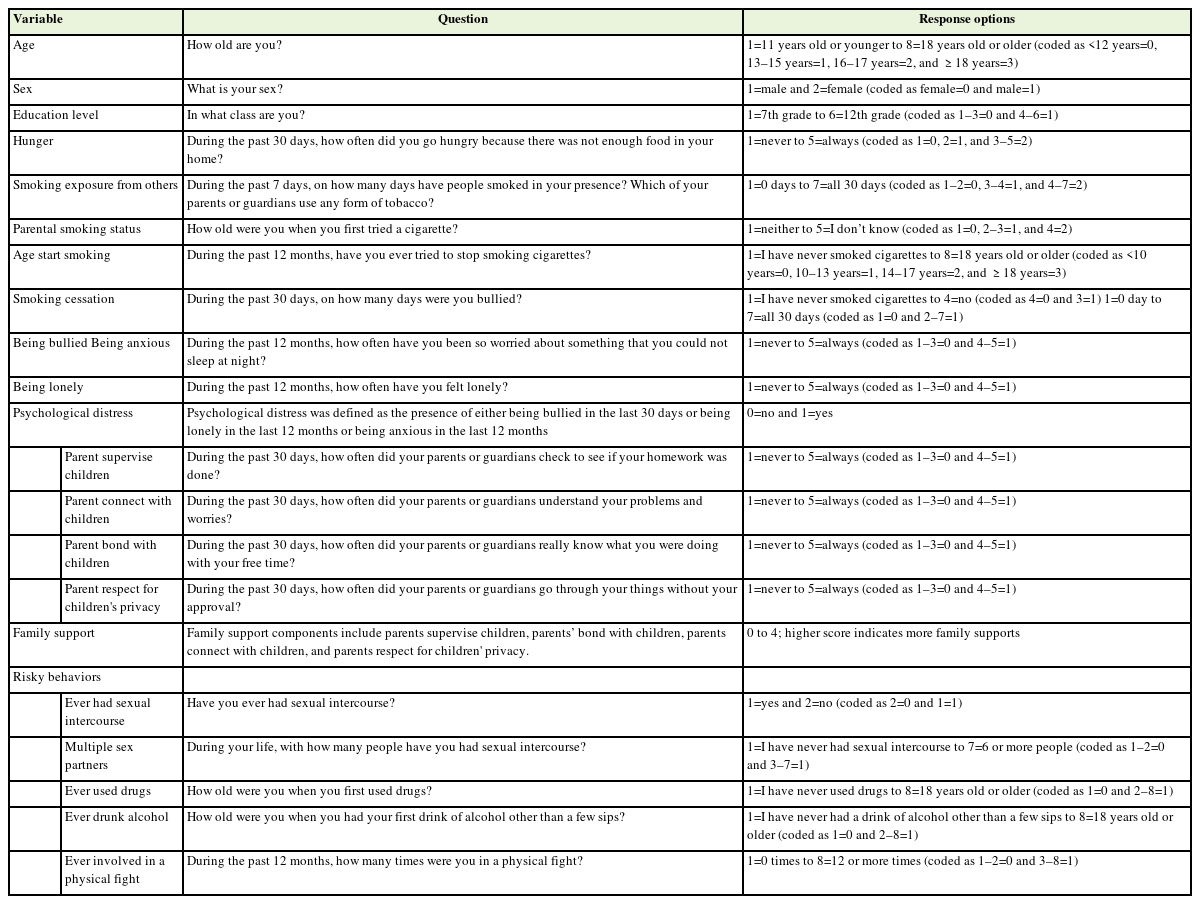
All study variables were self-reported by students and obtained from the GSHS questionnaire, as described in Table 1. Tobacco use was assessed using the question, “During the past 30 days, how many days did you smoke cigarettes?” and “During the past 30 days, how many days did you use tobacco products other than cigarettes, such as sirih, piper betel cerutu, or cigars?” The response was categorized according to previous studies using GSHS data for “current tobacco users” if students used tobacco over the previous 30 days and “never used” if students responded zero days [19,20].
