Trends in Cervical Cancer Mortality by Socioeconomic Status in Korean Women between 1998 and 2009
Article information
Abstract
Background
Death from uterine cervical cancer could be preventable by an active participation of women at risk in a screening program such as the Papanicolaou test. In order to examine the presence of socioeconomic disparity in preventable deaths, we evaluated the time trends of cervical cancer mortality by socioeconomic status in Korean women.
Methods
We selected level of educational attainment and marital status as surrogate indices of socioeconomic status. Using death certificate data and Korean Population and Housing Census data from Korea National Statistical office, we calculated age-standardized yearly mortality rates from cervical cancer between 1998 and 2009 according to the level of education as well as marital status.
Results
Cervical cancer mortality peaked in 2003 and then decreased gradually over time. Cervical cancer mortality was the highest in the group with the lowest level of educational attainment in all age groups and the gap between the lowest and the highest educational level has increased over time. Cervical cancer mortality was lower in married women than unmarried women in all age groups, and the degree of difference did not change over time.
Conclusion
In the Korean population, socioeconomic differential in cervical cancer mortality has persisted over time.
INTRODUCTION
Uterine cervical cancer has long been the leading cause of cancer death in women worldwide. Fortunately, development of the Papanicolaou test allowed early detection of cervical cancer at a treatable stage and has been recognized as one of the most effective cancer screening tools.1) Thus, introduction of cancer screening programs using the Papanicolaou test into populations at risk has been expected to reduce cervical cancer mortality dramatically.
In Korea, population-based cervical cancer screening has been offered free to Medical Aid Program recipients since 1999 and the target population of the screening program has gradually expanded to the beneficiaries of National Health Insurance (NHI): to those with income levels of lower 20% in 2002, to those with income levels of lower 30% in 2003, and to those with income levels of lower 50% in 2005. Finally, in 2011, the NHI corporation also started the National Cancer Screening Program (NCSP) by which NHI beneficiaries in upper 50% of income levels could also benefit and, currently, all Korean women aged 30 or older are able to receive cervical cancer screening test biennially.2)
However, despite the active introduction of the nationwide cervical cancer screening program,3) cervical cancer is still the sixth most common cancer in Korean women.4) Therefore, it seems uncertain whether the NCSP has effectively contributed to reducing the disease burden from cervical cancer in Korean women.
In order to maximize the effect of a preventive screening program, improvement in the participation rate of the target population at risk seems essential. Several studies were conducted to evaluate factors related to the participation rate of a screening program and they suggested socioeconomic factors such as income,5) level of educational attainment,3,6) marital status,7) and the area of residence3) as major determinants.
Low socioeconomic status (SES) has long been suggested to be associated with a higher risk of cervical cancer8-10) and the introduction of the free screening program is expected to lower the risk of cervical cancer death among women with low SES very effectively. However, it is also uncertain if the NCSP has effectively contributed to reducing cervical cancer mortality in women with low SES.
In this regard, we examined the trends of cervical cancer mortality since the introduction of the population-based cervical cancer screening program for Korean women in 1999 by the level of educational attainment and marital status, i.e., markers of SES. Examining the magnitude of socioeconomic differentials in cervical cancer mortality may provide clues to more effective population-based strategies against cervical cancer.
METHODS
We selected educational level and marital status as markers of SES for this study because data on other SES markers such as income or area of residence were not available. We derived death certificate data on Korean women aged 25 or older between 1998 and 2009 from the Korea National Statistical Office, which included age at death, educational level, marital status, and specific cause of death (http://mdss.kostat.go.kr/mdssext/). Then, we identified deaths from cervical cancer that have occurred each year using codes of International Classification of Disease-10 (C530-C539).
We counted the number of whole Korean women aged 25 or older by educational level and by marital status based on the Korean Population and Housing Census data. The Korean Population and Housing Census is an obligatory process inquiring into all Koreans and foreigners residing in the Republic of Korea in compliance with the Statistics Act and it has been conducted every 5 years since 1925.11)
We categorized the yearly data of cervical cancer death into 24 groups with consideration of both age groups (six groups by 10-year interval) and the highest level of educational attainment (elementary school or less: ≤6 years, middle school: 7-9 years, high school: 10-12 years, and college or higher: more than 12 years). We also categorized census data into the same 24 groups with consideration of both age groups and educational levels. Then, we calculated the crude rate of death from cervical cancer in each group. For this calculation, census data from 2000 was used as the denominator for mortality between 1998 and 2002, data from 2005 for mortality between 2003 and 2007, and data from 2010 for mortality between 2008 and 2009.
