Non-Insulin-Based Indices of Insulin Resistance for Predicting Incident Albuminuria: A Nationwide Population-Based Study
Article information
Abstract
Background
Studies have shown that incident albuminuria is associated with insulin resistance (IR); however, an IR marker that best predicts the prevalence of albuminuria has not yet been established. This study explored the association between IR and incident albuminuria using various IR indices, including the homeostasis model assessment of IR (HOMA-IR), metabolic score for IR (METS-IR), and triglyceride-glucose (TyG) index, and compared their predictive abilities for the prevalence of albuminuria.
Methods
A total of 4,982 Korean adults from the 2019 Korea National Health and Nutritional Examination Survey were analyzed. The odds of albuminuria were determined using the quartiles of the IR indices. Receiver operating characteristic (ROC) curves were used to calculate the area under the ROC curve and predictability. The cutoff values for albuminuria detection were also computed.
Results
An increase in the quartiles of all three IR indices was associated with incident albuminuria, even after full adjustment for covariates (HOMA-IR: odds ratio [OR], 1.906; 95% confidence interval [CI], 1.311–2.772; P=0.006; METS-IR: OR, 2.236; 95% CI, 1.353–3.694; P=0.002; TyG index: OR, 1.757; 95% CI, 1.213–2.544; P=0.003). The area under the ROC curve for incident albuminuria based on the HOMA-IR, METS-IR, and TyG indices was 0.594 (95% CI, 0.568–0.619), 0.633 (95% CI, 0.607–0.659), and 0.631 (95% CI, 0.606–0.656), respectively. The optimal cutoff values for predicting albuminuria were 2.38, 35.38, and 8.72 for the HOMA-IR, METS-IR, and TyG indices, respectively.
Conclusion
The METS-IR and TyG indices outperformed HOMA-IR in predicting incident albuminuria.
INTRODUCTION
Chronic kidney disease (CKD) is a health problem affecting approximately 9.1% of the global population [1]. It is not only associated with impaired renal function, but also with cardiovascular disease, contributing to increased morbidity and mortality. Therefore, early detection of patients at risk for CKD is critical in preventing adverse cardiovascular events. Albuminuria is a sensitive indicator of kidney failure [2]. Furthermore, incident albuminuria is associated with a cluster of chronic diseases, including diabetes mellitus, hypertension, and dyslipidemia, which are risk factors for cardiovascular diseases [3,4].
Several studies have shown an association between incident albuminuria and insulin resistance (IR) [5,6]. They used either a hyperinsulinemic/euglycemic clamp (HEC) or the homeostasis model assessment of IR (HOMA-IR) to estimate IR. HEC is the gold standard for assessing IR; however, it is a time-consuming and invasive method that requires skilled labor and is inappropriate for large population-based epidemiological studies [7]. Instead, the HOMA-IR index, an alternative tool, can be used to evaluate IR. However, HOMA-IR is often inaccurate in estimating IR due to biological variations in glucose and insulin levels, which are included in the calculation. The score should be interpreted carefully in cases of beta-cell dysfunction [8]. Owing to the inaccuracy of HOMA-IR, non-insulin-based indices, such as the metabolic score for IR (METS-IR) [9] and the triglyceride-glucose (TyG) index [10], have been developed to assess IR. These indices not only assess beta-cell function but also the components of metabolic syndromes, such as triglyceride (TG), high-density lipoprotein cholesterol (HDL-C) levels, and body mass index (BMI).
The use of various IR indices to assess the association between IR and IR-related disorders has recently emerged. However, more research is needed to assess the relation between IR and incident albuminuria. No study has compared the predictability of various IR indices for incident albuminuria or determined the optimal cutoff values and diagnostic performance of each index for detecting albuminuria. This study aimed to show that incident albuminuria is associated with IR using the insulin-based IR index (HOMA-IR) and non-insulinbased IR indices (METS-IR and TyG index) and to further compare their predictability in detecting the presence of albuminuria.
