|
 |
- Search
| Korean J Fam Med > Volume 44(3); 2023 > Article |
|
Abstract
Background
This study explored the psychosocial needs of family caregivers of persons with spinal cord injuries from the perspective of rehabilitation professionals.
Methods
An exploratory qualitative approach was used, and a total of 14 rehabilitation professionals from various backgrounds participated in face-to-face interviews. All interviews were audio recorded, and session notes were added to the existing data and later transcribed. Thematic analysis was used to identify key themes.
Results
Nine need themes emerged: informational, psychological, personal care, financial, social support, welfare, vocational, telemedicine, and referral.
Conclusion
The findings of this study will aid the design or development of need-based customized psychosocial interventions for family caregivers of persons with spinal cord injuries in India. Multiple stakeholders involved in spinal cord injury management should understand the importance of meeting the needs of family caregivers of persons with spinal cord injuries and the timely delivery of customized psychosocial interventions.
Spinal cord injury (SCI), a suddenly debilitating neurological disorder, significantly impacts the physical, psychological, social, and occupational well-being of the affected [1,2]. The persons with SCI (PwSCI) and their parents, spouses, children, and siblings are changed by SCI [3]. In India, the prevalence of SCI is 236 per million, with an annual incidence of 1,520 per million [4]. Nearly 1.5 million persons in India have SCI, with 20,000 new cases diagnosed yearly. The majority (60%–70%) of patients are illiterate, poor peasants, and males aged 16–30 years, indicating a higher rate among young people [5]. In a country like India, family is a crucial support system for affected individuals, and family members do whatever they can to help PwSCI recover. However, adapting approaches vary among families [6]. Family caregivers (FCGs) play an important role in the recovery of patients with PwSCI, and the quality of care they provide is equal to or better than expert care [7]. Caregiving in PwSCI requires substantial adjustment for FCGs, impacting their interpersonal relationships, societal roles, community and leisure activities, vocational functioning, psychological well-being, and health-related quality of life [8].
Providing care for PwSCI differs from that for people with other illnesses and injuries because of the unique challenges associated with SCI, such as bladder, bowel, pressure, and ulcer management [9], as well as the extended period of caregiving [10]. According to research studies conducted worldwide, FCGs of PwSCI experience isolation [11], burden [12], poor leisure satisfaction [13], a reduced capacity to find and keep work [14], and marital disturbances [15]. Therefore, it is imperative to acknowledge the tremendous efforts of FCGs in the PwSCI recovery and meet their unmet needs. Understanding the exclusive psychosocial requirements of FCGs will aid the development and delivery of customized interventions.
There is an amplified need for qualitative research that explores the needs of FCGs of PwSCI. Due to the unpredictable nature of SCI, some family members find themselves in unprecedented roles as FCGs [16]. There is a lack of knowledge about the emotional and practical issues that FCGs encounter in India [17]. Recognizing service delivery gaps and offering need-based psychological interventions is a pressing requirement across the country [18]. However, there is a paucity of research on how PwSCI and their FCGs adjust to new lifestyles following an accident or how dyadic coping mechanisms are used to maintain relationships. Moreover, unmet requirements of caregivers may limit appropriate care and seem to have a detrimental impact on the health of caregivers and recipients. Unmet needs cause FCGs to devote extra time to themselves [7]. Previous research findings from Western countries cannot be generalized considering the differences in the Indian sociocultural backdrop context. There is limited research on the psychosocial needs of FCGs in the Indian context. Hence, with this background, the current study aimed to understand better the needs of FCGs from a professional perspective.
This study adopted a qualitative method to effectively examine the study variables. This approach was used because it strengthens the identification and exploration of the study variables through the participants’ experiences [19]. In India, the specific requirements and experiences of FCGs have not yet been studied from the perspectives of experts. Hence, we used an exploratory qualitative approach and indepth face-to-face interviews to assemble the data.
