 |
 |
- Search
| Korean J Fam Med > Volume 43(5); 2022 > Article |
|
See commentary "Meal Frequency, Metabolic Health, and Social Norms" in Volume 43 on page 275.
Abstract
Background
Previous studies have shown a close relationship between skipping breakfast and nutritional deficiency. However, the impact of regular eating, including lunch and dinner, has not been studied well. We explored the correlation between regularity and frequency of daily meals and nutritional status.
Methods
We analyzed Korea National Health and Nutrition Examination Surveys between 2016 and 2018. A total of 7,725 adults aged 19ŌĆō49 years were classified into four groups according to the regularity of meal intake: three-meal regular diet (3MRD), two-meal regular diet, one-meal regular diet, and irregular diet (IRD). Food and nutrient intake was assessed using the 24-hour recall method and estimated by a generalized linear model in complex sample weight variables.
Results
In IRD, there were relatively more females who were not married, lived alone, or reported low levels of education. As subjects ate more meals, more people felt thinner and healthier by themselves. Dietary intake of cereal, vegetables, seaweed, and fiber was directly proportional to the number of regular meals as well as essential components such as water, carbohydrates, protein, fat, and micronutrients. Contrarily, alcohol and beverage consumption was inversely proportional to the number of regular meals. Intake level of legumes, fish, fruits, seasonings, milk, oils, sugars, and cholesterol was consistent regardless of meal frequency.
It is widely believed that a regular diet consisting of three meals is healthy, and it is encouraged despite limited epidemiological and clinical evidence. Daily meal frequency is likely to be associated with food choices and lifestyles. Modern westernized lifestyles feature irregular eating patterns, such as skipping meals [1]. Reduced meal frequency by intermittent fasting has attracted much attention worldwide [2-4]. Kahleova et al. [5] reported in the Adventist Health Study 2, a relatively healthy North American cohort, that eating one or two daily meals was associated with a relatively lower body mass index (BMI) compared with three daily meals. Conversely, other studies demonstrated that a high daily meal frequency was associated with high leisure-time physical activity, non-smoking, low alcohol consumption, low caloric intake from fat alcohol, high caloric intake from carbohydrates, and high relative fiber intake [6].
There is a general consensus that breakfast improves consumersŌĆÖ diet and nutrition compared to breakfast skipping [7-10]. Previous studies have shown a close relationship between breakfast skipping and nutritional inadequacy. However, the impact of meal frequency and regularity, including lunch and dinner, has not been established. Most Asian countries, including Korea, now have diverse eating patterns due to the adoption of Western eating patterns. However, there are few studies on the association between the regularity and frequency of daily meals and individual nutritional status.
This study aimed to determine whether young and middle-aged Korean adults achieved a balanced diet and nutrition and to estimate possible nutritional differences between groups according to meal frequency. We hypothesized that a regular breakfast-lunch-dinner meal pattern, compared to irregular diets (IRDs) or meal skipping, would be related to higher diet quality and a healthier clinical parameter overall.
This cross-sectional study utilized data from the seventh Korea National Health and Nutrition Examination Survey (KNHANES) conducted between 2016 and 2018. Of the 24,269 subjects who had completed laboratory blood tests, physical examinations, and surveys during the participation, only 19,389 people aged 19 or older were included. We defined young adults in the present study as individuals aged 19ŌĆō49 years. Of the 24,269 subjects who had completed laboratory blood tests, physical examinations, and surveys during the participation, only 19,389 people within the age bracket were included. We further excluded participants with missing data on meal frequency, food intake, and nutrition. Thus, 7,725 subjects (3,270 men and 4,455 women) were included in the final analysis.