METHODS
1. Study Population
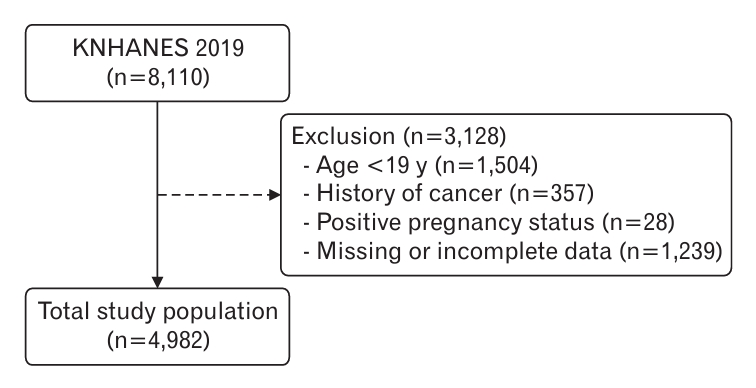
This retrospective cross-sectional study was based on data from the Korea National Health and Nutritional Examination Survey (KNHANES) conducted in 2019. The KNHANES is a nationwide survey conducted annually by the Korea Disease Control and Prevention Agency (formerly, Korea Centers for Disease Control and Prevention), consisting of three sections: health interviews, nutrition surveys, and health examination surveys. Participants were sampled from a representative population of non-institutionalized civilians in South Korea. Sampling was performed using a stratified multistage probability cluster sampling method. Once the sample was obtained, the participants were asked to complete the KNHANES. All participants provided written informed consent before enrolling in the survey. Among the selected individuals, 8,110 (74.4%) participated in the survey. Among these participants, we excluded those aged <19 years and those who met the following criteria: a history of cancer, a positive pregnancy status, or incomplete data. Ultimately, 4,982 Korean adults were included in the final analysis (Figure 1). This study adhered to the ethical principles of the Declaration of Helsinki and was approved by the Institutional Review Board of the Yonsei University College of Medicine, Seoul, Korea (IRB approval no., 4-2022-0817).
2. Data Collection
A survey was used to collect sociodemographic information, including education level and household income. Health-related questionnaires were used to gather data on physical activity status, aerobic exercise, smoking, alcohol consumption, and past medical history. Current smokers were defined as those who had smoked more than 100 cigarettes in their lifetime. Alcohol consumption was defined as the intake of more than one drink per month. Individuals engaging in aerobic exercises were defined as those performing moderate-intensity activity for 2 hours and 30 minutes per week or a combination of moderate-and high-intensity activity for 1 hour and 15 minutes per week. Restricted physical activity was defined as a limitation in daily activity due to any type of health or psychological problem.
Body weight (kg), height (m), and blood pressure (mm Hg) were measured using standard protocols. BMI was calculated as weight divided by height squared (kg/m2), and participants with a BMI >25 kg/m2 were considered obese [11]. Mean systolic blood pressure and diastolic blood pressures were measured.
After fasting for 8 hours, serum levels of glucose, insulin, total cholesterol, TG, HDL-C, blood urea nitrogen, and creatinine were assessed. Estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease formula: First-void urine samples were collected early in the morning to determine urine albumin and creatinine levels.
3. Definitions of Incident Albuminuria and IR Indices
Incident albuminuria was defined as a urine albumin-to-creatinine ratio of 30 mg/g. We used the following three indices to measure IR: HOMA-IR, METS-IR, and TyG index. The HOMA-IR was calculated using the following formula: insulin (U/mL)×glucose (mg/dL)/405. The METS-IR was calculated using the following formula: ln[2×glucose (mg/dL)+TG (mg/dL)×BMI (kg/m2)]/ln[HDL-C (mg/dL)]. The TyG index was calculated using the following formula: ln[TG (mg/dL)×glucose (mg/dL)/2].
