|
 |
- Search
| Korean J Fam Med > Volume 32(7); 2011 > Article |
Abstract
Background
The family medicine residency program consists mainly of clinical rotations in other specialties and the family medicine-specific training. We conducted this study to investigate how family medicine residents evaluated their training program that include family-oriented medicine, clinical preventive medicine, behavioral science and research in primary care.
Methods
In 2009, third-year residents of 129 training hospitals in Korea were surveyed to investigate the current state and their expectation of the residency program. The contents of questionnaires included training periods, conferences, procedures, interview techniques, outpatient and inpatient consultations, and written thesis.
Results
Total 133 out of 142 residents (93.7%) responded that 3 years of training is ideal or pertinent. Residents responded that the types of conference that they need most are journal review (81%), staff lecture (73.2%), and clinical topic review (73.2%), in that order. Procedures and interview techniques that the residents want to learn most were gastroscopy (72.5%), abdominal ultrasonography (65.2%), and pain management (46.4%). Hospitals where family medicine residents do not see hospitalized patients or patients in the outpatient clinic were 7.9% and 6.5%, respectively, whereas hospitals that maintain continuous family medicine outpatient clinics were only 40.8%. Education in outpatient clinic and articlewriting seminars was done less frequently in the secondary hospitals than in the tertiary hospitals.
As the term 'specialist of breadth'1) implies, family medicine attaches greater importance to breadth than to depth in medical care.2) Unlike other residency programs, rotating training in various medical specialties is the major part of the family medicine residency training. However, family medicine-specific training is considered more important than rotation in specialties. Role of family physicians should not be limited to gate-keeping. The family physicians' role has expanded from the existing disease-oriented paradigm to the patients, family, and community-oriented paradigm, and the range of medical care of family medicine included counseling of health risk factors such as drinking, smoking, and obesity. The idea of an early health checkup was also established by family physicians, and many family physicians actively take part in clinical preventive medicine. They produced many research articles related to the subject of primary care. The very specialties of family physicians can not be obtained through specialty rotations, but is determined by the quality of family medicine specific training.
Recently, there has been much discussion in the Korean Academy of Medical Science that the 2 years of rotating internship should be considered to raise general practitioners rather than 3 years of family medicine training to raise family physicians. There was also reconsideration in the US about whether 3 years of family medicine training is sufficient enough. According to a survey targeting specialists and medical students overseas, the interest in and support for family medicine in the US is gradually decreasing.3) Regardless, family medicine is still a popular major in Korea, but to maintain this popularity, the family medicine residents' claims should be heard to improve the quality of the training program.
There have been limited researches on the evaluation of residents' rotating training in specialties and the analysis of training program.4,5) Some research was related to family medicine professors' viewpoint about the range of residents' training experiences, curriculum of family medicine residency, and learning objectives.6,7) However, there has been no research to date on the current state of family medicine-specific training from the viewpoint of the resident physicians.
The purpose of this study is to investigate the 3rd year residents' view on the present state of the family medicine-specific training program and their expectation of that program, who are likely to provide most practical evaluation of this country's family medicine training program.
The subjects of this study were 3rd year residents in family medicine training hospitals in Korea. Survey questionnaires were sent to 349 residents at 129 hospitals by e-mails and post mails. Hospitals that share a same training program were counted as one hospital. For example, The Catholic University of Korea, School of Medicine has several hospitals in affiliation such as Daejeon St. Mary's Hospital, Seoul St. Mary's Hospital, Catholic University St. Mary's Hospital, St. Vincent Hospital, Uijeongbu St. Mary's Hospital, but all those were counted as one hospital because the training schedule (contents of rotation curriculum and period of each course) were similar to each other. In case of Paik Hospital, there are affiliated hospitals of Ilsan Paik Hospital, Seoul Paik Hospital, Sanggye Paik Hospital, and Busan Paik Hospital, but those were counted as separate hospitals because the training schedules were different from each other.
