Decision-Making on Contraceptive Use among Women Living with Human Immunodeficiency Virus in Malaysia: A Qualitative Inquiry
Article information
Abstract
Background
Malaysia is the first country in the Western Pacific Region to receive the validation certificate for the elimination of mother-to-child transmission of human immunodeficiency virus (HIV). The validation report recommends making sexual and reproductive health and rights of women living with HIV a priority. This article explores and assesses the sexual and reproductive health, rights, and access to healthcare services of Malaysia’s women living with HIV (WLHIV).
Methods
A qualitative secondary analysis conducted on 73 WLHIV from all over Malaysia comprised 11 in-depth interviews and 16 focus group discussions. Data were extracted from the original interview transcripts that emerged from the following questions: (1) “What are your experiences as a woman living with HIV in relation to your sexual and reproductive health and rights?” (2) “What are your experiences in accessing contraception?” (3) “What are your day-to-day experiences as a woman living with HIV?” Data were analyzed using thematic analysis.
Results
Four themes emerged from the study findings: “lack of negotiation,” “idealism in pregnancy,” “coping with restrictions,” and “past and future fears.” The four themes are grounded in religion, a patriarchal culture, meaning and expectations of motherhood, taking risks and going against medical advice to pursue fertility desires, fear of HIV transmission, and the side effects of contraceptive use.
Conclusion
The complexities involved in decision-making regarding contraceptive use revealed how WLHIV may have unresolved reproductive health needs inconsistent with healthcare providers’ focus on HIV management and prevention. Suggestions are made for improving the sexual and reproductive health and rights of WLHIV in Malaysia, which include establishing a reproductive health counseling program.
INTRODUCTION
In the 1990s, Malaysia has witnessed a gradual shift in the landscape of the human immunodeficiency virus (HIV) epidemic from originally populations of people who inject drugs toward predominantly sexual transmission now. As of December 2019, Malaysia has an estimated 15,115 women aged 15 years or older living with HIV, constituting 17% of all adults (15+ years old) living with HIV [1].
With the gradual increase in the proportion of women living with HIV (WLHIV), HIV policies demand that the sexual and reproductive health (SRH) needs of this vulnerable group be made a crucial component in the fight against eliminating HIV. Promoting and achieving optimal SRH is essential for the well-being of WLHIV, as well as their partners and children [2]. WLHIV should be allowed to make decisions regarding their reproductive and sexual life, including the rights to contraceptive use, childbearing (when and how many), and to access sexual and reproductive health services on the same grounds as all other women [3].
Nevertheless, WLHIV face unique challenges in achieving optimal SRH and exercising their rights. The choice of contraception among WLHIV is defined by the need to prevent sexual transmission of HIV as well as to prevent unwanted pregnancies and mother‐to‐child transmission of HIV [4]. Hence, contraceptive use among WLHIV is higher than that among HIV-negative women [5].
Although ensuring access to contraceptive use is an important aspect of SRH, Marlow et al. [5] reported that WLHIV were offered limited contraceptive options and, sometimes, they had no access to SRH services. Studies among sero-discordant couples also illustrated a similar finding. HIV sero-discordant couples in Kenya chose to disregard contraceptive use and attempted pregnancy despite the risk of HIV transmission [6].
This study seeks to explore factors influencing the decision of WLHIV to use contraceptive methods in relation to gender norms, religion, individual beliefs, and expectations. It aims to add new knowledge to the existing literature that is mostly focused on WLHIV living in the sub-Saharan countries. The findings are of interest to health professionals working in the fields of maternal and child health, public health, and sexually transmitted diseases.
METHODS
1. Study Design
A qualitative secondary analysis (QSA) of data obtained from our previous study is conducted [7]. The QSA method involves reusing qualitative data that were collected previously by the same or a different set of researchers in response to a different research question [8]. The process involves recontextualizing, reworking, or repurposing rich data for a new research that will extend the explanatory reach of the primary study and enhance the possibilities for building cumulative knowledge [9]. Secondary analysis of qualitative data also maximizes the effective use of data obtained from vulnerable and difficult-to-reach populations [8].
