|
 |
- Search
| Korean J Fam Med > Volume 44(5); 2023 > Article |
|
Abstract
Post-traumatic fibro-osseous lesions (PTFOL) are a rare and benign tumor that typically affects the ribs and is probably caused by an excessive post-traumatic reactive process. PTFOL primarily affects the sixth, seventh, and eighth ribs. Here, we report a case of a PTFOL with an unusual location and expansion that simulated a malignant chest tumor. A 28-year-old male patient with a history of minor chest trauma presented with pain. Chest radiography revealed a large, well-defined lesion on the left fourth rib, and computed tomography (CT) of the chest revealed a lytic lesion-type IC on the posterior and middle arches of the left fourth rib with a cartilaginous matrix and discontinued periosteal reaction without soft tissue mass extension. Additionally, magnetic resonance imaging of the chest revealed an ovoid, expansive mass with cystic lobules and lobulated contours extending almost over the entire left fourth rib, measuring 134×47 mm in size. This mass has a low signal on T1-weighted images and a heterogeneous intermediate signal on T2-weighted images, with intense enhancement after gadolinium injection suggestive of a malignant chest tumor. A CT-guided bone biopsy confirmed the presence of an intramedullary lesion consisting of fibrous connective tissue with fusiform fibroblastic cells without atypical signs. The lesion was delimited by bone trabeculae with nibbled edges, indicating exaggerated osteoclastic activity compatible with a diagnosis of PTFOL. The patient was treated with simple analgesics, and chest pain was relieved, with an unchanged volume of the lesion at 1 year of follow-up.
Post-traumatic fibro-osseous lesions (PTFOL) are benign tumors that are often misdiagnosed as rib metastases, osteoid osteomas, fibrous dysplasias, or benign fibrous histiocytomas [1-3]. It is a rare lesion that typically affects the ribs, primarily the sixth, seventh, and eighth ribs [1], and is probably caused by an excessive post-traumatic reactive process [4]. To our knowledge, the involvement of the first four ribs has not yet been reported.
Various names have been used to describe this rare entity, such as traumatic dysplasia, post-traumatic symmetrical fibro-osseous dysplasia, symmetrical fibro-osseous dysplasia of the rib, sclerosing xanthoma, or pseudotumor focal Erdheim-Chester disease [2,4-6].
The diagnosis of PTFOL is rarely made through imaging techniques alone, and histopathological examination is necessary to confirm its diagnosis, particularly in cases of suspected lesions. For treatment, some studies suggest a simple follow-up, while others indicate chest wall resection of the lesion [3,4]. To avoid unnecessary surgery, PTFOL should be suspected during imaging procedures after eliminating differential diagnoses.
We report the case of a rare and unrecognized osseous lesion with an unusual location and expansion simulating a malignant chest wall tumor in a young male who presented with chest pain.
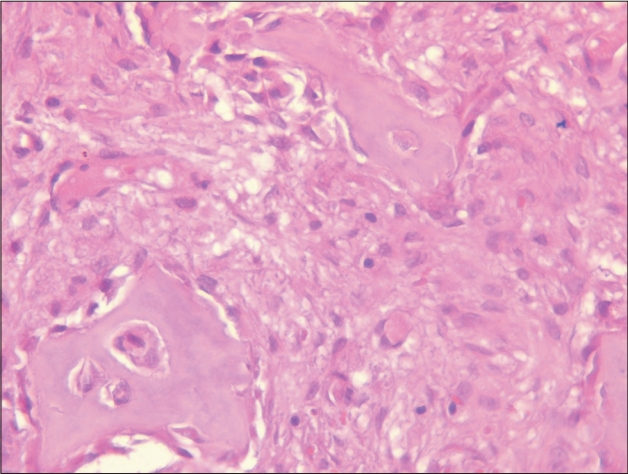
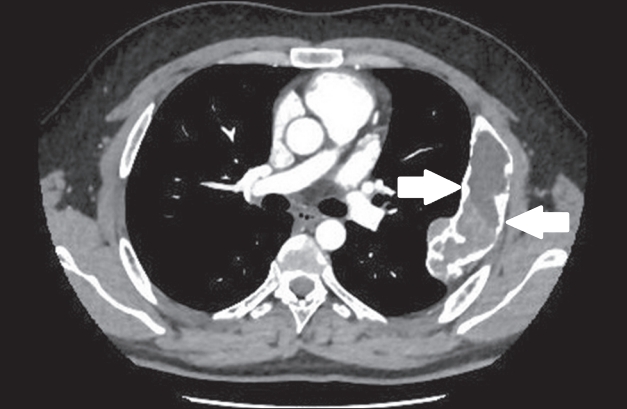
A 28-year-old male patient with a history of minor chest trauma before 5 years presented to the cardiology department with chest pain. A physical examination revealed no abnormalities. Electrocardiographic and echocardiographic findings were normal. Chest radiography revealed a large, well-defined lesion on the left fourth rib (Figure 1). Computed tomography (CT) revealed a lytic lesion-type IC of the posterior and middle arches of the left fourth rib with a cartilaginous matrix and a discontinued periosteal reaction without soft tissue mass extension (Figure 2). Laboratory investigations were within normal ranges, with an erythrocyte sedimentation rate of 13 mm in the first hour, a C-reactive protein concentration of 1.3 mg/L, and a calcium level of 2.41 mmol/L. Faced with this atypical lesion that suggested a malignant tumor, we completed our investigation with magnetic resonance imaging (MRI) of the chest, which showed an ovoid, expansive mass with a lobulated contour extending over almost the entire left fourth rib. This lesion had a low signal on T1-weighted images and a heterogeneous intermediate signal on T2-weighted images (clearly enhanced after gadolinium injection), all with cystic lobules. The lesion measured