This study was conducted at the Department of Neurological Rehabilitation, a tertiary care center in South India. A predefined number of 14 experts from seven different professional backgrounds were chosen as participants. The inclusion criteria were: experts working with PwSCI such as, neurophysicians, occupational therapists, physiotherapists, medical and psychiatric social workers, neuropsychologists, nurses, non-government organizations (NGOs); a minimum of 5 years of experience working in the same field; ability to speak English; and willingness to provide informed consent to participate. The exclusion criteria were as follows: unwillingness to participate. The study was conducted from June to September 2021.
The researchers developed a semi-structured questionnaire to capture the sociodemographic details of the experts, such as educational qualifications, specialty, years of experience, and department of affiliation.
The researchers developed an interview guide (IG) to collect data on the concerns and needs of FCGs of PwSCI. The IG was tested for face and content validation. The updated IG after face validation was provided to professionals for content validation. The IG was finalized in consultation with 14 professionals who worked with PwSCI and their FCGs. None of these 14 experts were included in this study. The samples were chosen based on their previous expertise working with PwSCI and their FCGs, and each provided insight into qualitative research approaches. The IG contents are listed in Table 1.
Face-to-face, in-depth interviews of experts who met the inclusion criteria were conducted. The researcher started the interview using the above IG contents wherever required and used appropriate probes to assist with the collection of the required information (Table 2). Each interview lasted for approximately 45–60 minutes.
This study is the first phase of an ongoing Ph.D. research project entitled “Well-being program for caregivers of persons with spinal cord injury: a feasibility study.” Ethical clearance was obtained from the Institute of Human Behavioral and Ethics Committee of the National Institute of Mental Health and Neuro-Sciences (No. NIMH/DO/BEH. Sc.Div./2020-21). The participants were informed of the research and its procedures before providing written informed consent.
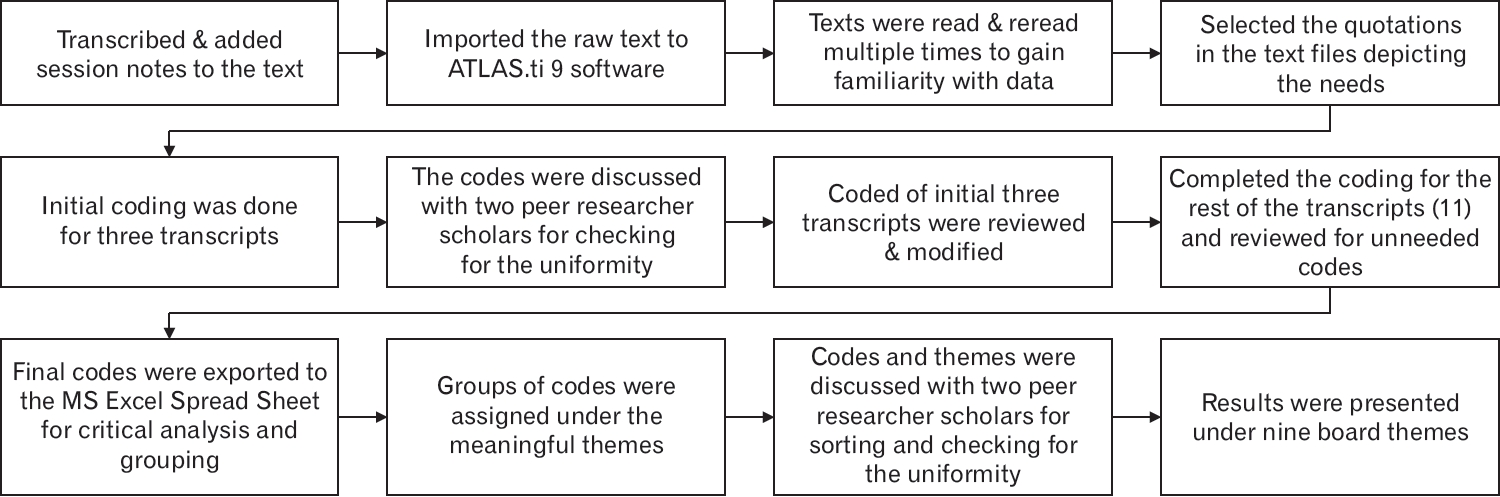
All interviews were recorded, and session notes were added to the existing data. The transcripts were imported and coded using Atlas.ti (ATLAS.ti 9 Desktop Trial; https://atlasti.com/free-trial-version/). To familiarize themselves with the data, the raw texts were read and reread several times. The text parts that represented FCG needs were examined and evaluated during the coding process, and an additional code was created. Two peer research scholars who were not part of this research maintained data uniformity and sorted out the codes after a detailed discussion of the emerging codes and themes. Based on the primary coding findings, the researcher coded the remaining data. To generate new meaningful codes and reduce unnecessary codes, the researcher reviewed the complete dataset. After exporting the scripts to a Microsoft Excel file, they were thoroughly evaluated, and the themes were correctly labeled. Subsequently, the developed codes were assigned to the relevant topics. Again, these codes were discussed with two peer researchers to ensure that the codes and assigned themes were consistent. Subsequently, these adjustments are discussed and defined. The data were analyzed for each of the 14 interviews. The findings were organized according to the nine needs that emerged from the codes. The entire data analysis process is illustrated in Figure 1.
The sociodemographic characteristics of the 14 experts who participated in the study are presented in Table 2.
Psychosocial needs were arranged under relevant themes as a result of the qualitative research data analysis, which yielded nine themes (Table 3). Below is a full description of each code under several themes as well as expert quotes.
All the experts emphasized the importance of informational needs and expressed that FCGs should know about all the components of the neurological condition, such as the injury nature, type, and cause and patient symptoms, management, prognosis, and recovery. Considering the unique nature of symptoms in SCI, experts have stressed the need for techniques for managing symptoms such as bowel incontinence, bladder incontinence, and pressure ulcers. The additional needs are mentioned in Table 2. The experts articulated the requirements for information, as described below.
“We should inform caregivers about techniques for managing symptoms such as bowel incontinence, bladder incontinence, and pressure ulcer; otherwise, in the long run, these complications will impact the recovery and rehabilitation outcomes, thereby increasing the caregiver burden.” (Dr. N, neurophysician)
“The first question the CGs propose is, ‘When will my loved one start walking?’ It is important to educate the family caregivers about their loved ones’ neurological conditions, especially the prognosis and recovery phase, to help them have realistic expectations and plan accordingly.” (Mr. T, physiotherapist)