In order to calculate the crude death rate from cervical cancer in each age and marital status group, we repeated the above calculation process with 12 groups categorized with consideration of six age groups and two marital status groups (married and unmarried). The unmarried marital status group included widows and those women who were never-married or were divorced from their husbands and who were combined into one group because of the relatively small number of each group compared to married women.
Finally, we calculated the age-standardized mortality rate of cervical cancer for each educational level as well as for each marital status using the mean of Korean population numbers from 2000, 2005, and 2010 as a reference group. All the analyses were performed using SAS ver. 9.3 (SAS Institute Inc., Cary, NC, USA). The data used in this study do not include any identifiable personal information. Thus, the institutional review board of the Samsung Medical Center exempted acquisition of informed consent form for the current study.
RESULTS
The educational level increased in Korean women during the study period. The proportion of women educated more than 12 years has increased and that of less educated women has increased, but such trends are unclear among those who have died from cervical cancer. The proportion of married women has decreased both in the general population and cervical cancer dead (Table 1).
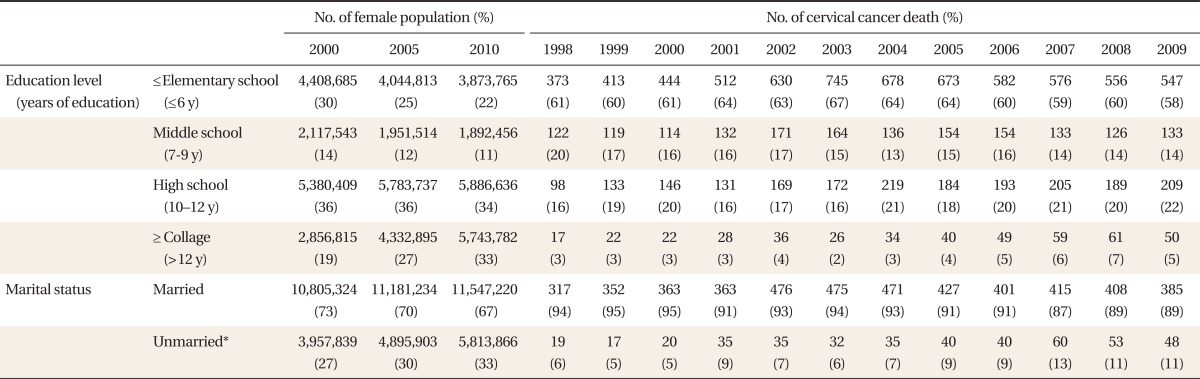
Distribution of educational level and marital status among general Korean female population (2000, 2005, and 2010) and women who died from cercal cancer (between 1998 and 2009)
Table 2 shows the time trend of the mortality rate of cervical cancer between 1998 and 2009 by 10-year age. Crude mortality rate increased until 2002 or 2003 and then, it started to decrease in almost all age groups. The time trend of the age-standardized mortality rate did not differ from that of the crude mortality rate.
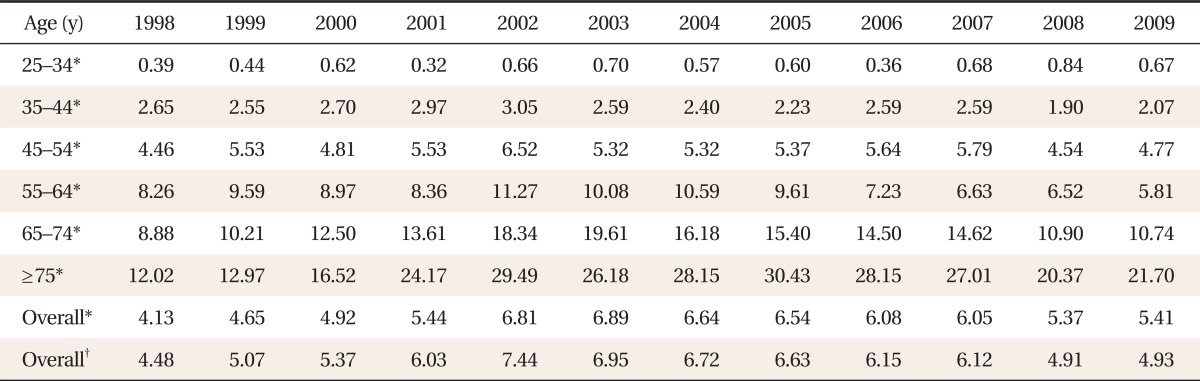
Mortality rates (per 100,000 persons) from cervical cancer in Korean women by 10-year age group between 1998 and 2009
Table 3 shows the change in the age-standardized mortality rate of cervical cancer between 1998 and 2009 by the educational level in Korean women aged 25 years and over. Over the twelve years, the mortality from cervical cancer was highest among the lowest education level group and lowest among the highest education level group. When we compared the mortality in 2009 with the mortality in 1998, the cervical cancer mortality rate decreased only in the highest education level group, while it increased in other groups. The lowest education level group showed a 57% higher mortality rate in 2009 compared to 1998.