approximately 134×47 mm and was responsible for the cortical swelling without soft tissue invasion (Figure 3). These findings initially indicated an expansive tumor, such as chondrosarcoma, Ewing sarcoma, or especially an Askin tumor. A CT-guided bone biopsy revealed an intramedullary lesion consisting of fibrous connective tissue with fusiform fibroblasts without atypical signs. The lesion encompassed multiple osteoid trabeculae with a metaplastic appearance, surrounded by osteoblasts. The lesion was delimited by bone trabeculae with nibbled edges, indicating exaggerated osteoclastic activity (Figure 4). These histopathological findings confirmed a diagnosis of PTFOL. A simple follow-up was recommended, and the patient was treated with simple analgesics, and chest pain was relieved. Chest X-ray control showed an unchanged volume of the lesion at 1 year of follow-up.
The patient provided informed written consent for publication of the research details and images.
PTFOL is a rare, benign tumor that is often unrecognized and misdiagnosed as fibrous dysplasia, osteoid osteoma, or other benign tumors. Only a few cases have been reported in the literature, and in most cases, the diagnosis was retained after chest wall resection. Therefore, it is important to recognize this rare entity to avoid unnecessary surgical procedures and their complications. In this context, we report the case of a 28-year-old male patient who presented with an expansive lesion of the rib; the diagnosis of PTFOL of the fourth rib was confirmed with a CT-guided bone biopsy. The treatment consisted of a simple follow-up.
The reported age range at diagnosis of PTFOL is 14–79 years, with a mean age of 51 years [3,4]. The incidence is probably underestimated because the lesion is often misdiagnosed as other more common lesion of the ribs [4]. Classically, only one rib is affected; however, the lesion could be polyostotic and involve more than one rib, or in rare instances affect other bones such as the scapula, which has only been reported in two patients [2,7]. In most patients, the lesion affected only the posterior and lateral portions of the ribs [3,4]. However, in this patient, the lesion involved the entire fourth rib. Previous studies have reported smaller lesions measuring less than 3.5 cm in size [1], whereas in our study the volume was significantly higher, measuring 13.4×4.7 cm.
A history of trauma was reported in our patient and in most patients with PTFOL; for example, a study by McDermott et al. [3] reported a history of trauma in seven patients from a total of 11 patients with PTFOL, with a delay between lesion discovery and the traumatic episode being variable between 2 and 42 years in the same study. Chest trauma is usually minor and subclinical, as was the case in our patient. The pathogenesis of PTFOL remains unclear till date, and PTFOL is thought to be a reactive process rather than a bone tumor. The endosteal blood supply, provided by the posterior intercostal artery, is distinct from the periosteal blood supply, which is supported by the anterior intercostal artery in the ribs. As a result, incomplete or abnormal resorption of focal endosteal osteonecrosis can lead to the development of PTFOL. This phenomenon could potentially clarify the accumulation of foamy histiocytes, the fibroblastic background of these lesions, and their association with trauma [1].
Although PTFOL is usually described as a fortuitous discovery, it can be symptomatic [4]. In our patient, the lesion was discovered during an investigation for moderate chest pain related to the lesion. The diagnosis can be made using chest radiography, but it is also often discovered through chest CT scans or chest MRIs. The typical radiological feature of PTFOL is an ovoid or fusiform central radiolucency with a sclerotic rim. In contrast, the radiographic findings of our patient showed that the lesion had a cartilaginous matrix, and the periosteal reaction was discontinued. However, in some patients, the lesion has been reported to be radio-dense [3,7].