The general characteristics of the subjects were collected using standardized questionnaires. The data collected included age, sex, living status, marital status, education level, household income, place of residence, smoking, alcohol consumption, physical activity, dietary supplement, subjective health level, and subjective body shape. Age was classified as 19 to 29, 30 to 39, or 40 to 49 years old. The highest level of public education was divided into four groups: university, high school, middle school, and elementary school. Household income was also categorized into four groups: high, middle-high, middle-low, or low income. The place of residence was classified as urban or rural. Smoking consumption was divided into three groups: non-smokers or smokers of less than five packs (100 cigarettes) in their lifetime, ex-smokers who have smoked more than five packs in their lifetime, or current smokers regardless of the amount of smoking. We categorized alcohol consumption into four groups according to the frequency of drinking during the last year: non-drinkers who did not drink alcohol, mild-drinkers who drank less than once a month to 2ŌĆō4 times a month, moderate-drinkers who drink 2ŌĆō3 times a week, and heavy-drinkers who drank more than 4 times a week. Subjects were placed in the regular physical activity group upon meeting one of the following conditions: (1) more than 3 days per week of vigorous physical activity for 20 minutes or more, (2) more than 5 days per week of moderate physical activity for 30 minutes or more, or (3) more than 5 days a week of walking for 30 minutes or more.
Meal frequency was assessed using the question, ŌĆ£How many times a week did you have breakfast/lunch/dinner last year?ŌĆØ Only those checked 5 to 7 times a week were considered regular meals. For example, if breakfast is eaten 4 times/wk, 5 times/wk for lunch, and 6 times/ wk for dinner, this is regarded as a regular diet consisting of only two meals (i.e., lunch and dinner). Meal frequency was analyzed by combining the number and type of meals (breakfast, lunch, and dinner). According to the dietary survey, study subjects were further categorized into four groups based on meal frequency. The three-meal regular diet (3MRD) group included those who eat breakfast, lunch, and dinner more than 5 times a week. The two-meal regular diet (2MRD) group included those who eat breakfast and lunch, breakfast and dinner, or lunch and dinner regularly more than 5 times a week. Lastly, the one-meal regular diet (1MRD) group included those who eat only breakfast, only lunch, or only dinner regularly. Those who did not eat any meal more than 5 times a week were placed in the IRD group.
Food and nutrient intake was assessed by using the 24-hour recall method. Individual foods were categorized into 18 groups based on previous studies: total food, cereal and grain products, potatoes and starches, vegetables, seaweeds, meat and their products, eggs, legumes, seeds and nuts, mushrooms, fish and selfish, fruits, sugars and sweets, seasonings, milk and dairy products, beverages, liquor, oils and fats, and other foods. Daily energy and nutrient intake, including intake of total calories (kcal/d), carbohydrates (g/d), protein (g/d), and fat (g/d), were assessed. Total energy intake was calculated considering all foods consumed during 1 day before examination. The method was validated in Korea and published by the rural department administration Korean ministry of food, agriculture, forestry, and fisheries. We determined the inappropriateness of micronutrients based on the estimated average requirement (EAR) from Korean Dietary Reference Intakes (KDRIs).