2. Overview of the Primary Study
The primary study was a qualitative assessment to evaluate sexual and reproductive health and rights, and access to healthcare services among WLHIV in Malaysia. Study participants were WLHIV from all over Malaysia, aged 18 and above, Malaysian citizens, fluent in Malay or English language, and who have availed healthcare services from the facilities established by the Ministry of Health, since January 2018. Experiences and views were also sought from key stakeholders including doctors, nurses, and counselors who were involved in providing services to WLHIV from January 2018. A total of 11 in-depth interviews and 16 focus group discussions were conducted, involving 73 WLHIV and 18 healthcare providers. All respondents were purposively sampled using the maximum variation technique to ensure diversity of respondents’ socioeconomic background. All interviews were conducted in Malay language by authors (Z.S., S.S., and N.A.A.H.), who are experienced qualitative researchers. An interview guide was developed by the research team members and piloted to ensure non-discriminating language was used with the respondents. The interviews consisted of 14 questions on the experiences of WLHIV regarding their (1) access to healthcare services (focusing on prevention of mother-to-child transmission services); (2) sexual and reproductive health and rights; and (3) stigma and discrimination in accessing healthcare services. Thematic analysis was used to analyze all interview transcripts, and the findings on the three aspects were presented in a report published by the Ministry of Health, Malaysia [7].
3. Data Collection
Since the scope of interest of this study is on decision-making regarding contraceptive use among WLHIV, data were extracted from the original interview transcripts that emerged from the following questions: (1) “What are your experiences as a woman living with HIV in relation to your sexual and reproductive health and rights?”(2) “What are your experiences in accessing contraception?” (3) “What are your day-to-day experiences as a woman living with HIV?”
4. Settings and Relevant Context
Malaysia is a Southeast Asian country with a total population of 32.7 million. The three major ethnic groups in the country are the Malays, Chinese, and Indians, with Islam being the official religion. Malaysia is the first country in the Western Pacific Region and the first Muslim country in the world to eliminate mother-to-child transmission of HIV and syphilis in 2018. An estimated 99.3% of HIV-positive pregnant women received antiretroviral therapy (ART) in 2019, which resulted in a mother-to-child transmission rate of 1.64%. Malaysian families typically have a clearly defined and deeply entrenched gender division of labor within the family. Marriage dynamics among Malaysian couples tends to be conservative and patriarchal: husbands decide on marital matters, and wives submit to their decisions.
5. Data Analysis
According to Morse [10], researchers may perform secondary analysis just as they would conduct a primary data analysis. The techniques and processes central to inductive analysis are generally applicable to a secondary interpretive process but are simpler due to the smaller dataset. All extracted transcripts were read, reread, and discussed among the research team members to ensure suitability to inform the research questions. Data were analyzed using thematic analysis [11]. The research team reviewed the transcripts and in vivo coding was performed through familiarization with the transcripts.
Transcripts and sentences were extracted using the “Find” button in the Word application using codes and keywords such as family/family planning, child*, contracept*, contraceptive methods, birth control, decision/decision making, condoms, implant, injection, natural planning, and tubal ligation. To ensure that relevant transcripts or sentences were not left out, the overall transcripts were read through multiple times. Once the researchers were satisfied that all relevant transcripts had been included and compiled, they began the process of categorizing them into subthemes and themes. The subthemes and themes were refined and further refined during the multiple discussions among the research team members. The final themes were deliberated on by the research team until they arrived at a consensus.
6. Ethical Considerations
The primary study received ethical approval from the Human Research Ethics Committee, Universiti Sains Malaysia (USM/JEPeM/21070517) and the Medical Research and Ethics Committee, Ministry of Health Malaysia (NMRR21-1583-60936 IIR). The qualitative secondary analysis does not require additional ethics approval. Informed consent was obtained from all individual participants included in the study.
RESULTS
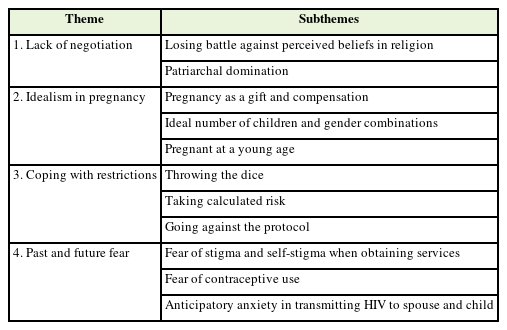
Data were sourced from the interview transcripts of 73 WLHIV who were mostly postnatal women, diagnosed before 2018, residing in the east region, between the ages of 30 and 39, of Malay ethnicity, had secondary education, were unemployed (housewives), married, and had between 1 and 2 child(ren) (Table 1).