Open surgical biopsy remains the gold standard for histological analysis, and to obtain a definitive diagnosis, percutaneous imageguided needle biopsy is now the best technique; however, it requires an experienced radiologist [1]. Despite excellent diagnostic performance and lower complication rates compared to surgical biopsy, percutaneous rib biopsy is more difficult in this location and represents a real technical challenge [8], which was the method used in our patient to confirm the diagnosis of PTFOL. Of the 11 patients included in the study by McDermott et al. [3], only one was diagnosed using a needle biopsy; an open surgical biopsy was performed for the rest.
The main differential diagnosis of PTFOL is fibrous dysplasia, which is the most common benign lesion of the ribs. The distinction can be made based on some key differences, such as the random appearance of the woven bone embedded in a delicate fibrous stroma, thinner and more irregularly shaped trabeculae, and the absence of lamellar bone maturation [4]. This distinction is of high importance because the diagnosis of fibrous dysplasia implies a long clinical follow-up because of the minimal risk of sarcomatous transformation.
The second differential diagnosis of PTFOL is osteoid osteoma, which differs from PTFOL by a greater degree of stromal vascularity, the absence of a zonal pattern of osteoid and bone trabeculae, and numerous plump osteoblasts [3,4]. In contrast, the large volume and expansion of the lesion in our patient suggested a malignant chest tumor.
For treatment, chest wall resection with or without reconstruction remains the gold standard, and some studies have suggested a simple clinical and radiological follow-up for solitary and asymptomatic lesions of the ribs [1]. Despite improvements in surgical procedures and the use of newer reconstruction materials to minimize perioperative morbidity, this surgical procedure is still associated with high morbidity rates [9]. The most frequent complications were respiratory problems such as abscess, infection, pneumonia, and pleural effusion, which were reported in the literature in approximately 24% of patients who underwent chest wall resection [10].
In a study by Kandel et al. [6], one of the two reported patients died from pulmonary embolism 1 week after resection. Two of the seven patients reported in a study by Aubert et al. [4] presented with local complications after chest wall resection, along with respiratory complications (pleural effusion and pulmonary hernia).
In our study, we chose a simple follow-up, and the radiological control showed an unchanged lesion at 1 year of follow-up.
In conclusion, we report a rare case of PTFOL in an unusual location in the fourth rib, unusual volume and expansion covering the entire rib, a noninvasive modality of diagnosis using percutaneous CT scan-guided biopsy, and a nonconventional type of management based on simple follow-up treatment. Therefore, it is highly important to recognize this rare and benign entity and differentiate it from other rib tumors to avoid unnecessary extensive resection and long-term follow-up.
Figure. 1.
A chest radiograph showing a large and well-defined lesion in the left fourth rib (arrow).
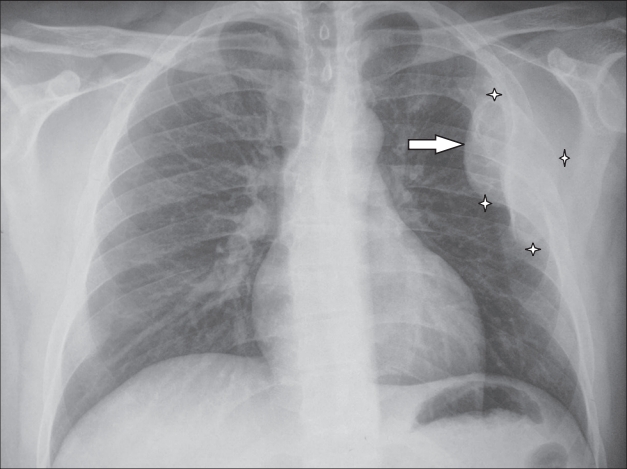
Figure. 2.
Computed tomography of the chest showing a lytic lesion type IC of the posterior and middle arch of the left fourth rib with a cartilaginous matrix and discontinued periosteal reaction (arrows).
REFERENCES
1. Nassereddine H, Larousserie F, Campagna R, Castier Y, Couvelard A, Choudat L, et al. Xanthomatous posttraumatic fibro-osseous lesion of the rib: a rare and underrecognized entity. case report and literature review. Int J Surg Pathol 2017;25:640-3.



2. Blanco M, Cabello-Inchausti B, Cura M, Fernandes L. Post-traumatic fibro-osseous lesion of the ribs and scapula (sclerosing xanthofibroma). Ann Diagn Pathol 2001;5:343-9.


3. McDermott MB, Kyriakos M, Flanagan FL. Posttraumatic fibro-osseous lesion of rib. Hum Pathol 1999;30:770-80.


4. Aubert S, Kerdraon O, Conti M, Buob D, Petit S, Leroy X. Post-traumatic fibro-osseous lesion of the ribs: a relatively under-recognised entity. J Clin Pathol 2006;59:635-8.



6. Kandel RA, Pritzker KP, Bedard YC. Symmetrical fibro-osseous dysplasia of rib: post-traumatic dysplasia? Histopathology 1981;5:651-8.


7. Kessler S, Mirra JM, Gordon P. Case report 823: fibro-osseous pseudotumor of the scapula. Skeletal Radiol 1994;23:73-7.

8. Jakanani GC, Saifuddin A. Percutaneous image-guided needle biopsy of rib lesions: a retrospective study of diagnostic outcome in 51 cases. Skeletal Radiol 2013;42:85-90.