3. Statistical Analysis
The analyses were conducted using STATA ver. 14.2 (Stata Corp., College Station, TX, USA). All variables are described as proportions and presented according to the students’ tobacco use status. Weighting was performed throughout the analysis to adjust for differences in the sample selection probability. A multivariate logistic regression model was used to examine determinants and correlates of tobacco use. Plausible covariates, such as age, sex, education, hunger, psychological distress, smoking exposure, parental smoking status, family support, and other risky behaviors (ever had sexual intercourse, had multiple sex partners, ever used drugs, ever drank alcohol, and involved in physical fighting), were considered potential confounders. The goodness-of-fit test using the Hosmer-Lemeshow test was conducted to test for the logistic regression model, with a P-value >0.05 indicating that the model was fit. Two-way interaction checks were performed for potential determinants, resulting in no interaction between potential determinants; thus, the no interaction term was included in the logistic regression models. Associations are presented as adjusted prevalence odds ratios (POR) and 95% confidence intervals (CIs).
RESULTS
1. Participant Characteristics
A detailed summary of the participants’ characteristics is presented in Table 2. The proportion of participants who had used tobacco in the last 30 days was 9.1%. Adolescent smokers were predominantly male (91.5%). Most participants were 13–15 years old (61.7%) and junior high school students (64.9%). Other significant characteristics showed that a large proportion of the youth smokers had inadequate food supplies in their homes (49.5%) and experienced psychological distress due to loneliness, anxiety, or bullying (34.9%). In addition, a large proportion of adolescent smokers exhibited risky behaviors, i.e., ever-had sex (8.9%), had multiple sex partners (3.2%), ever used drugs (6.8%), ever drunk alcohol (18.9%), and were involved in physical fighting (22.4%), compared to non-smokers.
2. Determinants of Tobacco Use among Indonesian Adolescents
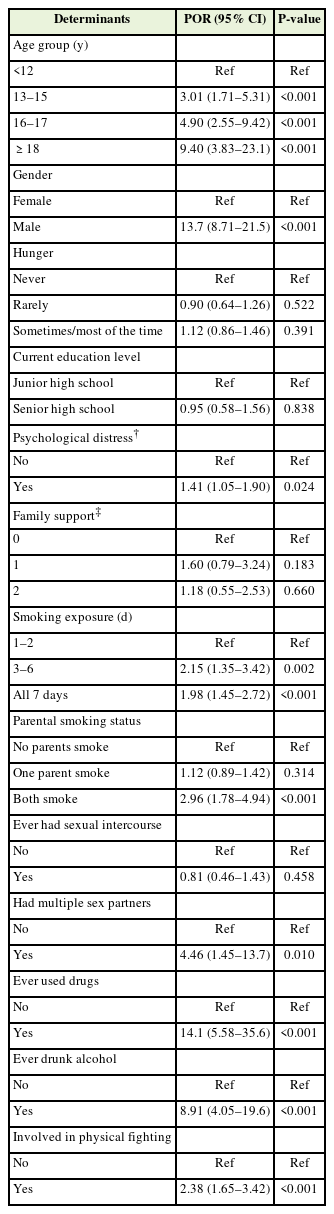
Being an adolescent smoker was positively associated with an increased age group, i.e., POR 3.01 (95% CI, 1.71–5.31; P<0.001) for age group 13–15 years old, POR 4.90 (95% CI, 2.55–9.42; P<0.001) for age group 16–17 years old, and POR 9.40 (95% CI, 3.83–23.1; P<0.001) for age group ≥18 years old, compared to those in age group <13 years old. Males were also at increased odds of being an adolescent smoker (POR, 13.7; 95% CI, 8.71–21.5; P<0.001) compared to females. Psychological distress increased tobacco use odds by 1.41-fold (95% CI, 1.05– 1.90; P=0.024) compared to those with no psychological distress. Moreover, exposure to smoking 3 to 6 days a week (POR, 2.15; 95% CI, 1.35–3.42; P=0.002) and all weeks (POR, 1.98; 95% CI, 1.45–2.72; P<0.001) increased the odds of using tobacco compared to 1 to 2 days of smoking exposure a week. When both parents smoke tobacco, the odds of tobacco use among adolescents increased by 2.96-fold (95% CI, 1.78–4.94) compared to non-smoking parents. Table 3 summarizes the determinants of tobacco use among Indonesian adolescents.