Sociodemographic characteristics of women living with human immunodeficiency virus in Malaysia (n=73)
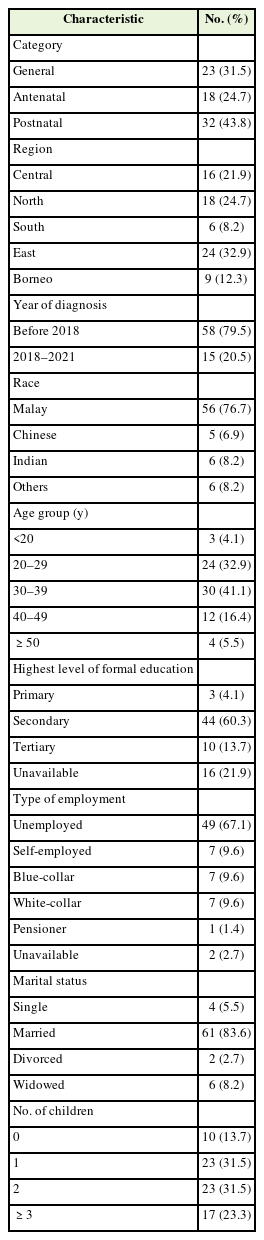
Four themes emerged during the analysis (Table 2): (1) Lack of negotiation: This refers to the struggles of WLHIV against the perceived beliefs of the religion they practiced and a dominating spouse. (2) Idealism in pregnancy: This refers to the justification they offered in refusing contraceptive use, a notion grounded in a set of meanings and expectations about pregnancy. (3) Coping with restrictions: It indicates the extent of risk taking and underlying rationalizations in contraceptive use and non-use among WLHIV. (4) Past and future fears: It refers to how feelings of stigma, worry, and anxiety shaped the decision-making in family formation and types, acceptance, and refusal of contraceptive use.
1. Theme 1: Lack of Negotiation
This theme reflects the challenges faced by WLHIV in dealing with their husbands who dominated the decision-making process leaving little room for negotiation in contraceptive use and sterilization. The majority of WLHIV spoke of their husbands’ inconsistent and outright refusal to use condoms, either as a contraceptive or as an HIV preventive measure. WLHIV reported having difficulty negotiating condom use and often lost the battle when religion was involved in the argument. Muslim religious doctrine on fate and decree (qada and qadr) was commonly misused to justify condom refusal by their partners. By believing in predestined fate, one is completely dependent on God and the natural order of life. Therefore, one tends to evade responsibility and escape the liability of making one’s own decision or exercising partial free will without any motivation to change preordained fate. Religion as a belief system may traverse across cultures, morals, and other value systems. Women too used religion to justify their decision-making, as is demonstrated in Theme 3.
My husband does not want to use a condom. He says he believes in Allah. I am worried and sometimes angry too, but he says he is confident in Him. If He wills it (husband becomes infected with HIV), so be it.
I told him “I am sick and that we must use protection.” He said, “The fate of death is in the hands of God … heck, let’s fall sick together, it does not matter.”
WLHIV narrated that their husbands initially used condoms but discontinued after a certain period. The decision to cease contraceptive use was based on the belief that their husbands had finally come to terms with fate and that having a HIV-positive wife is considered a test from the almighty God.
He used it only in the first year; in the second year, (he) stopped using it. My husband is determined, he said he does not need it. He can accept it. If he gets the disease from me, he is willing to accept it and considers it a test for him.
There was little room for negotiation due to the power imbalance. Patriarchal domination is common as women are considered subordinate to men, and their voices are powerless. WLHIV experienced a power struggle in persuading their spouses to use condoms. At times, WLHIV resorted to asking a third party to intervene and convince the spouse on condom use, but even then, they were unsuccessful in gaining their spouses’ cooperation in the matter.