Descriptive statistics were used to present the general characteristics of the study subjects. Univariate associations between risk factors and meal frequency were evaluated using PearsonŌĆÖs chi-square test. Multivariable-adjusted associations between meal frequency and food intake or nutrients were evaluated using general linear model analysis, taking into consideration the sampling weights for the standard Korean population. P-value <0.05 (two-sided) was considered statistically significant. Statistical analyses were performed using IBM SPSS Statistics ver. 24 for Windows (IBM Corp., Armonk, NY, USA).
The study was approved by the Institutional Review Board of the Samsung Medical Center (IRB no., SMC 2021-06-136). The informed consent requirement was waived because the subjects had given consent for the KNHANES. The dataset is in the public domain and does not include individually identifiable information.
The general characteristics of the study subjects are shown in Table 1. Overall, the majority of the subjects had a 2MRD (n=3,680), followed by 3MRD (n=2,841), 1MRD (n=1,019), and IRD (n=185). A 3MRD was more prevalent among those aged 40 and older, while those aged 19 to 39 more commonly ate two regular meals per day. Females were more likely to be irregular dieters (75.7%) and eat one regular meal daily (69.9%). Higher proportions of living alone and non-married status were found among IRD group. The proportion of people with low educational levels was high in the IRD group. Current smokers and drinkers were likely to eat two regular meals per day. The income level, place of residence, and physical activity were not related to the number of meals. People who eat more regularly tend to take dietary supplements. Subjective health level was directly proportional to the number of regular meals, while subjective body shape tended towards obesity as the number of meals decreased. The 3MRD group had a significantly lower weight (P<0.001), BMI (P<0.001), waist circumference (P=0.001), systolic blood pressure (P=0.028), and diastolic blood pressure (P<0.001). In addition, the 3MRD group had significantly lower serum fasting glucose (P=0.001), total cholesterol (P<0.001), and triglyceride (P<0.001) levels.
Table 2 shows the food intake of the study population. Dietary intake of cereal and grain products, as well as seaweeds, was directly proportional to the number of regular meals. On the contrary, alcohol and beverage consumption was inversely proportional to regular meals. In the IRD group, potatoes and eggs were the most consumed. The 2MRD group ate fewer fruits and eggs than other groups. It was prominent that 1MRD group most consumed meat, but least consumed vegetables. The intake levels of legumes, fish, fruits, seasonings, milk, and oils, as well as the consumption of sugars and cholesterol, were consistent regardless of the number of regular meals (Table 3). Conversely, the number of regular meals was proportional to the intake levels of energy, water, dietary fiber, carbohydrate, and protein, as well as essential components such as sodium, potassium, calcium, phosphorous, iron, and vitamins B1, B2, and B3. Fat and saturated fat consumption was higher in individuals who ate less than three regular meals daily. Breakfast skippers had a significantly higher intake of meat (P=0.009) and a lower intake of milk (P=0.010), calcium (P=0.002), phosphorous (P=0.035), and riboflavin (P=0.003) than others in the 2MRD group (Supplements 1, 2). Individuals who only have breakfast was shown a higher intake of carbohydrate such as cereal and grain product among the 1MRD group (Supplements 3, 4).
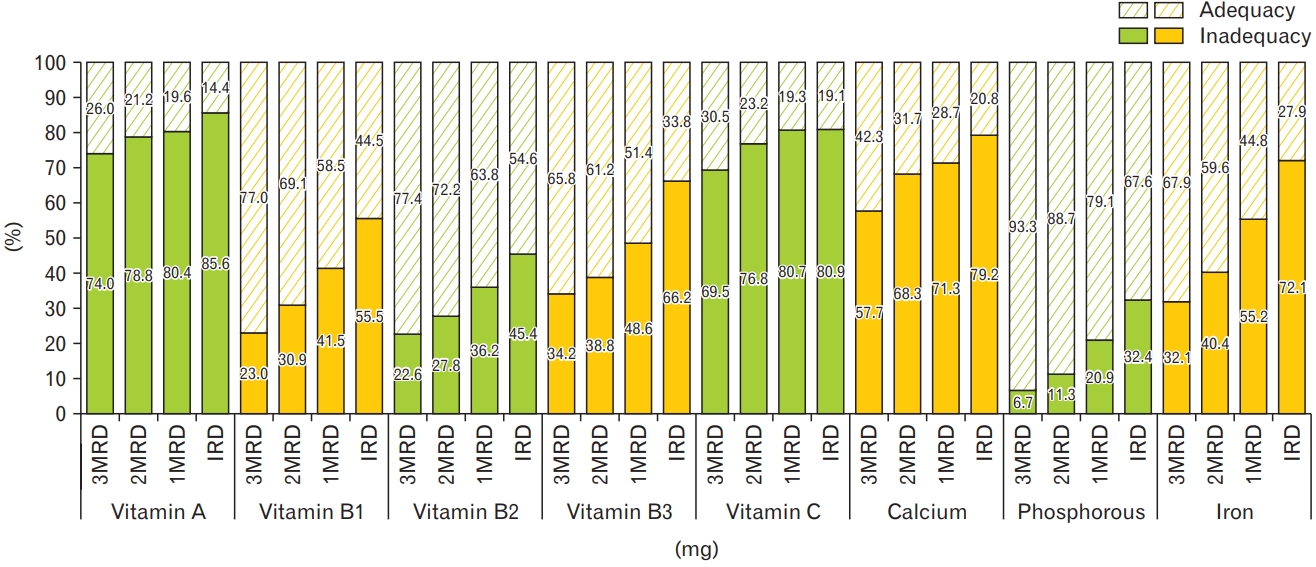
The inadequacy of micronutrients based on EAR from KDRIs is presented in Table 4. The vast majority of study subjects in each meal group showed very low compliance with micronutrient intake recommendations with vitamin A (proportion of population below EAR; 3MRD: 74%, 2MRD: 78.8%, 1MRD: 80.4%, IRD: 85.6%), vitamin C (69.5%, 76.8%, 80.7%, 80.9%), and calcium (57.7%, 68.3%, 71.3%, 79.2%) intakes being below daily dietary recommendations, whereas phosphorous exceeded the daily suggested intakes (Figure 1). Calcium was significantly (P=0.002) deficient in the diet of breakfast skippers (Supplement 5). There was no significant difference in inadequcy of micronutrients among 1MRD group (Supplement 6).