If the response of the survey were ambiguous, it was complemented by talking to the subjects by phone directly. The survey was conducted for 2 months from June 2009 to the end of July 2009. In the end, 142 residents in 76 hospitals responded to the survey. The average response rates by person and by hospital were 40.7% and 75.2%, respectively.
The questionnaire consisted of demographic features, opinion on the duration of family medicine training program, conferences in training hospitals, practice of related specific procedures and interviewing, necessity of these procedures and interviewing, experience of seeing patients in outpatient clinics and caring for hospitalized patients, as well as writing thesis articles.
The statistic analysis was done using SPSS ver. 17.0. (SPSS Inc., Chicago, IL, USA). Pearson's chi-square test and Fisher's exact test was applied to analyze frequency and to verify statistical correlation of categorical variables.
Among 142 respondents, 77 (54.2%) were males and 65 (45.8%) were females; 73 (51.4%) were married whereas 69 (48.6%) were not. The average age was 31.8 years. Out of 76 hospitals, 31 (40.8%) were classified as certified general recuperation hospitals (tertiary hospitals) by the enforcement regulation of national health insurance law, whereas the other 45 hospitals (59.2%) were secondary hospitals. Fourteen (18.4%) hospitals were small-sized hospitals possessing less than 300 beds, 45 (59.2%) possessed 300-1,000 beds, and 17 (22.4%) had more than 1,000 beds. Among 142 resident physicians, 80 residents (56.3%) belonged to secondary hospitals and 62 (43.7%) to tertiary hospitals (Table 1).
As for the training period of the family medicine residency program, most respondents replied that 3 years was ideal (13.4%) or appropriate (80.3%), and only 9 (6.3%) respondents answered that it was inappropriate. To a question whether they would have applied for a family medicine program if it was a 2 year program, 22 (15.5%) replied yes, 110 (77.5%) replied no, and 10 (7.0%) did not respond (data not shown).
The reasons for yes replies were 'the shorter program is the better', '2 years is enough for a primary care training', and 'the period doesn't matter'. The reasons for no replies were '2 years is too short to acquire professional knowledge of family medicine', 'family medicine training is not differentiated from training of general practitioners', and 'physicians of other specialties may disregard our program'.
If family medicine was a 4 year training program, 42 (29.6%) replied that they would 'have applied for it', 90 (63.4%) replied that they 'would not have', and 10 (7.0%) did not respond. Those who would have applied said 'longer period of training could enhance degree of completion', and 'the period doesn't matter'. Those who would not have applied said '4 years is too long, and 3 years is enough for primary care training', 'training period of 3 years is the very strength of family medicine training', and 'if family medicine were a 4 year program, I would have applied for internal medicine' (Table 2).
1) The current state of conferences and residents' expectation Seventy-six hospitals out of 101 responded to the survey of frequency of conference. Twenty-six (34.2%) held conferences 5 or more times a week, 16 (21.1%) held conferences 4 times a week, 18 (23.7%) held conferences 3 times a week, showing that 79.0% of the family medicine departments hold conferences more than 3 times a week. Conferences were held during lunch time in 51 hospitals, and in early morning or late afternoon in 5 hospitals. Four responded 'early morning and lunch time', 5 responded 'early morning and late afternoon', and 6 responded 'during lunch and late afternoon', showing that most hospitals (61, 80.3%) hold conferences during lunch (data not shown).