Most experts have stated that, while providing care for the PwSCI, FCGs often ignore their own mental health needs. (This may also be due to a lack of personal time.) Experts have identified various psychological needs for FCGs, such as acknowledging their feelings, problemsolving abilities, stress management techniques, positive coping strategies, and emotional regulation. The following quotes statement characterizes the psychological needs of FCGs.
“Many times, the CGs of PwSCI lack time to process their own emotions with others, as they must be with the PwSCI at all times. Thus, they are unable to even think about their needs and unknowingly put their mental health at risk.” (Ms. V, neuropsychologist)
“The CGs of PwSCI must learn healthy coping strategies for managing their ongoing psychosocial issues in routine life; otherwise, it would lead to significant financial and emotional constraints for their families.” (Ms. P, nurse)
Unlike in other illnesses, FCGs are unusually attached to PwSCI. Hence, FCGs often lack time to perform their daily activities or routines. Some experts have given their input to magnify the importance of the FCGs’ personal care needs, such as normalizing the daily routine (diet, sleep hygiene, leisure); role-sharing and responsibilities; managing marital, sexual, and interpersonal issues; and seeking help to make time for recreational and spiritual activities. Experts have been attentive to role-sharing and help-seeking behavior needs. The following quotes exemplify some of these themes.
“The CGs of PwSCI must think about their care and focus on normalizing their daily routines. To care for the PwSCI, the CGs must also manage their physical and mental health. Otherwise, it will bounce back to the CGs, in turn increasing their burden.” (Dr. B, psychiatric social worker)
“I have seen many CGs in the community provide endless care to the PwSCI to prevent them from experiencing loneliness. We should educate them on role-sharing and help-seeking behavior. This will relieve the primary CGs and allow the other family members to learn and share the caregiving responsibilities.” (Dr. K, non-governmental organization)
Considering the etiology and clinical picture of SCI, direct and indirect treatment costs are high. In a developing country like India, many PwSCI have low socioeconomic backgrounds; hence, they cannot afford treatment and find it difficult to meet the subsequent associated costs. Some experts have stated several financial needs, such as financial support for buying medicines, meeting household expenditures, providing education for children, and availing resources for financial support. The following quotes illustrate some of these themes.
“As known, SCI is a chronic illness, and CGs must spend money on medication, frequent hospital visits, and clean intermittent catheterization materials, which can constitute a huge burden for them.” (Mrs. P, nurse)
“Many PwSCI were the breadwinners of the family; hence, after the injury, everything turned upside down. The female CGs (their spouses) reported the difficulty they encounter in meeting the financial expenses associated with running the family and continuing their children’s education.” (Mr. K, non-governmental organization)
Few experts have expressed social support needs, such as establishment of rehabilitation centers, peer support groups, respite care centers, significance of social participation, and secondary family support for caregiving, which can intensify the role of support for the FCGs. Empowering the CGs about peer support groups was highlighted in the interviews. The quotes below portray social support needs.
“Neurological rehabilitation centers are lacking in India. We must ensure their effective functioning and sustainable planning for services for the poor.” (Mr. K, non-governmental organization)
“We must empower CGs with respite care services and the ability to seek support from extended family members and society to reduce their burden. Many CGs have inadequate time to participate in various social gatherings; thus, we must educate them and others about the importance of community participation.” (Mr. A, psychiatric social worker)
Experts have stressed the importance of welfare needs such as unique disability identity (UDID) registration and certification, disability welfare benefits, rights of persons with disabilities, and government schemes. The following quotes explain some of these themes.
“It is our responsibility to make CGs aware of the UDID card, its benefits, and how best they can utilize the benefits. The pension amount can help families address their financial constraints.” (Mr. A, psychiatric social worker)
“All persons with a disability (PwD) and their CGs should know about the rights of the PwD, particularly supported education, supported employment, and concepts of the Rights of PwD Act.” (Mr. K, non-governmental organization)
The experts were more expressive and concerned about the vocational needs of the FCGs of PwSCI. They reported how the injury would affect the vocational components of PwSCI and FCGs. Some experts stated that the FCGs would need help obtaining jobs, starting self-employment, and continuing their education or jobs. The following quotes exemplify some of these themes.