To our knowledge, this is the first study to evaluate dietary patterns and nutritional status by meal frequency. We also assessed the importance of regular intake of breakfast, lunch, and dinner. In accordance with our hypotheses, our findings suggest that regularly eating three meals per day is beneficial for young and middle-aged Korean adults. Women who lived alone, were unmarried, or had low educational attainment were likely to eat irregularly and subjectively feel obese and unhealthy. Bae et al. [11] assessed different health behaviors between single- and multiple-member households. They found that women who lived alone ate less food high in fat and exercised more. However, income level, place of residence, and physical activity, which are known confounding factors, are not associated with meal frequency in our study.
Numerous epidemiological studies reported that high eating frequency has a potential protective effect on body composition. Schoenfeld et al. [12] conducted a meta-analysis of 15 studies to establish the effect of eating frequency on fat reduction. Frequent feedings enhance the retention of free fat mass, possible muscle protein accretion, and postprandial thermogenesis, the increase in heat production that occurs for up to 8 hours after a meal. [13] This result was supported by Canuto et al. [14] with a systematic review of 31 articles that showed an inverse relationship between eating frequency and the BMI and visceral obesity of men. It has been hypothesized that increased eating frequency also affects appetite control and improves dietary-induced thermogenesis, lipidemia, and glycemia [15-17]. High meal frequency generally led to lower peaks (P<0.05) in perceived appetite, satiety, glucose, insulin, ghrelin, and PYY responses compared with low meal frequency [18]. Controlled feeding studies conducted by Leidy and Campbell [19] suggested that high meal frequency (>3 meals per day) has minimal, if any, impact on appetite control and food intake, whereas low meal frequency (<3 meals per day) negatively affects appetite control.
Daily meal frequency have been related to differences in dietary quality. Holmback et al. [6] indicated that increased eating frequency was associated with increased energy derived from carbohydrates, increased relative fiber intake, and less energy derived from protein and fat. Our results were similar except for increased protein consumption in the 3MRD group. The group also showed a higher intake of calories, macronutrients, and micronutrients than other groups. Except for the 3MRD group, none of the groups met the EAR of energy intake. We believed that reducing caloric intake rather than eating frequency was more relevant in preventing weight gain [20]. However, calorie restriction was not associated with weight loss in our study. Reduced meal frequency is associated with an irregular eating pattern that could cause weight gain by increasing hunger-related hormones, ultimately leading to metabolic disturbances that may increase cardiovascular risk [21]. Thus, a regular meal pattern potentially has positive effects on health outcomes regardless of meal frequency.
In this study, the participants of the KNHANES, a large nationwide population-based sample with a high response rate, were representative of the source population. We only included young and middle-aged adults from 19 to 49 because the nutrition plan for sedentary women is different from that of premenopausal women [22]. In addition, retirement, a major transition in life, affects food habits [23,24]. Previous studies have defined the frequency of meals based on the dichotomous responses to the question, ŌĆ£did you have breakfast/lunch/dinner yesterday?ŌĆØ 25) We attempted to overcome this source of potential bias by assessing meal frequency and regularity over an average of 1 week per year, and at least five meals a week were determined as regular meals [26].