My husband took it (not wearing condom) for granted … I thought I would let the doctor explain things to him. If I tell him, he would not believe it, but if the doctor tells him, maybe, just maybe, he would yield to the suggestion.
The WLHIV were constantly advocated to use protection; they made several efforts to induce their husbands to use a condom, but once vetoed by the husband, their efforts were all in vain.
The nurse scolded me and each time I visited her, she would keep reminding me to use protection. “Use protection,” she always said. She even told me to use double layer. Every month I went to the clinic, she (nurse) supplied me with condoms. At one point, my husband said there is no need to use it (condom); he was prepared to accept becoming infected it (HIV), and there was no forcing him to change his mind.
We observed that the autonomy of WLHIV in contraceptive use remained conditional; they were allowed to decide on the type of contraceptive method as long as it did not involve the man having to use a condom or undergo sterilization.
I made the decision (to wear an implant); my husband just supported me … he does not like it when the doctors discuss about the disease.
The decision to use the implant was entirely my own. He had no objection as long as I don’t tie my tubes.
From a different perspective, some WLHIV benefited from the patriarchal system. In Malaysia, although the procedure for undergoing bilateral tubal ligation (BTL) requires the mutual consent of both husbands and wives, in many instances, the husband had the final say. WLHIV spoke lovingly of their concerned husbands who made unselfish decisions in the best interest of their wives.
The doctor informed me that I may suffer from complications during the operation, so it is best to do the BTL … unless, there is no blood loss, no complication from an old wound, they would not proceed, and they would ask us first … my husband was scared on hearing this and agreed to it.
The husband’s decision was also driven by circumstances such as health concerns and other considerations such as when the wife feels overwhelmed by the burden of pregnancy.
The doctor told my husband to agree for the BTL (laughs) … my husband said he pitied me … pregnant and diabetic … he took pity on me and straight away signed the form.
2. Theme 2: Idealism in Pregnancy
The theme “idealism in pregnancy” justifies the decision to refuse contraceptive use to fulfill fertility desires. The symbolic gesture of pregnancy as an act of giving and compensating rationalizes the decision-making in family planning and contraceptive use among WLHIV. The aspect of family formation is crucial: getting married and forming a new family or remarrying and having more children to form a bigger family. Despite opposition by physicians, all WLHIV who remarried reported that they wished to conceive so that they could fulfill their new spouse’s request for a child. For these women, the need to please their new husbands and their commitment to seal the union by bearing children surpassed their concerns about the health risks of becoming pregnant.
The doctor said my health is not stable yet, so I must refrain from conceiving for the sake of my child, and I … I was pregnant a few months later; the doctor was quite angry at me … he asked why couldn’t I be patient and wait until my health is stable. I said I could not because I had just remarried, and my new husband wants a child.
Parents of singletons often worry that without siblings, their child might become lonely and have problems in sharing and making friends. Concerned WLHIV with an only child compensated for the lack of companionship by becoming pregnant to provide the existing child a new sibling.
I want another child because my child is alone and has no company/friends to play with.
I want to give my child a sibling.
The intention is stronger when they have experienced the death of a child.
I lost a child once … I cannot let my current child be the only child, it is a pity, right?
The loss of a pregnancy or the death of a child can invoke reactions that motivate fertility desires. For WLHIV who have lost children, conceiving is an act to compensate for the loss.
The doctor said that most likely I cannot conceive because I am not well … but at the same time I still want one (a child) … I was pregnant once, my first son, but he died.
Pregnancy is also regarded as a gift from God to compensate for the illness.
When I found out I was pregnant, I was happy. I considered it a gift to myself. Although I am sick, God gives me health, alhamdulillah (praise be to God).
All women with fertility intention mentioned having the ideal number of child(ren) they wished. The optimal number varied from woman to woman; among WLHIV, having two children seemed to be the most preferred choice, followed by three children. Hence the decision for contraceptive use was usually put on hold until the ideal number of children is borne.
Praise to Allah, it is okay to undergo bilateral tubal ligation, I already have two children.
Such a sentiment is reinforced when female doctors also recommend BTL following the birth of the second child.
The doctor told me to tie my tubes after I delivered my second child.