“As many of the PwSCI are young males and their spouses must remain with them at home, we must educate them on the self-employment options available. This can enable the CGs to earn money to run the family and simultaneously care for the PwSCI.” (Mr. R, non-governmental organization)
“A job is a primary need for the economic stability of the PwSCI and their CGs. Hence, we must inform them about government and non-government vocational training centers in their areas.” (Mr. B, psychiatric social worker)
Some experts have stated the significance of telemedicine needs for PwSCI and their FCGs, such as regular follow-ups, ordering prescriptions, inquiring, and performing exercises over video calls. One of the vital comments from these needs was initiating telemedicine services for follow-up services for PwSCI due to coronavirus pandemic restrictions and to reduce indirect treatment costs. The following quotes demonstrate some of these themes.
“Traveling from far distances for follow-ups is very difficult for the PwSCI and their CGs. We should initiate telemedicine services to reduce their travel difficulties and treatment costs.” (Dr. N, physical medicine and rehabilitation)
“In collaboration with the telemedicine department, rehabilitation therapists should provide physiotherapy and occupational services for the PwSCI. We must initiate these services to increase awareness and ensure effective care for PwSCI.” (Ms. A, occupational therapist)
In this study, experts highlighted the importance of referral needs for FCGs, which play a significant role in the outcomes of PwSCI recovery. Continued exercise and regular treatment adherence are key factors for better recovery from SCI. Hence the FCGs should be aware of the therapy centers and hospitals in their areas. FCGs must learn about trauma care centers, occupational and physiotherapy centers, and local NGOs. The following quotes represent some of these themes.
“We all know the importance of continuation of exercises after rehabilitation center discharge. Hence, the PwSCI and their CGs must know about the physiotherapy and occupational therapy centers in their areas to prevent treatment lapses and not increase CG burden.” (Mr. T, occupational therapist)
“We must inform CGs about the local NGOs and their services so they can seek support from the community whenever they are in need, thereby enhancing their social support, which is important.” (Mr. A, psychiatric social worker)
This study highlighted the psychosocial needs of the FCGs of PwSCI in India. Nine need themes emerged from the qualitative analysis: information, psychological, personal care, financial, social support, welfare, vocational, telemedicine, and referral.
We must understand the bidirectional relationship between the FCG and most psychosocial issues arising from the health condition of PwSCI. These are not separate entities, as each impacts the other. The complexity of providing care for PwSCI is individualistic and contextual in nature. Hence, special attention is required to capture the requirements of FCGs. Multiple stakeholders must consider the needs of PwSCI and their FCGs, such as experts involved in SCI management and NGOs. Moreno et al. [20] highlighted an integrative approach to SCI needs by including different stakeholders such as PwSCI, their FCGs, and healthcare professionals in a scoping study protocol.
To our knowledge, the current qualitative study is the first in India to explore the psychosocial needs of FCGs of PwSCI. The present study highlights the significance of the interplay of different factors, such as personal, emotional, social, vocational, health service, and environmental factors, related to the psychosocial needs of FCGs for PwSCI. It is imperative to understand the roles of these factors to provide active support mechanisms for psychosocial interventions for the FCGs of PwSCI. Experts involved in SCI management play a crucial role in achieving rehabilitation goals. Experts play an essential role in eliciting the psychosocial needs of FCGs and PwSCI. They can anticipate psychosocial issues in the FCGs of PwSCI patients at different periods, such as during rehabilitation and after discharge. A Switzerland-based qualitative study reported the same from experts’ observations and their professional roles with adequate knowledge about psychosocial issues [21].
We must understand the impact of unfulfilled psychosocial needs associated with a decreased quality of life [22] and increased caregiving burden [7]. A comparison of the findings of previous studies with the current study reveals the most significant information needs. A preliminary study from the United States consisting of 17 FCGs of PwSCI stated health information needs as the most important [23]. The same study reported that the emotional needs of FCGs were often unmet, findings that are consistent with those of the current study. A recent qualitative study from Canada demonstrated the importance of educational training programs for PwSCI and their family members in building relationships post-injury [24].