This study was limited by recall bias, as a self-reported questionnaire was used with a 24-hour recall method. Furthermore, snack survey items were not collected and could affect the results in the 7th KNHANES. It is also a cross-sectional study and thus cannot determine causal inference. However, by adopting stratification, clustering, and sample weight variables, the study population was a nationally representative estimate of the Korean population. Studies that include Koreans remain very limited. Additional well-defined studies, including food information with snacks, are needed to clarify the role of fasting time with the regularity and frequency of meals.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4082/kjfm.21.0149.
Supplement┬Ā1.
Food intake of the subjects according to the dietary pattern in the two-meal regular diet group.
Supplement┬Ā2.
Energy and nutrient intakes of subjects according to the dietary pattern in the two-meal regular diet group.
Supplement┬Ā3.
Food intake of the subjects according to the dietary pattern in one-meal regular diet group.
Supplement┬Ā4.
Energy and nutrient intakes of subjects according to the dietary pattern in one-meal regular diet group.
Supplement┬Ā5.
Inadequacy of micronutrients compared by estimated average requirement in two-meal regular diet group.
Supplement┬Ā6.
Inadequacy of micronutrients compared by estimated average requirement in onemeal regular diet group.
Figure.┬Ā1.
Proportion of population below estimated average requirement for micronutrients. 3MRD, three-meal regular diet; 2MRD, two-meal regular diet; 1MRD, one-meal regular diet; IRD, irregular diet.
Table┬Ā1.
General characteristics of the subjects according to the meal frequency (total=7,725)
| Characteristic | 3MRD | 2MRD | 1MRD | IRD | P-value |
|---|---|---|---|---|---|
| No. of subjects | 2,841 | 3,680 | 1,019 | 185 | |
| Age (y) | <0.001 | ||||
| ŌĆā19ŌĆō29 | 465 (16.4) | 1,069 (29.0) | 354 (34.7) | 70 (37.8) | |
| ŌĆā30ŌĆō39 | 857 (30.2) | 1,358 (36.9) | 389 (38.2) | 69 (37.3) | |
| ŌĆā40ŌĆō49 | 1,519 (53.5) | 1,253 (34.0) | 276 (27.1) | 46 (24.9) | |
| ŌĆāMean┬▒SE | 37.74┬▒0.22 | 33.87┬▒0.21 | 32.42┬▒0.35 | 31.91┬▒0.73 | <0.001* |
| Sex (female) | 1,650 (58.1) | 1,953 (53.1) | 712 (69.9) | 140 (75.7) | <0.001 |
| Living status (living alone) | 113 (4.0) | 323 (8.8) | 98 (9.6) | 26 (14.1) | <0.001 |
| Marital status (married) | 2,140 (75.3) | 2,296 (62.4) | 605 (59.4) | 97 (52.4) | <0.001 |
| Educational level | <0.001 | ||||
| ŌĆā<Elementary school | 16 (0.6) | 23 (0.7) | 16 (1.7) | 3 (1.7) | |
| ŌĆāMiddle school | 71 (2.8) | 86 (2.6) | 23 (2.5) | 5 (2.9) | |
| ŌĆāHigh school | 860 (33.8) | 1,256 (38.1) | 389 (41.6) | 82 (47.7) | |
| ŌĆā>University | 1,595 (62.7) | 1,932 (58.6) | 507 (54.2) | 82 (47.7) | |
| Income level | 0.074 | ||||
| ŌĆāLow | 689 (24.3) | 955 (26.0) | 286 (28.1) | 58 (31.4) | |
| ŌĆāMiddle-low | 687 (24.2) | 913 (24.9) | 249 (24.4) | 45 (24.3) | |
| ŌĆāMiddle-high | 710 (25.0) | 945 (25.7) | 248 (24.3) | 42 (22.7) | |
| ŌĆāHigh | 752 (26.5) | 861 (23.4) | 236 (23.2) | 40 (21.6) | |
| Place of residence (urban) | 1,288 (45.3) | 1,769 (48.1) | 515 (50.5) | 91 (49.2) | 0.198 |
| Smoking status | <0.001 | ||||
| ŌĆāCurrent smoker | 397 (15.1) | 848 (24.8) | 207 (21.7) | 37 (21.0) | |
| ŌĆāEx-smoker | 462 (17.5) | 594 (17.4) | 129 (13.5) | 22 (12.5) | |
| ŌĆāNon-smoker | 1,777 (67.4) | 1,980 (57.9) | 619 (64.8) | 117 (66.5) | |
| Drinking status | <0.001 | ||||
| ŌĆāHeavy drinker | 107 (4.4) | 206 (6.2) | 56 (6.2) | 12 (6.7) | |
| ŌĆāModerate drinker | 433 (17.4) | 695 (21.4) | 195 (21.0) | 33 (17.9) | |
| ŌĆāMild drinker | 1,570 (60.5) | 2,069 (60.9) | 579 (60.8) | 102 (61.4) | |
| ŌĆāNever drinker | 527 (17.7) | 452 (11.6) | 125 (12.0) | 29 (14.0) | |
