INTRODUCTION
Amylase is an amylolytic digestive enzyme whose main function is to digest starch into smaller polysaccharides, finally producing monosaccharides. Serum amylase originates mostly from the pancreas and salivary glands; however, a small amount is released from other organs, such as the kidneys, liver, muscle, and fallopian tubes. The enzyme assumes two basic forms: P-type amylase secreted from the pancreas and S-type amylase secreted from the salivary glands. Amylase is cleared by the kidneys and the reticuloendothelial system; thus, it is associated with renal failure and liver disease [1].
Hyperamylasemia is a serum amylase level above the upper limit of normal (range, 30–110 U/L). An elevated serum amylase is observed in around 75% of cases of pancreatitis. However, acute pancreatitis usually presents with constitutional symptoms, such as nausea, vomiting, abdominal pain, hyperglycemia or hypocalcemia, and radiological changes in the pancreas [2]. Nevertheless, asymptomatic hyperamylasemia is usually observed with other systemic diseases such as tumors, mumps, or kidney failure, or with drug use [3].
CASE REPORT
A 43-year-old Jordanian man working in Saudi Arabia was diagnosed with hypertriglyceridemia in 2017 when he presented to a family medicine clinic for a routine physical examination. At that time, his lipid profile was abnormal as follows: total cholesterol, 243 mg/dL; triglyceride, 570 mg/dL; low-density lipoprotein, 71 mg/dL; and high-density lipoprotein, 32 mg/dL. He was started on fenofibrate 145 mg/d and provided lifestyle modification advice. He presented again to the family medicine clinic in October 2018 with a blood test report from his home country during holiday that showed elevated amylase enzyme levels.
It is well known that elevated triglyceride levels can cause acute pancreatitis; thus, every effort was made to rule out hypertriglyceridemia-induced pancreatitis. During that visit, the patient reported a 1-year history of symptoms of intermittent episodes of mild non-radiating epigastric pain associated with abdominal bloating and a change in bowel habits. He had not experienced nausea or vomiting, and his symptoms were not caused by specific types of foods. He had been a cigarette smoker for almost 10 years; however, he denied a history of drug or alcohol consumption. Moreover, he reported noncompliance with the prescribed fenofibrate regimen. His family history was significant for celiac disease (sister). Physical examination findings were normal.
1. Diagnostic Assessment
Complete blood count testing indicated mild leukocytosis, and liver and renal function test results were within the normal ranges. His lipid profile readings were as follows: total cholesterol, 300 mg/dL; triglyceride, 1,086 mg/dL; low-density lipoprotein, 50 mg/dL; and high-density lipoprotein, 30 mg/dL. The serum amylase level was 212 U/L, while the serum lipase level was within the normal range. Abdominal ultrasound revealed only fatty liver changes and a small left renal cyst. The patient was advised to take the fenofibrate as prescribed and proceed to the emergency room whenever he developed significant symptoms. He was also scheduled for a follow-up appointment for reassessment within the family medicine practice.