Many interventional studies worldwide included psychoeducational interventions in their design to provide for the health information needs of PwSCI and their FCGs [25]. In line with the current study’s findfindings, a descriptive survey from Australia that included 179 FCGs of PwSCI concluded that informational, personal, and respite support are the most commonly reported service needs [26]. In the current study, some social science experts stated the need for FCG employment. An editorial from India mentioned the challenges of PwSCI and their FCGs at the community level and recommended addressing issues related to emotional, vocational, empowerment, and community-based rehabilitation [27].
Experts have reported on telemedicine needs, considering the coronavirus disease 2019 pandemic, and stressed the significance of telemedicine services to ensure follow-up. Experts also stated the importance of telemedicine for decreasing treatment costs and increasing the quality of life [28]. The experts in this study identified the telemedicine needs for the benefit of FCGs based on their observations and suggestions from the CG, such as ensuring regular follow-up, supervising the PwSCI’s exercises, conducting therapy sessions, clarifying doubts, developing realistic expectations of the PwSCI, and obtaining online prescriptions. It is a well-documented fact that FCGs of PwSCI have poor mental health outcomes, such as depression, anxiety, loss of identity, isolation, and reduced satisfaction. A literature review from Ireland concluded that providing interventions, such as problem-solving skills, support groups, and family training to the FCGs of PwSCI is the need of the hour, consistent with the current study’s findings [29].
The need for referrals identified in this research is similar to previous studies across global perspectives of the special attention rendered to referral services related to the management of clinical symptoms and secondary complications associated with SCI [30]. However, the experts in this study mentioned various referral services, such as hospitals, local NGOs, Jan Aushadhi medical centers, district differently abled welfare officers, local administrators, paid caregiver services, trauma care/neurology centers, occupational centers, and physiotherapy centers. Some experts stressed the importance of peer support groups in the current study, which identified some unique needs such as psychoeducation, teaching problem-solving skills, coping skills, and telemedicine services as recommended by previously published research studies. Informational needs are the most commonly reported needs in studies worldwide. In this study, almost all experts stressed the importance of informational needs.
However, considering the sociocultural background of Indian caregivers, experts have reported some unique needs. The most dominant needs were informational, psychological, personal care, and financial.
The current study had some limitations, including its small sample size and convenience sampling design. Data triangulation was performed to enrich the findings from other perspectives. The study’s findings cannot be generalized because of the small sample size. Despite these limitations, this study had several strengths. To the best of our knowledge, it is the first study to examine the psychosocial needs of Indian FCGs of PwSCI among participants from various professional backgrounds. Face-to-face interviews were conducted to assess the needs of the FCGs. This study provided an abundant amount of experience from experts managing SCI.
The viewpoints and experiences of the experts suggest the importance of developing interventions and providing services to FCGs of PwSCI. The current findings will be implemented in a management plan by a multidisciplinary team to offer a promising direction for intervention for FCGs. Developing customized interventions and testing them in controlled settings based on the psychosocial needs of FCGs is needed. Future research could adopt quantitative and qualitative methods in a large sample size to substantiate these findings. As per experts’ perspectives, policy-level interventions would then be initiated to meet some of the needs of the FCGs.
The FCGs of PwSCI in India have inimitable needs compared to those of Western FCGs. When these needs are unmet, unfavorable recovery outcomes for PwSCI and psychosocial outcomes for both PwSCI and the FCGs of PwSCI occur. The findings of this research will aid the design and development of need-based, customized psychosocial interventions for the FCGs of PwSCI in India. Multiple stakeholders involved in the management of SCI stressed the importance of meeting the needs of FCGs of PwSCI and the timely delivery of customized psychosocial interventions.
ACKNOWLEDGMENTS
The authors express their gratitude to the professionals who contributed to this research.
Table 1.
Interview guide contents and probes
Table 2.
Experts’ sociodemographic characteristics
Table 3.
Psychosocial needs of the FCGs of PwSCI
REFERENCES
1. Dumont RJ, Okonkwo DO, Verma S, Hurlbert RJ, Boulos PT, Ellegala DB, et al. Acute spinal cord injury, part I: pathophysiologic mechanisms. Clin Neuropharmacol 2001;24:254-64.