4. Statistical Analyses
Continuous variables were expressed as means and standard errors, and categorical variables were expressed as numbers and percentages (%). The quartiles of each IR index are represented as Q1, Q2, Q3, and Q4 (Q1 is the lowest and Q4 is the highest; detailed values are presented in Supplement 1). Multiple logistic regression was used to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) of each IR index quartile for incident albuminuria in the three models. Model 1 was adjusted for sex and age; model 2 was adjusted for factors in model 1 plus socioeconomic factors, such as household income, educational level, aerobic exercise, restricted activity, smoking status, and alcohol consumption; and model 3 was adjusted for factors in model 2 plus diseases, such as hypertension, diabetes mellitus, cardiovascular disease, CKD, and obesity. We examined receiver operating characteristic (ROC) curves to compare the predictability of IR indices for incident albuminuria using the area under the ROC curve (AUC) at baseline. The AUC for the METS-IR, TyG index, and HOMA-IR were compared using the Delong method. Youden’s index was used to calculate the optimal cutoff points of each IR index for predicting albuminuria. Statistical analyses were performed using IBM SPSS ver. 26.0 (IBM Corp., Armonk, NY, USA) and SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA). Statistical significance was set at P<0.05 for this study.
RESULTS
1. Participant Characteristics
The clinical characteristics of the participants were summarized according to the presence or absence of incident albuminuria (Table 1). Participants with albuminuria were not only more obese, with higher mean BMI, systolic blood pressure, and diastolic blood pressures values, but also had more restricted physical activity. Individuals in the albuminuria group performed less aerobic exercise and were more likely to have chronic diseases (such as hypertension, diabetes mellitus, cardiovascular diseases, and CKD) than those without albuminuria. The mean glycated hemoglobin, fasting plasma glucose, and serum insulin levels, excluding eGFR levels, were higher in the albuminuria group than in the non-albuminuria group. Participants with incident albuminuria had higher mean HOMA-IR, METS-IR, and TyG index scores than those without albuminuria.
2. Incident Albuminuria and Quartiles of IR Indices
The ORs for incident albuminuria increased as the quartiles of the IR indices increased. The ORs in the highest quartile (Q4) of all three IR indices were statistically significant (P<0.05) even after adjusting for covariates. In model 3, the ORs (95% CI) for METS-IR Q4, TyG index Q4, and HOMA-IR Q4 were 2.236 (1.353–3.695), 1.757 (1.213–2.544), and 1.906 (1.322–2.772), respectively (Table 2).
3. Comparison of the Predictability of IR Indices for Incident Albuminuria
We investigated the ability of each IR index to predict the incidence of albuminuria (Table 3). The AUCs (95% CI) of the non-insulin-based IR indices, METS-IR and TyG index, were 0.633 (0.607–0.659) and 0.631 (0.606–0.656), respectively, while that of the insulin-based IR index, HOMA-IR, was 0.594 (95% CI, 0.568–0.619). All AUC values of the three indices performed significantly better than chance (overall P<0.001). The comparison between HOMA-IR and both non-insulin-based IR indices showed significant differences (METS-IR and HOMA-IR, P=0.002; TyG index and HOMA-IR, P=0.004). Overall, both the METS-IR and TyG indices showed higher predictability than the HOMA-IR for incident albuminuria (Table 3, Figure 2).
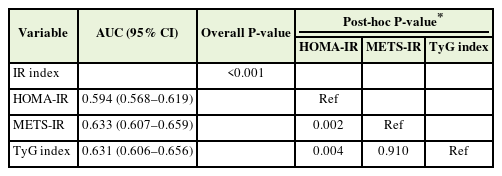
Comparison of the area under the ROC curves of the three IR indices for predicting incident albuminuria
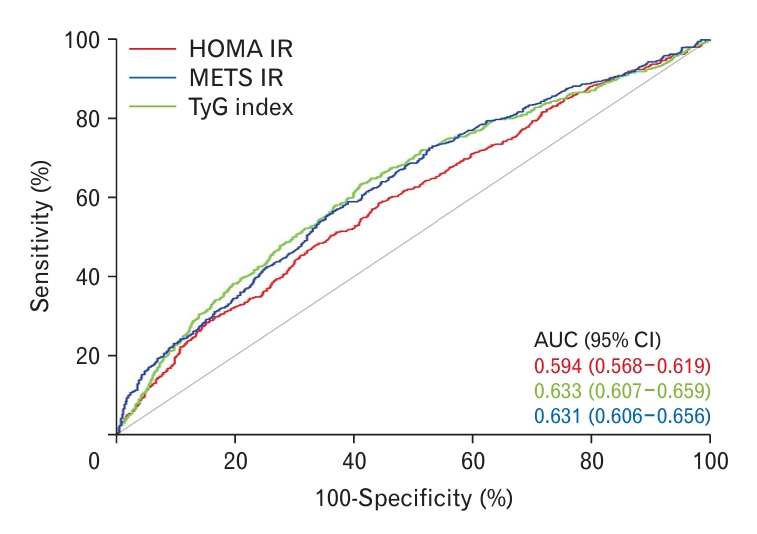
Predictability of the three insulin resistance indices for incident albuminuria. The diagonal line represents the reference area under the curve of 0.50, indicating chance performance; A curve above 0.50 signifies performance better than chance. AUC, area under the receiver operating characteristic curve; CI, confidence interval; HOMA-IR, homeostasis model assessment of insulin resistance; METS-IR, metabolic score for insulin resistance; TyG, triglyceride-glucose.