3. Correlates of Tobacco Use among Indonesian Adolescents
Our analysis found that tobacco use was associated with risky behaviors (Table 3). For instance, smoking increased the odds of having multiple sex partners by 4.46-fold (95% CI, 1.45–13.7; P=0.01). Tobacco use also increased the odds of using drugs (POR, 14.1; 95% CI, 5.58–35.6; P<0.001), drinking alcohol (POR, 8.91; 95% CI, 4.05–19.6; P<0.001), and being involved in physical fights (POR, 2.38; 95% CI, 1.65–3.42; P<0.001).
DISCUSSION
This study represented a wider adolescent population than previous studies and showed that approximately one in 10 Indonesian adolescents use tobacco. Although the proportion of adolescent smokers was relatively high, most (92.4%) had attempted to quit smoking. Several characteristics are associated with adolescent tobacco use, including older age, male sex, smoking exposure, psychological distress, and parental smoking. Our study found that tobacco use among adolescents co-occurred with other risky behaviors, such as being involved in physical fighting, having multiple sex partners, drinking alcohol, and using drugs.
The prevalence of adolescent smokers in our study was relatively lower than that reported in the National Basic Health Survey 2018 (population-based survey) and GYTS 2014 (school-based tobacco survey), which were 19.6% and 20.3%, respectively [2,7]. This might be due to the different ages of the participants, as the age characteristics in our study were wider than those of others. Our study included adolescents aged less than 12 to >18 years, while the participants in the NBHS and GYTS studies were ≥15–19 and 13–15 years old, respectively. The proportion of tobacco users in our study was also lower compared to the findings from a study conducted by Pengpid and Pletzer [21] in 2019, who reported that the proportion of tobacco users in Indonesia was 12.8%. Although the dataset was the same, the different proportions might be explained by the different approach in the statistical analysis, of which this study only used data from 7,663 participants due to the exclusion of participants if there were missing data in important variables and used weighting to report proportions. Another study comparing the prevalence of adolescent smokers using data from the GSHS of 68 low-to-middle-income countries showed that the proportion of male adolescent tobacco users in Indonesia (48.2%) exceeded the average prevalence of male adolescent tobacco users in both countries (18%) and Southeast Asia (15.3%) [19].
Consistent with previous literature, our study showed that older age and male gender were associated with the odds of using any tobacco products [6,10,22]. The role of gender is apparent worldwide, as reported by Xi et al. [19] in their study, finding that, on average, the prevalence of male adolescents who smoke (18.0%) was twice that of female adolescents (8.9%) globally. In addition, the ratio of male and female smokers was found to be higher among countries in the Southeast Asia region (around 5:1), as also witnessed in our study (around 8:1), implying that females are under social pressure to not smoke cigarettes [19,23]. The positive association between older age groups and smoking behavior in this study aligns with previous evidence conducted in the United States, arguing how a greater age group reflects greater autonomy and less parental control, hence an increase in the probability of smoking [24].