2. Ahuja CS, Wilson JR, Nori S, Kotter MR, Druschel C, Curt A, et al. Traumatic spinal cord injury. Nat Rev Dis Primers 2017;3:17018.



3. Lude P, Kennedy P, Elfstrom ML, Ballert CS. Quality of life in and after spinal cord injury rehabilitation: a longitudinal multicenter study. Top Spinal Cord Inj Rehabil 2014;20:197-207.



4. Srivastava RN, Singh A, Garg RK, Agarwal A, Raj S. Epidemiology of traumatic spinal cord injury: a SAARC perspective. Int J Mol Biol Biochem 2015;3:9-22.
5. Singh R. Epidemiology of spinal cord injuries: Indian perspectives. Epidemiol Spinal Cord Inj 2012;157-68.
6. Simpson G, Jones K. How important is resilience among family members supporting relatives with traumatic brain injury or spinal cord injury? Clin Rehabil 2013;27:367-77.



7. Smith EM, Boucher N, Miller WC. Caregiving services in spinal cord injury: a systematic review of the literature. Spinal Cord 2016;54:562-9.



8. Middleton JW, Simpson GK, De Wolf A, Quirk R, Descallar J, Cameron ID. Psychological distress, quality of life, and burden in caregivers during community reintegration after spinal cord injury. Arch Phys Med Rehabil 2014;95:1312-9.


9. Nogueira PC, Rabeh SA, Caliri MH, Dantas RA, Haas VJ. Burden of care and its impact on health-related quality of life of caregivers of individuals with spinal cord injury. Rev Lat Am Enfermagem 2012;20:1048-56.