A pigeon pair mother is often celebrated by society. The ability to conceive a boy and a girl is considered the pinnacle of reproduction. This stereotyping was observed to influence WLHIV and their spouses’ decision in family planning.
I have already made plans with my husband that if we have a pair of children, then I will tie my tubes.
Until such an ideal is achieved, the women did not have the capacity to negotiate as their husbands made the final decision. This supports the lack of negotiation mentioned in the earlier theme.
I have discussed this with my husband, but if we do not get a baby girl, he refuses to let me tie my tubes.
Many WLHIV felt that the recommendations of healthcare providers to defer pregnancy until the required level of CD4 cell count was reached could delay the eventual pregnancy. Time was of the essence as they preferred to conceive during the ideal reproductive age.
The doctor said I have to wait until I am really healthy … but if I wait until I am healthy, it might be too late … I am 31 years old now.
This is further supported by another respondent; although meant as a joke, the fear of being mistaken for the grandmother of her child is enough to abandon any idea of conception once a WLHIV passes a certain age.
I said I do not have the energy to conceive, I am already old. If I send my child to school, other people might think my child is my grandchild (laughs).
3. Theme 3: Coping with Restrictions
Often, WLHIV experienced with limited options in various aspects of their lives. Feeling desperate, they coped by taking chances and making decisions based on calculated risk, religious beliefs, subjective estimations, and personal values. WLHIV and sero-discordant partners who have made peace with the illness refused to become over-anxious and projected an aura of confidence when talking about their future as all life outcomes were uncertain. Like the act of “throwing the dice,” all decisions were made based on their faith in God (Allah) as the protector and benefactor. This feeling of hope and confidence was further established when the doctor whom they respected also shared the same optimism.
The doctor said it is all left to us; if we take care of ourselves, praise to Allah. It is all God’s work. If God wished for the child to be healthy, alhamdulillah. We would not know, right? That is what the doctor told me, to just take care of myself.
Acceptance is key, as their sero-discordant spouses had come to terms or made peace with the disease.
He said it is okay, he does not mind if he gets it too; he is not worried. That is exactly what he said. So, what else can I say?
WLHIV who were older and married longer expressed confidence in non-condom use. The decision was based on self-observation and self-drawn conclusions that males were not susceptible to become infected by the disease from their HIV-positive partners. Such a notion was derived based on years of observation.
Praise be to Allah! It has been 15 years. I have seen many WLHIV who married HIV-negative men, and they remained free from HIV, no transmission. Like me, I do not use condoms. Others too. Some have had two to three children. Based on my unscientific observations, the husbands of all my HIV-positive female friends who got married are all HIV-negative, till now.
There was a tendency among WLHIV to keep scores on their husbands’ and children’s HIV-negative status. Each HIV-negative result for their husbands and newborn children reinforced their subsequent decision to discontinue contraceptive use to pursue pregnancy.
I am grateful, for when I was with my previous husband, he remained HIV-negative. My current husband is also HIV-negative. I am very thankful.
My oldest child is (HIV) negative. My second child is also (HIV) negative.
Some couples were willing to take the risk of refusing sterilization in the hope of a potential cure for the disease in the future.
In 2006, the doctor told us to do BTL, but my husband said, “No, (there was) no need for it. We do not know, there might be a cure in the future.”
derlying their decisions, WLHIV projected a conscious effort to negotiate contraceptive use by evaluating its risks, benefits, convenience, and outcomes.
I never used any kind of contraceptive. I am the scared type. If I am to take pills, I am sure to forget to take them and become pregnant. So, it is better to do without (contraceptive) it and just allow things to happen naturally; it is easier.
I prefer to allow things to take their natural course … using a condom. I had the injection after my first delivery. My body did not tolerate it well, so I had prolonged periods. Hence, I prefer to allow things to take their natural course.
Sometimes I use it, sometimes I do not … I did what the doctor taught me to do during my fertile period.
Their decision to conceive or discontinue condom use was also based on calculated risk estimated using statistics, test results, and observations they presumed were in their favor. The HIV transmission risk is considered low and even lower when WLHIV is on treatment and, as such, posed no grave danger either to the spouse or the unborn child.
The risk to my child is only 2% ... and only 0.02% if the mother is on treatment. He (husband) said it is okay to live with HIV like a normal person … the virus is in the body … it has nothing to do with other diseases. Because he has seen many HIV couples who became pregnant and could deliver babies.