| Physical activity (yes) | 1,316 (51.8) | 1,632 (49.5) | 494 (52.8) | 86 (50.0) | 0.129 |
| Dietary supplement (yes) | 1,543 (54.3) | 1,647 (44.8) | 430 (42.2) | 75 (40.5) | <0.001 |
| Subjective health level | <0.001 | ||||
| ŌĆāGood | 963 (37.8) | 1,092 (33.1) | 262 (28.0) | 48 (27.9) | |
| ŌĆāWell | 1,286 (50.5) | 1,801 (54.5) | 536 (57.3) | 88 (51.2) | |
| ŌĆāBad | 300 (11.8) | 410 (12.4) | 137 (14.7) | 36 (20.9) | |
| Subjective body shape | 0.003 | ||||
| ŌĆāThin | 369 (14.0) | 549 (16.0) | 103 (10.8) | 15 (8.5) | |
| ŌĆāNormal | 1,043 (39.6) | 1,256 (36.7) | 355 (37.2) | 66 (37.5) | |
| ŌĆāObese | 1,225 (46.5) | 1,617 (47.3) | 497 (52.0) | 95 (54.0) | |
| Chronic disease | |||||
| ŌĆāHypertension | 354 (13.4) | 388 (11.3) | 101 (10.6) | 19 (10.7) | 0.009 |
| ŌĆāDiabetes mellitus | 98 (3.9) | 130 (3.9) | 24 (2.7) | 5 (3.0) | 0.233 |
| ŌĆāHypercholesterolemia | 292 (11.5) | 382 (11.5) | 102 (11.3) | 13 (7.7) | 0.417 |
| ŌĆāHypertriglyceridemia | 235 (11.7) | 368 (14.2) | 77 (10.5) | 14 (10.7) | 0.053 |
| ŌĆāAnemia | 265 (10.2) | 264 (7.8) | 90 (9.7) | 18 (10.4) | 0.022 |
| Anthropometric | |||||
| ŌĆāHeight (cm)ŌĆĀ | 167.68┬▒0.14 | 167.76┬▒0.11 | 167.47┬▒0.21 | 167.40┬▒0.49 | 0.560* |
| ŌĆāWeight (kg)ŌĆĀ | 66.54┬▒0.26 | 67.31┬▒0.23 | 68.64┬▒0.46 | 68.43┬▒0.92 | <0.001* |
| ŌĆāBody mass index (kg/m2)ŌĆĀ | 23.53┬▒0.09 | 23.76┬▒0.08 | 24.34┬▒0.15 | 24.31┬▒0.29 | <0.001* |
| ŌĆāWaist circumference (cm)ŌĆĀ | 80.23┬▒0.22 | 80.81┬▒0.20 | 81.88┬▒0.39 | 81.60┬▒0.74 | 0.001* |
| ŌĆāSystolic blood pressure (mm Hg)ŌĆĪ | 112.34┬▒0.30 | 112.61┬▒0.28 | 113.14┬▒0.46 | 115.12┬▒0.90 | 0.028* |
| ŌĆāDiastolic blood pressure (mm Hg)ŌĆĪ | 74.97┬▒0.22 | 75.94┬▒0.21 | 76.55┬▒0.36 | 76.88┬▒0.78 | <0.001* |
| Biochemical | |||||
| ŌĆāFasting glucose (mg/dL)┬¦ | 93.93┬▒0.33 | 95.73┬▒0.35 | 95.72┬▒0.72 | 95.69┬▒1.17 | 0.001* |
| ŌĆāHemoglobin A1c (%)┬¦ | 5.40┬▒0.01 | 5.43┬▒0.01 | 5.41┬▒0.02 | 5.42┬▒0.04 | 0.341* |
| ŌĆāTotal cholesterol (mg/dL)Ōłź | 188.56┬▒0.84 | 192.79┬▒0.68 | 195.02┬▒1.33 | 189.29┬▒2.82 | <0.001* |
| ŌĆāTriglyceride (mg/dL)Ōłź | 123.75┬▒2.49 | 136.01┬▒2.17 | 145.00┬▒5.33 | 141.84┬▒11.77 | <0.001* |
| ŌĆāHDL-C (mg/dL)Ōłź | 52.51┬▒0.31 | 52.22┬▒0.22 | 52.20┬▒0.45 | 51.45┬▒0.94 | 0.666* |
| ŌĆāLDL-C (mg/dL)Ōłź | 119.91┬▒0.23 | 122.61┬▒1.55 | 122.04┬▒3.13 | 129.16┬▒11.66 | 0.750* |
| ŌĆāHemoglobinŌĆĀ | 14.34┬▒0.03 | 14.35┬▒0.02 | 14.43┬▒0.04 | 14.54┬▒0.09 | 0.098* |
| ŌĆāHematocritŌĆĀ | 43.77┬▒0.08 | 43.81┬▒0.07 | 44.08┬▒0.12 | 44.20┬▒0.25 | 0.073* |
Values are presented as unweighted number (%) or estimated mean┬▒SE. P-values are obtained by cross-tabulation analysis (PearsonŌĆÖs chi-square test) in complex sample designs.
3MRD, three-meal regular diet; 2MRD, two-meal regular diet; 1MRD, one-meal regular diet; IRD, irregular diet; SE, standard error; HDL-C, high-density lipoprotein-cholesterol; LDL-C, low-density lipoprotein-cholesterol.
Table┬Ā2.
Food intake of the subjects according to the meal frequency (total=7,725)
| Variable | 3MRD | 2MRD | 1MRD | IRD | P-value |
|---|---|---|---|---|---|
| No. of subjects | 2,841 | 3,680 | 1,019 | 185 | |
| Total food (g/d)* | 1,689.45┬▒12.13 | 1,732.82┬▒11.57 | 1,733.39┬▒19.37 | 1,694.32┬▒36.61 | 0.039 |
| Cereal and grain products** | 315.54┬▒3.17 | 295.95┬▒2.82 | 282.21┬▒5.22 | 272.82┬▒11.00 | <0.001 |
| Potatoes and starches** | 68.85┬▒3.33 | 52.30┬▒2.42 | 46.95┬▒4.12 | 64.94┬▒9.72 | 0.009 |
| Vegetables** | 306.34┬▒4.31 | 274.14┬▒3.27 | 263.09┬▒5.73 | 264.98┬▒15.36 | <0.001 |
| Seaweeds** | 46.85┬▒3.41 | 38.92┬▒3.11 | 29.79┬▒3.36 | 23.05┬▒5.27 | <0.001 |
| Meat and their products** | 169.50┬▒4.31 | 178.75┬▒3.65 | 192.96┬▒6.61 | 161.75┬▒10.47 | 0.007 |
| Eggs* | 51.89┬▒1.62 | 45.76┬▒1.12 | 46.77┬▒3.39 | 51.37┬▒6.70 | 0.023 |
| Legumes | 51.65┬▒2.42 | 50.86┬▒2.86 | 40.97┬▒3.32 | 51.13┬▒8.48 | 0.051 |
| Seeds and nuts* | 8.60┬▒0.87 | 6.78┬▒0.97 | 8.93┬▒1.46 | 5.12┬▒0.98 | 0.034 |
| Mushrooms* | 16.21┬▒0.95 | 12.96┬▒0.64 | 14.74┬▒1.52 | 13.53┬▒2.50 | 0.039 |
| Fish and selfish | 126.61┬▒3.77 | 131.36┬▒4.18 | 125.85┬▒6.88 | 106.68┬▒11.00 | 0.144 |