10. Schulz R, Czaja SJ, Lustig A, Zdaniuk B, Martire LM, Perdomo D. Improving the quality of life of caregivers of persons with spinal cord injury: a randomized controlled trial. Rehabil Psychol 2009;54:1-15.



11. Guilcher SJ, Craven BC, Lemieux-Charles L, Casciaro T, McColl MA, Jaglal SB. Secondary health conditions and spinal cord injury: an uphill battle in the journey of care. Disabil Rehabil 2013;35:894-906.



12. Khazaeipour Z, Ahmadipour E, Rahimi-Movaghar V, Ahmadipour F, Vaccaro AR, Babakhani B. Association of pain, social support and socioeconomic indicators in patients with spinal cord injury in Iran. Spinal Cord 2017;55:180-6.



13. Raj JT, Manigandan C, Jacob KS. Leisure satisfaction and psychiatric morbidity among informal carers of people with spinal cord injury. Spinal Cord 2006;44:676-9.



14. Ellenbogen PS, Meade MA, Jackson MN, Barrett K. The impact of spinal cord injury on the employment of family caregivers. J Vocat Rehabil 2006;25:35-44.
15. Dickson A, O’Brien G, Ward R, Flowers P, Allan D, O’Carroll R. Adjustment and coping in spousal caregivers following a traumatic spinal cord injury: an interpretative phenomenological analysis. J Health Psychol 2012;17:247-57.



16. Dickson A, O’Brien G, Ward R, Allan D, O’Carroll R. The impact of assuming the primary caregiver role following traumatic spinal cord injury: an interpretative phenomenological analysis of the spouse’s experience. Psychol Health 2010;25:1101-20.


17. Murthy RS. Caregiving and caregivers: challenges and opportunities in India. Indian J Soc Psychiatry 2016;32:10-8.

18. Kenny C, Sarma KM, Egan J. An interpretive phenomenological account of the experiences of family carers of the elderly. Irish J Psychol 2012;33:199-214.

19. Yilmaz K. Comparison of quantitative and qualitative research traditions: epistemological, theoretical, and methodological differences. Eur J Educ 2013;48:311-25.

20. Moreno A, Zidarov D, Raju C, Boruff J, Ahmed S. Integrating the perspectives of individuals with spinal cord injuries, their family caregivers and healthcare professionals from the time of rehabilitation admission to community reintegration: protocol for a scoping study on SCI needs. BMJ Open 2017;7:e014331.



21. Trezzini B, Phillips B. Impact of legal regulations and administrative policies on persons with SCI: identifying potential research priorities through expert interviews. Disabil Rehabil 2014;36:1883-91.


22. Sweet SN, Noreau L, Leblond J, Dumont FS. Understanding quality of life in adults with spinal cord injury via SCI-related needs and secondary complications. Top Spinal Cord Inj Rehabil 2014;20:321-8.



23. Meade MA, Taylor LA, Kreutzer JS, Marwitz JH, Thomas V. A preliminary study of acute family needs after spinal cord injury: analysis and implications. Rehabil Psychol 2004;49:150-5.

24. Jeyathevan G, Cameron JI, Craven BC, Munce SE, Jaglal SB. Re-building relationships after a spinal cord injury: experiences of family caregivers and care recipients. BMC Neurol 2019;19:117.




25. Dyck DG, Weeks DL, Smith CL, Shaw M. Multiple family group intervention for spinal cord injury: quantitative and qualitative comparison with standard education. J Spinal Cord Med 2021;44:572-82.


26. Foster M, Amsters D, Carlson G. Spinal cord injury and family caregivers: a description of care and perception of service need. Aust J Prim Health 2005;11:91-101.

27. Chhabra HS, Batra S. Spinal cord injury and its impact on the patient, family, and the society. Int J Recent Surg Med Sci 2016;2:1-4.

28. Tyagi N, Amar Goel S, Alexander M. Improving quality of life after spinal cord injury in India with telehealth. Spinal Cord Ser Cases 2019;5:70.