INTRODUCTION
Cardiac myxoma is a rare, benign primary cardiac neoplasm with an incidence of 0.09% among patients at a hospital-based cardiology unit.1) It frequently occurs in the left atrium of the heart.2) Atrial myxoma remains an elusive diagnosis since it is almost always an incidental finding.2) Electrocardiogram (ECG) abnormalities are uncommon in the presence of atrial myxoma.3) However, suspicious serial changes in ECG patterns could play a role in the detection of an atrial myxoma at a primary care setting.
CASE REPORT
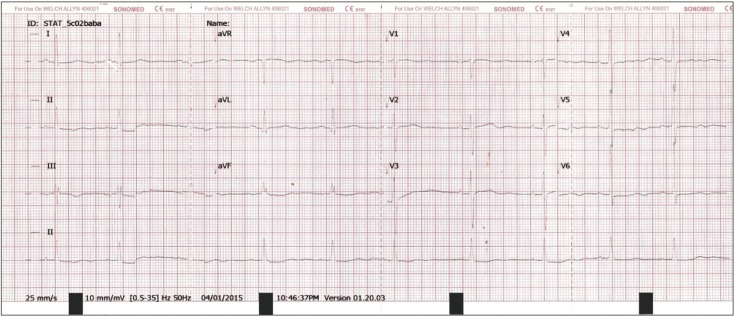
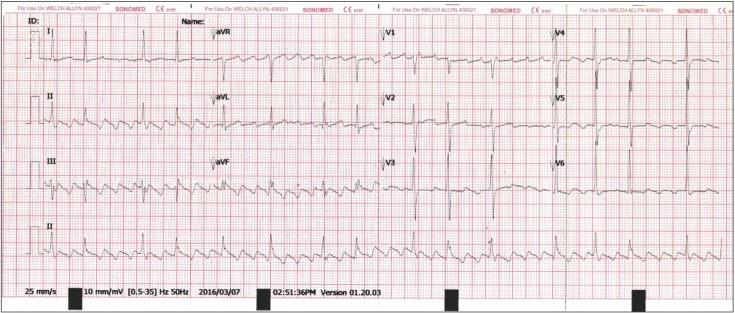
A 71-year-old lady presented with an abnormal ECG finding during a scheduled primary care appointment. She was asymptomic and had a history of type 2 diabetes mellitus, essential hypertension, and dyslipidemia. During the consultation, the ECG reading showed premature ventricular contraction at a 1:1 ratio (ventricular bigeminy) with a heart rate of 46/min (Figure 1). Her ECG from the previous year (Figure 2) showed non-specific changes, possibly related to early left ventricular hypertrophy. The recorded vital signs were as follows: blood pressure, 159/74 mm Hg; heart rate, 62/min; and respiratory rate, 18 breaths/min. On physical examination, heart murmurs were not audible and other findings were unremarkable. The laboratory findings were: glycated hemoglobin, 7.1%; urea, 10.0 mg/dL; creatinine 1.0 mg/dL; Na+, 137 mEq/L; and K+, 3.6 mEq/L. In order to rule out secondary causes that could have led to the changes in the ECG, various blood investigations were ordered. An urgent appointment was scheduled a week later to review these results. The patient was also advised to seek urgent medical attention if she felt palpitations or giddiness. During the second consultation, a week later, the repeat ECG showed atrial flutter with a 3:1 atrioventricular block (Figure 3). All the results of the blood investigations were normal (thyroid stimulating hormone, 4.26 ┬ĄIU/mL; Na+, 135 mEq/L; K+, 4.4 mEq/L; corrected Ca2+, 8.9 mg/dL; PO4-, 0.32 mg/dL; hemoglobin, 12.9 g/dL; and white blood cell count, 7.4├Ś103/┬ĄL), except for an elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels (88 mm/h and 9.8 mg/L).
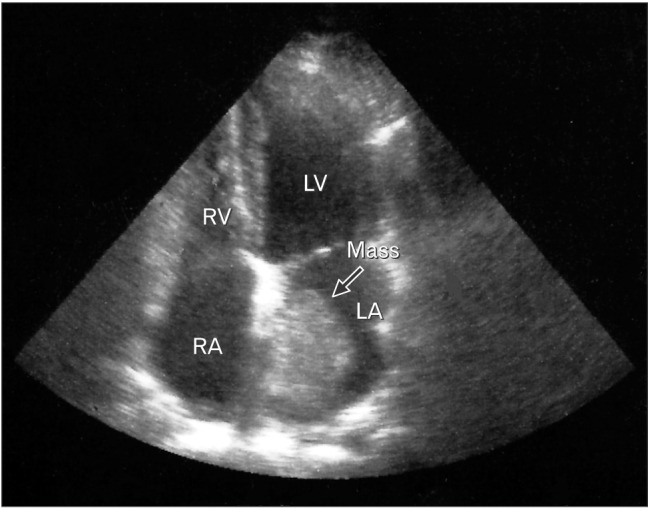
Urgent transthoracic echocardiography revealed a dilated left atrium and ventricle without any myocardial hypokinetic changes. A large echogenic mass measuring 3.1├Ś4.1 cm was identified at the left atrium (Figure 4). The mass was solid and appeared pedunculated, arising from a stalk at the endocardium. The patient had a left ventricular ejection fraction of 54%. The patient was immediately referred to a tertiary care cardiology clinic where a second transthoracic echocardiography was performed. An imaging diagnosis of left atrial myxoma was confirmed. The tumor measured approximately 2.9├Ś3.1 cm. A paroxysmal atrial fibrillation pattern was observed on the ECG. Warfarin treatment was initiated while aiming for a target international normalized ratio between 2 and 3. Currently, the patient is jointly cared for by the primary care physician and a multidisciplinary team that is helping to manage the anticoagulation therapy. The patient is unwilling to undergo surgery to remove the tumor.
DISCUSSION
Atrial myxoma is common in middle-aged women; women are affected twice as often as men.2,4,5) Although the origin of cardiac myxomas is uncertain, 10% of cases are familial.2) Familial type atrial myxomas can take the form of genetic myxoma syndromes such as the Carney complex.4,6) Depending on the size, site, and lesion composition, clinical presentation in patients can range from no symptoms to heart failure.2) Cardiac examination in patients with left atrial myxoma might reveal an early diastolic tumor plop, apical diastolic murmur, changes in pre-existing murmurs, gallop rhythm, or modification of the first (split) or second heart sound.3)
ECG findings may be nonspecific in 20% to 40% of patients.7) The most common ECG finding is left atrial hypertrophy (35%), followed by repolarization disorders (21%), conduction disorders (24%), and rhythm disorders (9%).3) Atrial fibrillation and atrial flutter are rare in left atrial myxoma.3) Chest radiograph findings are non-specific, and include pulmonary interstitial marking, congestive heart failure signs, non-specific cardiomegaly, and left atrial enlargement.3) Calcification linked to the tumor and pleural effusions are unusual.3)
Blood investigations might reveal an elevated ESR, CRP level, and white blood cell count.4,8) Transthoracic echocardiography should be performed on all patients with suspected atrial myxoma.5) Cardiac myxoma can be diagnosed without further imaging if echocardiography confirms the presence of a mobile mass attached to the endocardial surface by a stalk arising from the fossa ovalis.7)
In conclusion, suddent changes in ECG (especially if a previous ECG shows sinus rhythm) coupled with an elevated CRP ir ESR levels should prompt the clinician to rule out cardiac myxoma through transthoracic echocardiography. An urgent referral to a cardiologist is warranted if there is clinical presentation of an infected myxoma, systemic embolization, or non-specific constitutional symptoms.