4. Cutoff Value and Diagnostic Performances for Predicting Incident Albuminuria
The optimal cutoff points of HOMA-IR, METS-IR, and TyG indices for suspected incident albuminuria were 2.38, 35.38, and 8.72, respectively (Figure 3). For each optimal cutoff point, the sensitivity/specificity were 0.47/0.68, 0.64/0.56, and 0.57/0.64 for HOMA-IR, METS-IR, and TyG index, respectively (Figure 3).

Receiver operating characteristic (ROC) curve for each insulin resistance index depicting cutoff values and diagnostic performance in predicting incident albuminuria. Cutoff points (sensitivity, specificity) of the homeostasis model assessment of insulin resistance (HOMA-IR) (A), metabolic score for insulin resistance (METS-IR) (B), and triglyceride-glucose (TyG) index (C).
DISCUSSION
It is well known that albuminuria, independent of a deranged eGFR, is not only a manifestation of early CKD but also a factor in all-cause cardiovascular mortality [12]. In this study, we found that both insulin-based (HOMA-IR) and non-insulin-based IR indices (METS-IR and TyG indices) were associated with incident albuminuria among Korean adults. Additionally, the METS-IR and TyG indices showed higher predictability than the HOMA-IR index. Our results suggest that noninsulin-based IR indices are more closely associated with incident albuminuria than HOMA-IR. To the best of our knowledge, this is the first study to compare the predictability of HOMA-IR, TyG index, and METS-IR for incident albuminuria and to determine the optimal cutoff values and diagnostic performance of each index for detecting albuminuria.
The underlying mechanism of reduced insulin sensitivity resulting in albuminuria is mainly explained by endothelial dysfunction [13]. Insulin is involved in regulating the stimulation of nitric oxide production from the endothelium [5], and impaired endothelial function in glomeruli can lead to albuminuria [14]. From a molecular standpoint, IR can lead to endothelial dysfunction via impaired phosphatidylinositol 3-kinase-dependent signaling, necessary for nitric oxide production and endothelin-1 secretion for vasodilation 6. An in vivo study in mice suggested that IR increased podocyte death, potentially contributing to early diabetic nephropathy [15]. The RISC (Relationship between Insulin Sensitivity and Cardiovascular Disease) study, a 3-year longitudinal cohort study, showed that healthy adults with reduced insulin sensitivity had an increased prevalence of incident albuminuria (B-coefficient=-0.14, P=0.001) [13]. In addition, insulin sensitizers, such as thiazolidinediones, help reduce albuminuria, supporting the idea that improving insulin sensitivity may also decrease albuminuria [5].
While the HEC is a direct tool for assessing IR, its invasiveness and laborious nature have led many investigators to use other surrogate markers of IR. Studies have assessed the association between IR and incident albuminuria using the HOMA-IR [6,16]. The calculation of HOMA-IR includes glucose and insulin values, which are the metabolic markers mostly used in patients with diabetes. Therefore, studies utilizing HOMA-IR might be skewed by a population with diabetes and might not adequately consider other risk factors, such as dyslipidemia and obesity. Abnormal lipid levels are well-known risk factors for cardiovascular disease and CKD progression [17]. High TG or low HDL-C levels have consistently been associated with decreased renal function in studies [18,19]. Obesity is associated with albuminuria due to changes in adipocyte metabolism, which produces hormones that directly or indirectly affect the kidneys [20]. Therefore, non-insulin-based IR markers (METS-IR and TyG index), whose calculations include the values of cardiovascular risk factors, such as TG, HDL-C, or BMI, are better predictors of albuminuria and renal dysfunction.