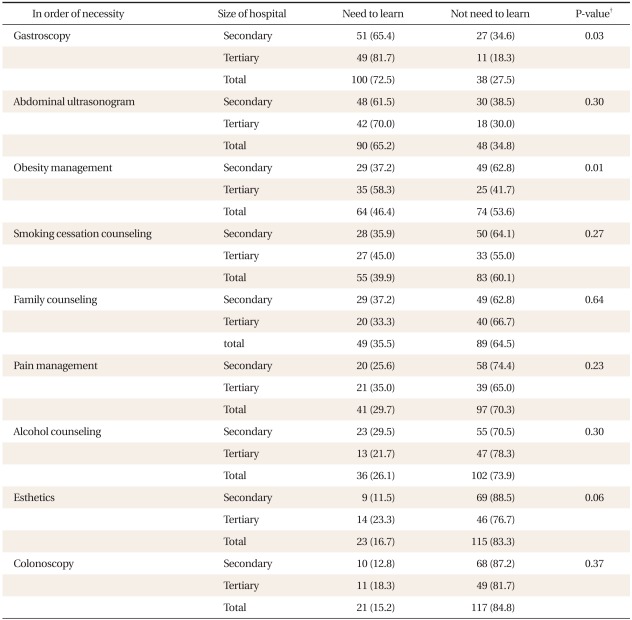
Most conferences were journal reviews. Journal review conferences were held in 74 hospitals (97.4%), and book reviews were held in 67 hospitals (88.2%). Clinical topic reviews were held in 61 hospitals (80.3%), and staff lectures were held in 51 hospitals (67.1%), which means that half of the hospitals held these type of conferences. In addition, the referred case review was held in 36 (47.4%) hospitals, conferences for discussion on the cases of hospitalized patients in family medicine (family grand round, FGR) was held in 19 (25.0%), tip meetings of sharing medical knowledge acquired in each rotation was held in 4 (18.4%), evidence based medicine seminar was held in 11 (14.5%), conference for learning interview skills (audiovisual meeting, AVM) was held in 8 (10.5%), and a medical ethics seminar was held in 1 hospital. Conferences were also held for complementary and alternative medicine (CAM), radiology, medical English, medical statistics, counseling technique, and psychosocial case study (Figure 1).
When questioned which conferences were helpful and thought to be necessary at the time of completing training, 115 respondents (81.0%) chose journal reviews, whereas 114 respondents (80.3%) chose staff lectures. These were followed by 104 respondents choosing clinical topic reviews (73.2%), 86 choosing book reviews (60.6%), 69 choosing referred case reviews (48.6%), 43 choosing tip meetings (30.3%), 34 choosing evidence based medicine seminars (23.9%), 26 choosing conferences for discussion on the cases of hospitalized patient of family medicine (18.3%), 22 choosing medical ethics seminar (15.5%), and 19 respondents choosing conference for learning interview skills (13.4%) (Figure 1).
2) The current state of training medical procedures and interviewing skills and residents' expectation
Among 76 hospitals, gastroscopy training was given in 71 (93.4%). Abdominal ultrasonography and obesity management training was given in 44 (57.9%) hospitals, whereas smoking cessation counseling and family counseling followed. Training programs included 15 minutes interview method, managing lymphedema, managing cancer patients, and dementia examination (Table 3).
As for obesity management, smoke cessation, and family counseling, the frequency of training experiences was statistically higher in tertiary hospitals than in secondary hospitals (P < 0.05). Obesity management was included in 19 training programs (43.2%) out of 44 secondary hospitals, and in 25 (83.3%) among 31 tertiary hospitals (P = 0.001). Smoking cessation counseling was included in 24 training programs (80.0%) among 44 secondary hospitals, and in 24 (80%) among 31 tertiary hospitals. Family counseling was included in 9 training programs (20.5%) among 44 secondary hospitals, and in 14 training programs (46.7%) among 31 tertiary hospitals (Table 3).
As for the residents' expectation of the primary medical procedures and interview skills, 100 (72.5%) of 138 residents responded that gastroscopy is a necessary procedure indicating the highest preference, while 90 (65.2%) replied that abdominal ultrasonography is a necessary procedure, and 64 (46.4%) replied that obesity management is necessary. These preferences were followed by smoking cessation counseling, pain management, and alcohol counseling. The preference for gastroscopy and pain management was higher in the residents of tertiary hospitals than those of secondary hospitals, and these findings were statistically significant (P = 0.03, P = 0.01) (Table 4).