| Fruits | 211.59┬▒6.18 | 197.36┬▒6.77 | 201.55┬▒12.24 | 201.47┬▒38.49 | 0.493 |
| Sugars and sweets | 13.07┬▒0.53 | 13.12┬▒0.44 | 13.45┬▒0.86 | 16.19┬▒2.61 | 0.687 |
| Seasonings | 40.86┬▒0.83 | 42.13┬▒0.70 | 41.34┬▒1.24 | 41.45┬▒3.36 | 0.689 |
| Milk and dairy products | 206.58┬▒5.61 | 196.85┬▒5.00 | 206.79┬▒11.22 | 211.40┬▒30.70 | 0.543 |
| Beverages** | 306.73┬▒8.26 | 362.56┬▒7.51 | 401.13┬▒15.49 | 422.70┬▒36.41 | <0.001 |
| Liquor** | 422.80┬▒21.14 | 596.85┬▒19.67 | 633.84┬▒36.00 | 819.43┬▒631.4 | <0.001 |
| Oil and fats | 8.85┬▒0.22 | 9.23┬▒0.21 | 9.55┬▒0.36 | 9.53┬▒0.70 | 0.336 |
| Other food* | 35.53┬▒9.14 | 11.12┬▒2.57 | 17.31┬▒5.42 | 9.03┬▒1.36 | 0.044 |
Table┬Ā3.
Energy and nutrient intakes of subjects according to the meal frequency (total=7,725)
| Variable | 3MRD | 2MRD | 1MRD | IRD | P-value |
|---|---|---|---|---|---|
| No. of subjects | 2,841 | 3,680 | 1,019 | 185 | |
| Energy intake (Kcal)** | 2,246.34┬▒21.77 | 2,171.78┬▒20.01 | 1,983.09┬▒32.44 | 1,838.45┬▒89.83 | <0.001ŌĆĀ |
| Water (g)** | 1,058.69┬▒11.83 | 1,037.90┬▒11.14 | 1,011.62┬▒18.40 | 921.04┬▒37.55 | 0.003 |
| Dietary fiber (g)** | 24.98┬▒0.25 | 22.43┬▒0.21 | 21.27┬▒0.38 | 20.82┬▒0.73 | <0.001 |
| Carbohydrates (g)** | 314.32┬▒1.81 | 292.79┬▒1.72 | 281.93┬▒2.82 | 276.43┬▒6.51 | <0.001 |
| Protein (g)** | 81.98┬▒0.63 | 80.12┬▒0.56 | 79.16┬▒0.98 | 73.46┬▒1.82 | <0.001 |
| Fat (g)** | 54.02┬▒0.60 | 55.92┬▒0.56 | 58.62┬▒0.95 | 55.67┬▒1.97 | 0.001 |
| Saturated fat (g)** | 17.60┬▒0.24 | 18.50┬▒0.23 | 19.67┬▒0.38 | 18.49┬▒0.77 | <0.001 |
| Cholesterol (mg) | 296.31┬▒4.74 | 291.48┬▒3.95 | 302.92┬▒8.57 | 293.80┬▒15.46 | 0.628 |
| Total sugars (g) | 65.82┬▒0.95 | 65.55┬▒0.85 | 67.43┬▒1.39 | 66.53┬▒3.33 | 0.685 |
| Sodium (mg)* | 3,732.63┬▒39.63 | 3,723.29┬▒32.71 | 3,691.96┬▒6.19 | 3,395.71┬▒112.4 | 0.039 |
| Potassium (mg)** | 2,987.18┬▒20.03 | 2,765.34┬▒18.70 | 2,676.20┬▒30.54 | 2,544.96┬▒65.61 | <0.001 |
| Calcium (mg)** | 567.50┬▒7.20 | 517.16┬▒5.20 | 500.58┬▒8.43 | 493.82┬▒29.01 | <0.001 |
| Phosphorous (mg)** | 1,185.35┬▒7.70 | 1,121.20┬▒6.32 | 1,094.66┬▒10.13 | 1,035.32┬▒24.79 | <0.001 |
| Iron (mg)** | 13.08┬▒0.16 | 11.97┬▒0.12 | 11.77┬▒0.19 | 10.88┬▒0.44 | <0.001 |
| Vitamin A (╬╝gRAE)** | 418.41┬▒8.32 | 388.40┬▒7.69 | 418.51┬▒28.84 | 345.30┬▒18.36 | 0.002 |
| Beta-carotene (╬╝g)** | 2,813.31┬▒55.12 | 2,531.46┬▒44.42 | 2,677.66┬▒303.3 | 2,364.96┬▒181.4 | <0.001 |
| Retinol (╬╝g)** | 183.18┬▒7.01 | 176.86┬▒6.37 | 194.75┬▒13.19 | 146.91┬▒11.08 | 0.008 |
| Thiamine (mg)** | 1.48┬▒0.01 | 1.40┬▒0.01 | 1.38┬▒0.02 | 1.27┬▒0.05 | <0.001 |
| Riboflavin (mg)* | 1.81┬▒0.02 | 1.75┬▒0.01 | 1.75┬▒0.03 | 1.67┬▒0.06 | 0.018 |
| Niacin (mg)** | 15.42┬▒0.17 | 15.01┬▒0.14 | 15.01┬▒0.29 | 13.66┬▒0.47 | 0.006 |
| Vitamin C (mg)** | 68.53┬▒1.76 | 60.58┬▒1.51 | 61.12┬▒3.14 | 64.38┬▒9.45 | 0.004 |
Table┬Ā4.
Inadequacy of micronutrient compared by estimated average requirement (total=7,725)
| Variable | 3MRD | 2MRD | 1MRD | IRD | P-value |
|---|---|---|---|---|---|
| No. of subjects | 2,841 | 3,680 | 1,019 | 185 | |
| Energy intake (kcal) | 20.48┬▒21.94 | -49.20┬▒20.17 | -239.62┬▒32.39 | -386.88┬▒89.66 | <0.001* |
| Calcium (mg) | -11.48┬▒7.19 | -61.32┬▒5.21 | -78.03┬▒8.42 | -85.04┬▒29.06 | <0.001 |
| Phosphorous (mg) | 605.38┬▒7.70 | 541.20┬▒6.32 | 514.66┬▒10.12 | 455.32┬▒24.79 | <0.001 |
| Iron (mg) | 3.64┬▒0.16 | 2.53┬▒0.12 | 2.33┬▒0.19 | 1.44┬▒0.44 | <0.001 |
| Vitamin A (╬╝gRAE) | -88.72┬▒8.31 | -118.22┬▒7.68 | -88.21┬▒28.84 | -161.56┬▒18.38 | 0.002 |
| Thiamine (mg) | 0.52┬▒0.01 | 0.45┬▒0.01 | 0.43┬▒0.02 | 0.32┬▒0.05 | <0.001 |
| Riboflavin (mg) | 0.65┬▒0.02 | 0.59┬▒0.01 | 0.60┬▒0.03 | 0.52┬▒0.06 | 0.018 |
| Niacin (mg) | 3.90┬▒0.17 | 3.50┬▒0.14 | 3.49┬▒0.29 | 2.14┬▒0.47 | 0.006 |
| Vitamin C (mg) | -6.47┬▒1.76 | -14.42┬▒1.52 | -13.88┬▒3.14 | -10.62┬▒9.45 | 0.004 |
REFERENCES
1. Sample CH, Martin AA, Jones S, Hargrave SL, Davidson TL. Western-style diet impairs stimulus control by food deprivation state cues: implications for obesogenic environments. Appetite 2015;93:13-23.