In accordance with our study, a national and school-based survey conducted in other countries, such as Brazil, showed that adolescents with psychological distress as detected by the 12-item General Health Questionnaire have higher odds of smoking tobacco for at least 7 consecutive days (OR, 2.17; 95% CI, 1.65–2.86; P<0.001), compared to nonsmokers [15]. Tobacco gained positive status among students, such as the perception that smoking “made life more comfortable,” “increased self-confidence,” and also “relieve stress.” It is also proposed that besides acting as an instrument for “self-medication”, the association between tobacco use and psychological distress can be perceived as a bidirectional relationship that influences each other [15,25].
A study in the United States that followed seventh grade students for 5 years (followed-up in 12th grade) observed that smokers are 4 times more likely to experience early pregnancy and parenthood compared to non-smokers [14]. Another study from the United States found associations between current smoking status and having multiple sex partners among teenagers aged 12 to 21 years [13]. The “clustering” pattern between using tobacco, drinking alcohol, using drugs, and physical fighting was observed in our study, which is in accordance with previous studies conducted in other countries [11,26,27]. Meanwhile, no studies in Indonesia exist that have reported similar findings. The clustering phenomenon is believed to emerge because of common etiological factors shared by these risky behaviors, which may also progress concomitantly [11].
This study was the first to use a nationally representative dataset from the 2015 Indonesian GSHS to explore the determinants and correlates of smoking among Indonesian adolescents. Furthermore, because the survey provided data on psychological distress and other risky behaviors, we included these factors as determinants and correlates of tobacco use among Indonesian adolescents. However, this study has some limitations. First, the self-reported information in the survey may cause bias in the participants, which might underestimate or overestimate the true smoking prevalence and associations of the demographic determinants found in this study. Second, as this study was based on a cross-sectional survey, it lacked temporality and is prone to reverse causation. Third, as the GSHS only has limited information on tobacco, this study was unable to explore specific information such as the students’ smoking status (occasional vs. regular smokers), geographic location (rural versus urban and school locations), and access to tobacco products.
Our findings support the notion that policymakers should ratify the World Health Organization Framework Convention on Tobacco Control (WHO-FCTC), which is the core tobacco control measure in Indonesia. Until recently, Indonesia is the only country in the Southeast Asian region that has not ratified the WHO-FCTC, which contains strategies to control the tobacco market through monitoring, smoke-free policies, cessation programs, health warnings, mass media, advertising bans, taxation and cigarette prices [8,28]. The first-decade report on the impacts of the WHO-FCTC showed that mass media campaigns and restricting adolescent access to tobacco reduced smoking initiation and prevalence, even promoting smoking cessation across countries [29]. The role of tobacco advertising is clear in promoting the likelihood of using tobacco among adolescents [30]. However, according to the WHO report, tobacco control in Indonesia still excludes the measure to ban tobacco advertising [28].
Second, as most adolescent smokers attempt to stop smoking, further research is needed to develop youth-friendly smoking cessation programs to accommodate their need to stop smoking. This program should incorporate a multifaceted approach, including parental involvement, student mental health, and a healthy lifestyle. A cessation program will be ineffective when parents who smoke are not encouraged to stop their habit, since the influence of parents is immense in modelling behavior toward their children [31]. Our study indicates that psychological distress and risky behaviors are associated with tobacco use. Thus, smoking prevention and cessation programs should be tailored to address these factors. The current review showed that brief counselling and behavioral interventions might be promising to encourage adolescents to stop using tobacco [32].
In conclusion, the prevalence of tobacco use among Indonesian adolescents is high among male students. However, most have attempted to stop tobacco use. This creates an opportunity to develop youth-friendly smoking cessation programs. In addition, we identified several determinants and risky behaviors associated with tobacco use. These findings could inform future policies on tobacco control programs for adolescents and be used to advocate for ratifying strict tobacco control as recommended by the WHO-FCTC.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
The GSHS dataset is provided online and available on https://extranet.who.int/ncdsmicrodata/index.php/catalog/489/datafile/F2. We would like to thank the Health Research and Development Agency, World Health Organization and the US Centers for Disease Control and Prevention for providing the open access data. The authors thank the study participants who participated in the GSHS survey.