To an open question of what types of further training residents would like to suggest to the Korean Academy of Family Medicine, 7 respondents requested training of dermatology, obesity management, and pain management, and 1 respondent requested hospital management education (data not shown).
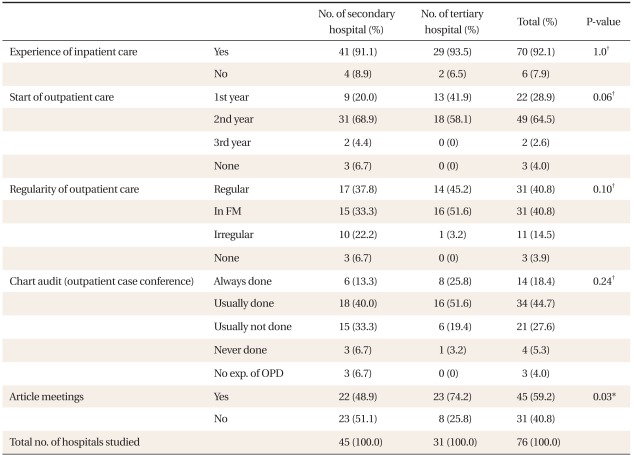
3) The current state of inpatient and outpatient care
In 70 (92.1%) out of 76 hospitals, residents treated inpatients of the family medicine department, but 6 (7.9%) did not have experience of inpatient care. To the question on the necessity of experiencing inpatient care in family medicine department, 116 (83.7%) of 142 respondents replied it is 'necessary'.
In 31 hospitals (68.9%), outpatient care was possible at the 2nd year of residency training, and this rate was the highest. In 2 out of 76 hospitals, only the 3rd year residents were allowed to see patients in outpatient clinic, whereas the 1st or 2nd year residents were not allowed. In 3 hospitals, family medicine residents were not allowed to see patients in the outpatient clinic during 3 years of training. In 49 hospitals (64.5%) residents began to see outpatients at the 2nd year of residency. As for the timing when residents wanted to start outpatient care, 38 (26.8%) respondents answered 1st year, 97 (68.3%) answered 2nd year, and 7 (4.9%) replied 3rd year (Table 5).
In 42 (55.3%) out of 76 hospitals, outpatient care experience was not continuously provided because residents see outpatients only during the time of family medicine rotation. In 31 hospitals (40.8%), continuous and regular outpatient care experience was provided regardless of the rotation schedule (Table 5).
In 48 (63.2%) out of 76 hospitals, chart audit was done by the professor in charge after outpatient clinic everyday or nearly everyday. However, in 21 hospitals (27.7%) chart audit was not done most days, and in 4 hospitals (5.3%) it was never done (Table 5).
Meeting of writing thesis articles was held in 22 (48.9%) out of 45 secondary hospitals, and 23 (74.2%) out of 31 tertiary hospitals, showing that the frequency is higher in tertiary hospitals (P = 0.03). As for the question of how helpful professors advice was in writing theses, 80 (56.3%) replied 'helpful', 37 (26.1%) replied 'mediocre', and 25 (17.6%) replied 'not helpful'. As for the current regulation that residents should submit two articles for certification including one article as a first author, 123 (86.6%) replied that it was acceptable, but 19 (13.4%) replied that the amount of articles should be reduced. Out of those 19, 15 replied that it should be reduced to one article with the submitter as a first author because submission system permitting the thesis with submitter's name as co-author is meaningless due to possibility of intentional interchanging of authors' names; 4 residents replied that it should be reduced to one article with the submitter as coauthor (data not shown).
Most 3rd year residents who almost completed family medicine training considered 3 year training period as ideal, which was in line with the results of the recent similar research on 4 year system of family medicine training in the US, in which 65.2% preferred the 3 year system.3)
Family medicine training program in Korea consists of rotating clinic experience in other departments of specialty and family medicine-specific training. According to the previous research, the training in other departments was often difficult when departments corresponding to the training course was not available in the hospital, or when the corresponding departments refused to offer training.8) Thus, a family medicine-specific training is considered the most important part and needs to be improved and utilized.