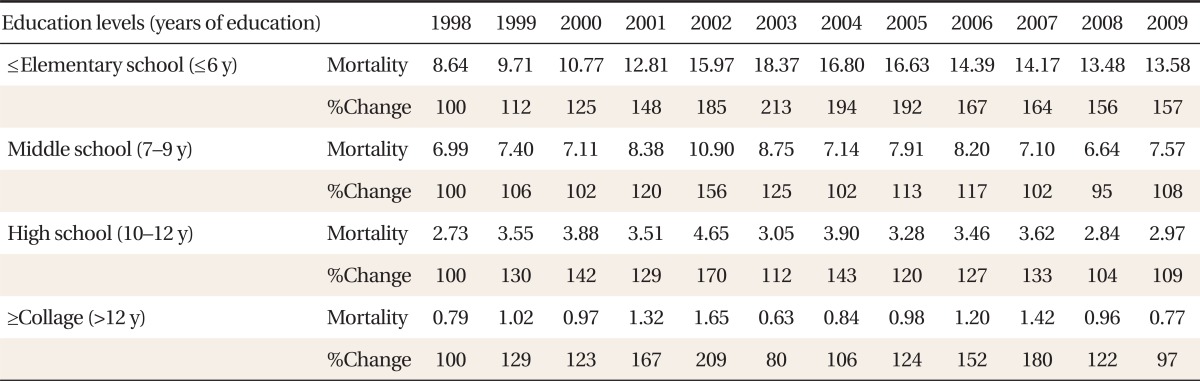
Age standardized mortality rate (per 100,000 persons) from cervical cancer by educational levels in Korean women aged 25 years and over between 1998 and 2009
We examined if the time trend and socioeconomic differentials of cervical cancer mortality differed by age group (Figure 1). In women aged less than 55 years, cervical cancer mortality increased over time in all education level groups. In women aged 55 years or older, cervical cancer mortality decreased over time in the three higher education level groups and increased in the lowest education level group. The gap in mortality rate between the lowest and the highest education level groups increased over time regardless of the age group.
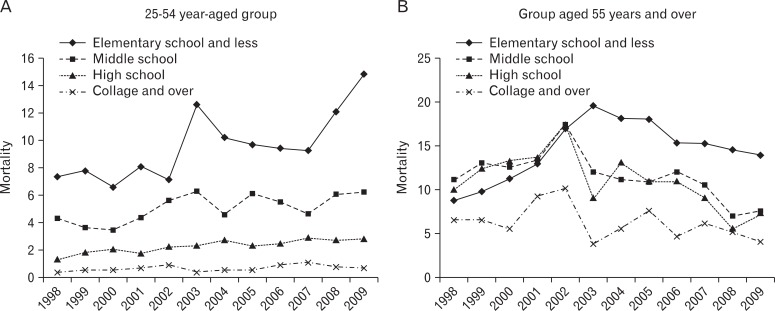
(A, B) Time trend in mortality rate (per 100,000 persons) from cervical cancer according to educational levels in Korean women in each age group (25-54 y, ≥55 y) between 1998 and 2009.
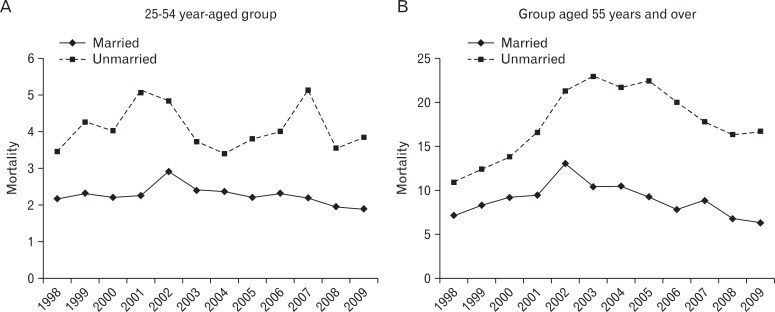
As shown in Table 4, the mortality of cervical cancer in all marital status groups reached a peak in 2002 and showed a more marked decreasing trend in the group of married women. In the mortality by marital status and age group, mortality was higher in unmarried women compared with married women in all age groups, and the difference in mortality rate between these groups did not change over time (Figure 2).