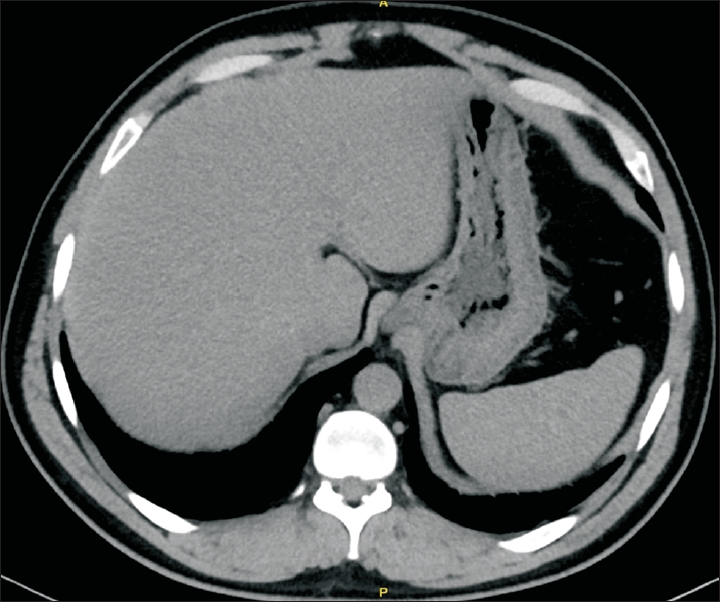
In December 2018, the patient presented for follow-up with symptoms of abdominal bloating in addition to infrequent attacks of diffuse abdominal pain. His amylase and triglyceride levels were 242 U/L and 271 mg/dL, respectively, and the rest of his blood tests were unremarkable. Subsequently, the patient was followed up every 3–6 months, during which time the serum triglyceride levels fluctuated between 90 and 460 mg/dL, whereas the serum amylase levels were between 212 U/L and 669 U/L and never returned to normal (Table 1). Anti-gliadin and anti-endomysial antibody tests were negative; thus, celiac disease was excluded. An abdominal computed tomography scan performed in November 2019 showed a normal pancreatic and hepatobiliary system (Figure 1). The patient was then referred to a gastroenterology clinic for further assessment. Findings of esophagogastroduodenoscopy and colonoscopy performed in January 2021 were normal. Serum and urinary amylase and creatinine were analyzed to calculate the amylase creatinine clearance ratio (ACCR) using the following formula: [urine amylase (U/L)×serum creatinine (mg/dL)]/[serum amylase (U/L)×urine creatinine (mg/dL)]×100. The normal ACCR is 3%–5%, while a result of <1% suggests macroamylasemia [4]. The test results were as follows: urine amylase, 238 U/L; serum creatinine, 0.71 mg/dL; serum amylase, 370 U/L; and urine creatinine, 293.42 mg/dL. The ACCR was calculated as 0.155%; thus, a diagnosis of macroamylasemia was established. The diagnosis was discussed with the patient, who was informed that no specific treatment is required for his condition.
Signed informed consent was obtained from the patient for the publication of his anonymized case-related information.
DISCUSSION
Macroamylasemia is a rare benign condition characterized by elevated serum amylase levels but normal urinary amylase levels and no other associated signs and symptoms. Macroamylase is a macromolecular complex consisting of amylase bound by immunoglobulin whose large size prevents kidney filtration. It usually causes hyperamylasemia with an ACCR of <1% [5]. The prevalence of macroamylasemia is around 1% in the general population and 2.5% among people with hyperamylasemia [6]. It is mostly found among men; however, some cases have been reported in children and newborns [7].
Macroamyalsemia is generally asymptomatic; in some cases, it may be detected incidentally during investigations of abdominal pain. However, this observation does not confirm the association between the two. Some authors suggest that the abdominal pain may be attributed to the deposition of macroamylase molecules in the pancreas [8]. The coexistence of macroamylasemia with multiple diseases such as ulcerative colitis, Crohn’s disease, hematologic malignancies, systemic lupus erythematosus, and rheumatoid arthritis has been reported [9]. Several studies have observed the association between macroamylasemia and celiac disease as well as the disappearance of macroamylasemia with a gluten-free diet [10].
In this case, macroamylasemia was not considered in the initial differential diagnosis due to its rarity, which led to an extensive investigation. Additionally, the coexistence of hypertriglyceridemia, which was initially uncontrolled, drew attention toward ruling out the diagnosis of acute pancreatitis. The risk of developing acute pancreatitis is approximately 5% with a triglyceride level >1,000 mg/dL [11]. Therefore, although macroamylasemia is a rare condition, it should be considered when elevated serum amylase levels are observed with normal serum lipase levels, urinary amylase levels, and renal function. The current findings demonstrate that ACCR is a feasible and cost-effective screening tool that can avoid unnecessary, expensive, and invasive tests and treatments.