Journal, book, and clinical topic reviews were the most frequently held conferences and the most preferred ones by residents. It is characteristic that the residents' preference for staff lectures, referred case review, and tip meeting conferences was high compared to the present state of holding these conferences. This result should be considered when planning conferences for resident training because those conferences are highly related to other departments. Ethical aspects were emphasized by the family medicine training regulations revised in 2008. Only 1 residency program held a medical ethics seminar, while 15.5% of the respondents wanted ethics education. It is considered that not only knowledge but also humanity and ethics should be taught in standardized conferences of family medicine residency program.
Conferences were held 3 or more times a week in 79% of the hospitals. A total of 80.3% of the conferences were held during lunch time. Because rotating in other departments is the main component of family medicine residency training, lunch time was considered the most appropriate for holding conferences.
To an open question of the preference for procedures, the respondents wanted active experience of the practical procedures such as gastroscopy, abdominal ultrasonography, pain management, obesity management, and skin care. This result requires the effort of the faculty in charge of the training program and the effort on the level of the Korean Academy of Family Medicine. The training opportunity of obesity management, smoking cessation counseling, and family counseling is plenty in tertiary hospitals compared to secondary hospitals. The Korean Academy of Family Medicine should make an effort to support training programs of secondary hospitals whose educational resources are relatively limited.
According to the family medicine training regulations, residents should see at least 60 hospitalized patients including 10 at the department of family medicine at their 1st year, and at least 40 hospitalized patients at the 2nd year. Also, residents should see more than 100 outpatients at the 2nd year, and more than 200 outpatients at the 3rd year. However, this research shows that family medicine residency programs of 6 hospitals (7.9%) did not satisfy the minimum requirement in seeing inpatients, and 5 hospitals (6.5%) did not satisfy the minimum requirement for seeing outpatients. If it is not a temporary situation, the relevant hospitals should make an effort to satisfy the minimum requirement and the sanction of the Korean Academy of Family Medicine would be needed.
Chart audit after outpatient care is a feedback process that can improve residents' outpatient care skill. However, it was not done in 28 (36.9%) out of 76 hospitals. Urgent supplementation is needed due to the importance of outpatient care skill. As for writing theses, only 80 respondents (56.3%) replied that the professors' advice was helpful, and writing theses proved to be even more difficult in secondary hospitals. Discussion on how to reinforce usability of insufficient faculty advisors through regional affiliation between secondary and tertiary training hospitals will be needed.
The limitation of this research is that the response rate of residents was low (40.7%) because obtaining addresses of the family medicine residents nationwide was difficult due to the protection of personal information. However, the high response rate of hospitals (75.2%), which was possible by an effort to reach via mail, phone call, and e-mail, contributed to the reliability of the results.
The survey of the present state of residency programs is important because the level of competency of family physicians depends on what contents comprise residency program during the limited training period of 3 years. The opinion of the 3rd year residents on family medicine specific training is precious and should not be neglected when developing quality training program in order for family medicine to be established as a primary care specialty and to keep pace with the rapidly changing medical environment and disease patterns. It is suggested that the results of this research should be reevaluated at the level of the Korean Academy of Family Medicine and reflected in residency training.
References
2. Medical Education in Training Institute. Family medicine. Vol. 3. 2006. Seoul: Seoul National University Press.
3. Duane M, Dovey SM, Klein LS, Green LA. Follow-up on family practice residents' perspectives on length and content of training. J Am Board Fam Pract 2004;17:377-383. PMID: 15355952.


4. Kim MJ, Shin HC, Kim CH, Choi YS, Lee H, Choi AK, et al. The current educational measurement of family practice residents. J Korean Acad Fam Med 2007;28:616-625.