2. Mattson MP, Longo VD, Harvie M. Impact of intermittent fasting on health and disease processes. Ageing Res Rev 2017;39:46-58.



3. Horne BD, Muhlestein JB, Anderson JL. Health effects of intermittent fasting: hormesis or harm?: a systematic review. Am J Clin Nutr 2015;102:464-70.


4. Hu D, Xie Z, Ye Y, Bahijri S, Chen M. The beneficial effects of intermittent fasting: an update on mechanism, and the role of circadian rhythm and gut microbiota. Hepatobiliary Surg Nutr 2020;9:597-602.



5. Kahleova H, Lloren JI, Mashchak A, Hill M, Fraser GE. Meal frequency and timing are associated with changes in body mass index in Adventist Health Study 2. J Nutr 2017;147:1722-8.



6. Holmback I, Ericson U, Gullberg B, Wirfalt E. A high eating frequency is associated with an overall healthy lifestyle in middle-aged men and women and reduced likelihood of general and central obesity in men. Br J Nutr 2010;104:1065-73.


7. Uzhova I, Mullally D, Penalvo JL, Gibney ER. Regularity of breakfast consumption and diet: insights from national adult nutrition survey. Nutrients 2018;10:1578.



8. Ruiz E, Avila JM, Valero T, Rodriguez P, Varela-Moreiras G. Breakfast consumption in Spain: patterns, nutrient intake and quality: findings from the ANIBES study, a study from the international breakfast research initiative. Nutrients 2018;10:1324.



9. Yoo KB, Suh HJ, Lee M, Kim JH, Kwon JA, Park EC. Breakfast eating patterns and the metabolic syndrome: the Korea National Health and Nutrition Examination Survey (KNHANES) 2007-2009. Asia Pac J Clin Nutr 2014;23:128-37.

10. Cho S, Dietrich M, Brown CJ, Clark CA, Block G. The effect of breakfast type on total daily energy intake and body mass index: results from the third National Health and Nutrition Examination Survey (NHANES III). J Am Coll Nutr 2003;22:296-302.


11. Bae S, Urrutia-Rojas X, Patel D, Migala WM, Rivers PA, Singh KP. Comparison of health behaviors among single- and multiple-member households. Am J Health Behav 2007;31:514-25.


12. Schoenfeld BJ, Aragon AA, Krieger JW. Effects of meal frequency on weight loss and body composition: a meta-analysis. Nutr Rev 2015;73:69-82.


13. Tai MM, Castillo P, Pi-Sunyer FX. Meal size and frequency: effect on the thermic effect of food. Am J Clin Nutr 1991;54:783-7.


14. Canuto R, da Silva Garcez A, Kac G, de Lira PI, Olinto MT. Eating frequency and weight and body composition: a systematic review of observational studies. Public Health Nutr 2017;20:2079-95.



15. Farshchi HR, Taylor MA, Macdonald IA. Beneficial metabolic effects of regular meal frequency on dietary thermogenesis, insulin sensitivity, and fasting lipid profiles in healthy obese women. Am J Clin Nutr 2005;81:16-24.


16. Jenkins DJ, Wolever TM, Vuksan V, Brighenti F, Cunnane SC, Rao AV, et al. Nibbling versus gorging: metabolic advantages of increased meal frequency. N Engl J Med 1989;321:929-34.


17. LeBlanc J, Mercier I, Nadeau A. Components of postprandial thermogenesis in relation to meal frequency in humans. Can J Physiol Pharmacol 1993;71:879-83.


18. Smeets AJ, Westerterp-Plantenga MS. Acute effects on metabolism and appetite profile of one meal difference in the lower range of meal frequency. Br J Nutr 2008;99:1316-21.


19. Leidy HJ, Campbell WW. The effect of eating frequency on appetite control and food intake: brief synopsis of controlled feeding studies. J Nutr 2011;141:154-7.


20. Mills JP, Perry CD, Reicks M. Eating frequency is associated with energy intake but not obesity in midlife women. Obesity (Silver Spring) 2011;19:552-9.



21. Paoli A, Tinsley G, Bianco A, Moro T. The influence of meal frequency and timing on health in humans: the role of fasting. Nutrients 2019;11:719.



22. Meeta M, Digumarti L, Agarwal N, Vaze N, Shah R, Malik S. Clinical practice guidelines on menopause: *an executive summary and recommendations: Indian Menopause Society 2019-2020. J Midlife Health 2020;11:55-95.



23. Si Hassen W, Castetbon K, Lelievre E, Lampure A, Hercberg S, Mejean C. Associations between transition to retirement and changes in dietary intakes in French adults (NutriNet-Sante cohort study). Int J Behav Nutr Phys Act 2017;14:71.


24. Ali-Kovero K, Pietilainen O, Mauramo E, Jappinen S, Rahkonen O, Lallukka T, et al. Changes in fruit, vegetable and fish consumption after statutory retirement: a prospective cohort study. Br J Nutr 2020;123:1390-5.


- TOOLS