Several studies have used the TyG index to predict chronic diseases and have shown its superiority over HOMA-IR. A 9-year longitudinal retrospective cohort study conducted in Korea demonstrated that the TyG index predicted the incidence of type 2 diabetes better than the HOMA-IR index, showing significant differences (AUCs of the TyG index and HOMA-IR were 0.784 and 0.728, respectively; P<0.001) [21]. Another Korean cohort study exhibited that the TyG index was superior to the HOMA-IR index in predicting metabolic syndrome (AUCs of TyG index and HOMA-IR were 0.837 and 0.680, respectively; P<0.001) [22]. A cross-sectional study reported a stronger association between the TyG index and arterial stiffness compared to that of the HOMA-IR [23]. METS-IR is another novel surrogate marker of IR, and emerging studies have demonstrated its potential association with several chronic diseases. Its calculation includes the values of BMI, HDL-C, TG, and fasting plasma glucose, requiring more detailed information than the TyG index. In a population-based cohort study with nonobese Japanese adults, a higher METS-IR score was associated with an increased risk of type 2 diabetes mellitus (hazard ratio, 1.17; 95% CI, 1.09–1.27; P<0.001) [24]. Another study in a normal-weight Chinese population revealed a similar relation between METS-IR and hypertension (OR, 2.884; 95% CI, 1.2468–3.369; P<0.001) [25]. A longitudinal study in Koreans without diabetes reported that METS-IR was a good predictor of ischemic heart disease (AUC, 0.620; P<0.001) [26]. However, only a few studies have compared the METS-IR and HOMA-IR.
A recent study by Gao et al. [27] reported that a high TyG index indicates a greater risk of incident albuminuria and suggested that it is a better predictive marker of early-stage CKD than HOMA-IR. A large population-based study by Wang et al. [28] showed that METS-IR was associated with a mildly reduced eGFR. Another cross-sectional study conducted by Su et al. [29] reported its association with an elevated urine albumin-to-creatinine ratio. Consistent with other studies, we demonstrated that both non-insulin-based IR markers, METS-IR and TyG index, are associated with incident albuminuria and have better predictability for incident albuminuria than HOMA-IR. However, this study has several limitations. First, because the AUC of the indices discussed in this study do not exhibit high predictability, their clinical use in real-world settings can be challenging. Second, the study population included only Koreans; therefore, it is difficult to apply the results to people of other ethnicities. Third, we could not determine definite causality between IR and albuminuria owing to the cross-sectional nature of this study design. Future research is needed to investigate an IR index that can better predict early-stage renal failure. Finally, since information on socioeconomic status and medical history as confounders is based on self-surveys, the data can be inaccurate and biased. Despite these limitations, the strength of this study was that it was a large national survey that included the general population of Korean adults.
In conclusion, all the IR indices were associated with the prevalence of incident albuminuria. Furthermore, non-insulin-based IR indices (METS-IR and TyG) displayed higher predictability of incident albuminuria than the insulin-based IR index (HOMA-IR) among Korean adults. This conclusion supports the notion that simple and cost-effective IR indices are more closely associated with incident albuminuria than traditional insulin-based IR indices. Prospective research with longitudinal data and other ethnic groups would help verify the association between IR and incident albuminuria.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
This research was supported by the Technology Innovation Program, A Platform for Prediction and Management of Health Risk Based on Personal Big Data and Life-logging, funded by the Ministry of Trade, Industry & Energy (grant no., 200002781) and the Korea Institute of Planning and Evaluation for Technology in Food, Agriculture and Forestry through the High Value-Added Food Technology Development Program, funded by the Ministry of Agriculture, Food and Rural Affairs (grant no., 321030051HD030).
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4082/kjfm.23.0138.
Quartiles of insulin resistance indices