5. Lee SH, Paek YJ, Kim SY, Oh SW, Shim JY, Lee JK. Research and scholarly activity of residency programs of family medicine in Korea. J Korean Acad Fam Med 2004;25:826-834.
6. Lee JK. Training of family medicine residency pointed of educational professor. J Korean Acad Fam Med 2002;23(4 Suppl):S390-S392.
7. Lee SH. New paradigm of residency programs and goal of training of family medicine. J Korean Acad Fam Med 2002;23(11 Suppl):S136-S146.
8. Paek YJ, Shin HC, Kim CH, Choi YS, Lee H, Cho AK, et al. Curriculum and training difficulties of family medicine residency programs in Korea. J Korean Acad Fam Med 2007;28:367-374.
Figure 1
Conference incidence by hospital and preference by residents. JR: journal review, BR: book review, CTR: clinical topic review, SL: staff lecture, RCR: referred case review, FGR: family grand round, Tip: tip meeting, EBMS: evidence based medicine seminar, AVM: audiovisual meeting, MES: medical ethic seminar, other conferences: complementary and alternative medicine, X-ray conference, medical english, statistics, counseling technique, psychosocial case review.
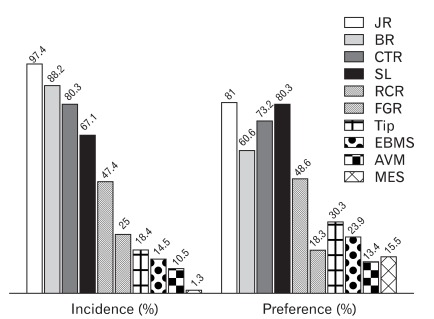
Table 2
Response to open-ended questions on application status and reasons according to residency duration.
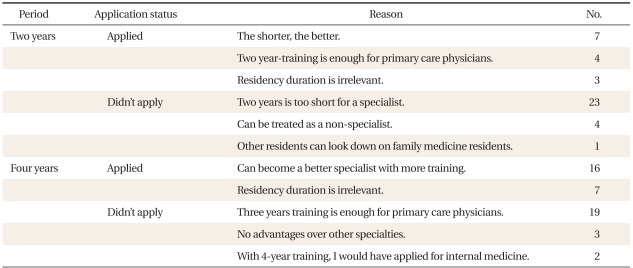
Table 3
Procedures and interview techniques by size of hospital (n = 74).*
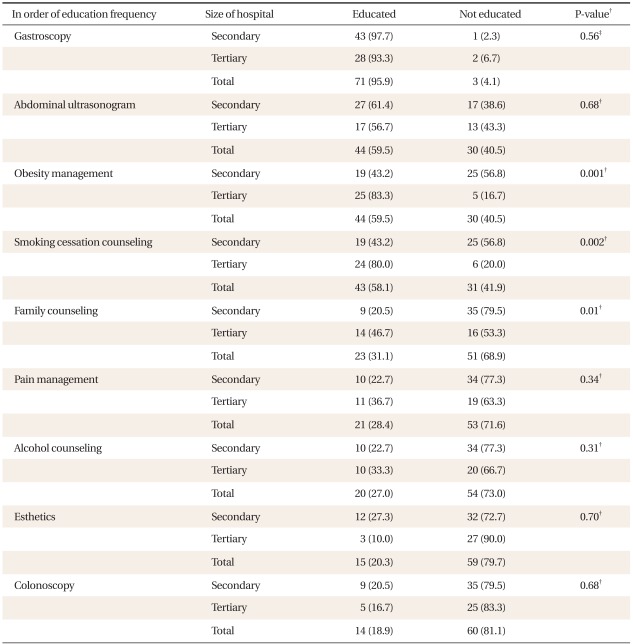
Values are presented as number (%). Other curriculum: 15 minutes interview, lymphedema · cancer pain management, dementia test.
*Two hospitals were excluded in analysis because of the ambiguous response which each resident has replied. †Chi-square test between the group of secondary hospital and tertiary hospital. ‡Fisher's exact test.