I told my husband to use condoms, but since my CD4 and viral loads are under control, there is no need to use it (condom).
When queried about contraceptive non-use, some WLHIV responded that condom use was no longer required since they were not sexually active with their spouses.
We do not have sex daily or weekly, but only monthly.
Actually, my husband and I don’t have an active sexual life, not active at all.
However, these statements were unclear on whether these couples were refusing condom use because of less exposure to its benefits or they were giving up on sexual life due to condom use. Probing was not possible because this study design involved using secondary data.
WLHIV expressed indifference over the idea of seeking approval from their doctors in discontinuing contraception and becoming pregnant. Those who had unplanned pregnancies did not regret going against protocol as they believed that the doctor had no role in their family planning. All women expressed the desire to have a healthy pregnancy, but they perceived the role of the clinic as unsupportive and interfering with their lives and personal rights to become pregnant.
It is not wrong for the doctor to be telling me what is right and forcing people to use contraceptive. It is ok, I accepted it. It is our right whether to follow or ignore the (doctor’s) recommendation.
I said I do not want it (BTL). I refused because I want to use condoms. I told him (the doctor) all this while I have been successful. I am healthy now. Like a normal person. I know my body.
WLHIV felt that that they had no choice but to go against the protocol and the doctors’ orders in pursuing conception.
All four specialists forced me to use an implant. I rejected it outright. I do not even use a condom. I want a child so badly; I really want to conceive. Praise be to Allah, my child is HIV-negative.
4. Theme 4: Past and Future Fears
This theme describes the feeling of fear that shaped the decision to accept or reject contraceptive use. WLHIV spoke of feeling stigmatized when seeking treatment at health facilities. These experiences made them cautious and protective of their loved ones. They did not want to subject their children to the same painful experiences and therefore chose not to conceive.
I am afraid. Just afraid. I am afraid when I go to the clinic. People start staring, and the nurses give me weird looks; (I have) so many clinics to attend, this clinic, that clinic.
People stare at me when I take my child for her check up at the Hospital xx. I am a retroviral disease patient. When they took my blood for testing, I saw the nurse staring, whispering, and speaking behind my back. What sin has my child committed?
Fear can also evolve from self-stigma. A WLHIV spoke of feeling shy and embarrassed when obtaining free condoms at the health clinics as she felt that she was being judged by the healthcare workers.
The health clinics offered free condoms. I asked for them, and she (nurse) gave me 12 pieces. When the condoms were finished, I asked for more, but sometimes I was ashamed to ask for it. I tried to put on a brave front and asked, and the nurses gave them to me. But sometimes I felt shy, even asking for them from the older nurses, I felt shy.
The decision to use and choose the types of contraception was also influenced by WLHIV’s fear of the adverse effects of contraceptive use that stemmed from misconception and the bad experiences of others.
Implants? If our antibody is not suitable/disagrees with the implant, it will make us fat … or cause bleeding.
I do not want it … I am afraid. People say that consuming oral contraceptives can sometimes increase your chances of getting cancer or whatever.
The feeling of fear may stem from poor knowledge and the lack of clear explanation by healthcare providers, as there was an instance where a WLHIV was not aware of the types of contraceptive available.
I did not know about the oral contraceptives … if I had known I would have taken it and the doctor never told me about the pill, “just use a condom,” he said. I know only now that there are pills and other types of contraceptives.
These women also projected anticipatory anxiety in transmitting HIV to their spouses and their unborn children. Preventing virus transmission and avoiding pregnancy were the driving forces for sterilization and consistent use of contraceptives. These feelings were so strong that WLHIV were willing to make sacrifices in their lives or adjust their choice of contraceptive methods. However, subtle feelings of regret lingered over the sacrifices made.
I used a condom to avoid transmitting the virus to my husband … I waited 7 years (for pregnancy) … it is a long wait, but I was very scared to conceive.
Till date, I have not conceived. As a woman I want more children, but I am afraid. I asked the nurse at the clinic, what would happen if I become pregnant …. I realized that if I were pregnant, I would have to take my child along with me to clinic. So many clinics to attend. Sad, I feel sad for my child.