Age standardized mortality rate of cervical cancer by marital status in Korean women aged 25-74 years between 1998 and 2009
DISCUSSION
In this study of Korean women, we found that socioeconomic differential in cervical cancer mortality exists across women with different levels of educational attainment and marital status. This finding is consistent with the findings from earlier studies. Patel et al.12) showed that five-year survival from cervical cancer was higher for married women than women with other marital status. Simard et al.9) reported that cervical cancer mortality was higher in less educated women (<12 years) compared with more educated women (>16 years) and this disparity in cervical cancer mortality increased between the periods 1993 to 1995 and 2005 to 2007. Several explanations exist for this finding. Firstly, greater exposure to risk factors for cervical cancer in the low socioeconomic group than in the higher SES group; secondly, the lower participation rate of the low socioeconomic group in the cervical cancer screening program. Previous studies have shown that the participation rate in cervical cancer screening was low in women with low education levels13,14) or unmarried women.14,15) Thirdly, the lower socioeconomic groups' lower accessibility to the medical care system.16) However, we could not examine these hypotheses in the current study. Therefore, further studies are necessary to obtain evidence to support or negate these hypotheses.
In Korea, the population-based cervical cancer screening program was initiated for the benefit of lower socioeconomic groups since 1999. Accordingly, the incidence of cervical cancer could be expected to decrease dramatically by the introduction of the Papanicolaou test especially among more deprived people. However, our study shows that cervical cancer mortality did not significantly between 1999 and 2009, and socioeconomic differentials between the lower education level group and the higher education level groups have rather increased over time during the last decade in Korean women. Given that it takes 5.5 to 21 years for precancerous lesions to progress into invasive cancer,17) the effect of NCSP in preventing cervical cancer mortality would become more distinct 10 or 20 years later.
The mortality of cervical cancer was lower in married women compared with unmarried women. This finding is consistent with the findings from other studies.12,18) As for the reasons for this finding, effect of social network19) and high participation rate of screening in married women have been suggested.20) In addition, few studies reported low educational level in unmarried women compared with married women.21,22)
Interestingly, we observed an increasing tendency of cervical cancer mortality in women of 25 to 34 years old, which is consistent with the findings from other studies23) and probably reflects the decline in age at first sexual contact in Korea.24,25) Thus, the range of NCSP recipients needs to be extended to all women who have experienced sexual contact regardless of age as most guidelines for cervical cancer screening indicate.26,27)
In addition, a steeper increase in cervical cancer mortality in women of 25 to 34 years was found for women in the lowest educational group (≤elementary school) than in women of the older age group. Given the marked improvement in educational level in Korean women during recent years, the lowest educational level in young women may reflect more deprived SES than in the same educational level in old women and, thus, may indicate a greater risk of cervical cancer mortality. However, we could not examine this issue in the current study and further studies are necessary.
The current study has some limitations. Firstly, for calculating mortality rate, we inevitably used census data from a 5-year interval instead of annual data because the Korean Population and Housing Census has been conducted every 5 years and it is the only survey which provides information on the number of persons by education level and marital status. Secondly, our study showed that cervical cancer mortality had increased until 2003 in all age groups. This is an unexpected finding given that cervical cancer mortality has decreased worldwide during the last several decades.28) Shin et al.29) who examined cervical cancer mortality in Korean women aged 30 to 69 years from 1993 to 2002 reported findings that may explain the reason for the unexpected increase in cervical cancer mortality between 1998 and 2003. In the study, the increasing tendency of cervical cancer mortality over time turned into a decreasing tendency after the correction of the cause of death which was misclassified as 'uterine cancer of unspecified.' Given that the data source of our study was the same as that of the study by Shin et al.,29) the unexpected findings regarding the trend of increasing cervical cancer mortality until 2003 have been accrued by the misclassification of the cause of death. However, it is less likely that the misclassification has caused significant bias in our study because the time trend of cervical cancer mortality did not materially differ across different education levels and marital status groups. Thirdly, we could not verify the accuracy of data on educational levels and marital status of the deceased.
In conclusion, this study shows that cervical cancer mortality increases with decreasing SES, and the socioeconomic differentials in cervical cancer mortality relative to education level and marital status have been increasing over time in Korean women even after the introduction of the nationwide cancer screening program.
ACKNOWLEDGMENTS
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea, and funded by the Ministry of Education, Science and Technology (2011-0013545 and 2010-0029113).
Notes
No potential conflict of interest relevant to this article was reported.