Additionally, fear of pregnancy complications prompted WLHIV to undergo sterilization.
There ps risk for me, and there is fear of bleeding. It is scary. I asked my husband, and he said, “let’s do it” (BTL).
DISCUSSION
This study describes the dynamic and complex interactions that constitute influences on WLHIV’s decision-making in contraceptive use. In general, WLHIV in Malaysia had limited ability to make decisions in sexual and reproductive matters within the household. According to Pintye et al. [12], although couples’ desires were dominant over those of individual partners in fertility decision-making, male preferences were more influential when differences between desires were observed. Generally, WLHIV were allowed to choose the type of contraceptive as long as it did not involve the male condom and BLT. It was a privilege that most WLHIV enjoyed, made possible by the lack of their spouses’ knowledge about contraception and due to the notion that contraception is a woman’s business [13]. The inequality of power in the relationships is not restricted to WLHIV. Patriarchal tradition and gender norms rooted in culture and religion are common among couples in countries such as Malaysia [14] and Indonesia [13]. However, for WLHIV, gender inequalities and power imbalances further restricted their ability to meet SRH needs and to exercise their rights [15].
Lack of negotiation was mostly cited for condom use. Islam does not forbid the use of contraceptives, but some Muslims are against family planning based on the belief that children are an adornment of life and a gift from God; thus, producing children is the purpose of marriage, and family planning contradicts the will of Allah and ability to provide [16].
Religion and spirituality were mentioned in several themes. WLHIV who were Muslims attributed their survival and acceptance of the disease and fate to their belief in qada’ and qadr. The concept of divine destiny is the fifth pillar in Islamic teaching according to which everything happens as per Allah’s will. However, the problem was rooted in the lack of understanding of this Islamic theology. Muslims are not supposed to be pessimistic and surrender to qada’ and qadr. They must work for their survival on earth and at the same time obey the sharia and be hopeful that Allah will accept their good deeds [17]. Similarly, WLHIV around the world also believe that their situation is decided by God [18]. The will of God is crucial in reproductive decision-making as “He” alone would protect their children. Based on this belief, the final decision is shared with “Him.” [18] The women felt a sense of relief because they could depend on spiritual forces and the protection of God [19].
Motherhood is a cultural norm; the phenomenon of pregnancy and the idealism relating to it was therefore culturally constructed and impacted by societal beliefs [20]. In a study of HIV-sero discordant couples in Kenya, motivations for pregnancy were influenced by the desired family size, desire for biological children, maintaining stability of the union, and conforming to sociocultural pressure [6]. A popular motive for having a child was to fulfill the husband’s desire for progeny [21]. Pregnancy was considered to promote a positive relationship between a couple, and it was the basis of marriage for starting a family. A baby is the most valuable asset in a person’s life, and giving birth is an act of continuing generations. Having multiple children was a common desire expressed by couples. A study on modern family planning method in women (not WLHIV) found that its use was directly and positively influenced by parity four or more [22]. The optimum number of children that maximizes parents’ happiness tends to differ from the perspective of parents, children, and society. In Europe, two is the preferred number [23]. The preference is to have at least one boy and one girl. Giving birth to a son is crucial for the continuation of a lineage, considering the influence of family, friends, and the husbands of these women in particular [24].
Even with the biomedical risks of ART and HIV transmission, our findings demonstrate how WLHIV were willing to take the risks prevalent on the path to motherhood. For pregnant WLHIV, pregnancy has evolved as a mediated experience of commitment and dedication. The experience of pregnancy was defined as an interplay of emotions, coping mechanism, and a sense of fulfillment [20]. For WLHIV in Kenya, pregnancy was motivated by the value of having one’s own child and the perceived significance of having children. For these women, their identity is based on their ability to carry children, and children are associated with a woman whose existence is fulfilled on bearing them [25]. WLHIV in New York provided several justifications that they believed offset the risks of pregnancy, including observing other HIV-positive women delivering healthy babies and feeling optimistic about having a healthy baby due to the prophylactic effects of zidovudine. In pursuing these motherhood dreams, consulting healthcare providers was perceived as interfering with a woman’s decision to become pregnant [25]. These women felt their physicians were not helpful and tried to discourage them from becoming pregnant because of their HIV-positive status [26]. Nevertheless, their motherhood instincts were so strong that these women were ready to break the protocol and reassured themselves that God would protect the child and being young and “healthy” would prevent transmission [21].
Decision on contraceptive used was also made based on observations and statistics on the HIV transmission rate. The rationalization that men were not susceptible to HIV (even without condom use) was reported in a study of HIV-sero-discordant couples on ART in rural Uganda who believed in the notion that the “his [man’s] blood is still strong.” Apparently, this protected their male partner from testing positive [27]. It is important to emphasize a person could become infected from having unprotected sex even once, or a person could have unprotected sex many times and not become infected, regardless of how low or high the risk per exposure is.
Fear has a significant impact on contraceptive use decisions. Concerns relating to an unintended pregnancy resulting in a HIV-positive baby and the survival of the HIV-positive mother were among the factors influencing reproductive decision-making [28]. Research evaluating the impact of HIV on family size preference in Zambia found/discovered that the risk of contracting HIV led to a decision to have fewer children. Many were also concerned about leaving orphans for others to care for, as well as the expenses associated with taking care of orphans. Contraceptive side effects are another aspect causing fear in these women. Women expressed their dissatisfaction with hormonal contraception on social media. These internet testimonies have been criticized for creating “hormonophobia” or an excessive fear of hormones based on irrational causes such as overestimation of health hazards linked with their usage, which was previously sparked by the periodic media debates over hormonal contraception. The concerns about the adverse consequences of contraception voiced by WLHIV in the current study are not unfounded. Invocation of going against the natural order, worries about future fertility, concerns about menstruation, physical side effects, altered mental health, negative effects on sexuality, fears and anxiety, and the delegitimization of hormonal contraceptive side effects were among the reasons for rejecting hormonal contraception [29].
1. Limitations of the Study
We recognize the hazards within QSA as reported by Morse [10] in 1994 in performing this study. Potential researcher bias is well understood, and the effort to reduce the bias was established by holding frequent discussions during the analysis and reporting of the findings. We are also aware of the potential to intensify and exaggerate the unique characteristics of the original data. All authors of this paper were involved in the primary study and are familiar with the transcripts. This arrangement allowed us the access to tacit understandings and nuances to articulate and reconstruct the data without violating the original meaning of the transcripts.
2. Conclusion
WLHIV’s decisions on contraceptive use either for prevention of HIV transmission or for family planning were shaped by four overriding considerations that are intertwined with each other. “Lack of negotiation,” which indicates WLHIV’s losing battle against their spouse, while “idealism regarding pregnancy” pinpoints to contraceptive use and non-use that is based on a set of meanings and expectations about pregnancy. “Coping with restrictions” highlights risk-taking behaviors and going against medical advice to fulfill fertility intention. “Past and future fears” describe how feelings of stigma, worry, and anxiety influenced family formation decisions and contraceptive usage. The narratives showed the eclecticism and flexibility that characterized WLHIV’s decision in contraceptive use and non-use, which may not be in keeping with health providers’ focus on HIV management and prevention. Although the emphasis in reproductive health is to encourage the use of contraceptives, merging HIV and reproductive care can be complex. WLHIV may have unaddressed reproductive health needs. Increased support for the reproductive health of WLHIV is needed, including supporting pregnancy desires (to choose when, how, and if, to have children). Findings from this study can be used to develop a comprehensive reproductive health counseling for WLHIV and their spouses by including elements of religion, culture, and female empowerment. Finally, we recommend health professionals to be sensitive toward the four considerations in order to be fully engaged in a shared decision-making with HIV-affected couples.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
This study has received financing and funding grant via the Joint United Nations Program on HIV/AIDS Regional Office for Asia and the Pacific (external grant no., 304 /PPSP /6150214 /T154).
Acknowledgements
We are grateful to everyone who participated in our interviews and shared their own stories. Supporters of community research aided the research team, and Dr Ye Yu Shwe (UNAIDS Regional Support Team, Asia and the Pacific) deserves special recognition for his unwavering technical assistance. In addition, we appreciate the cooperation from of the Malaysian Ministry of Health and Universiti Sains Malaysia (USM) in the provision of research facilities.