|
 |
- Search
| Korean J Fam Med > Volume 45(1); 2024 > Article |
|
Abstract
Background
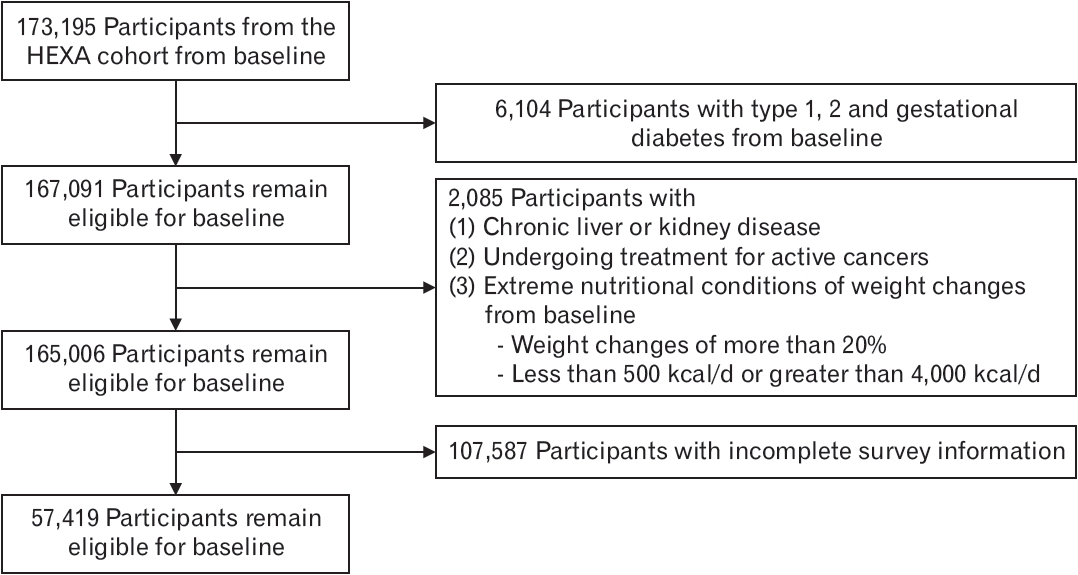
Methods
Results
Conclusion
ACKNOWLEDGMENTS
SUPPLEMENTARY MATERIALS
Supplement 1.
Supplement 6.
Figure. 2.
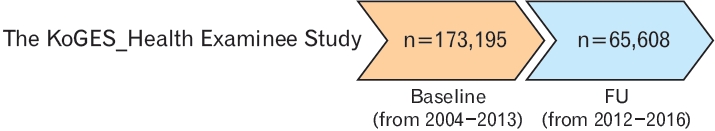
Table 1.
| Characteristic |
Fruits consumption in quartiles (servings/wk) |
P-value* | ||||
|---|---|---|---|---|---|---|
| 0–7.9 | 8–15.9 | 16–20.9 | ≥21 | |||
| No. of participants | 13,418 | 20,660 | 8,402 | 14,939 | ||
| Sex | <0.001 | |||||
| Female | 7,006 (52) | 13,680 (66) | 6,202 (74) | 11,603 (78) | ||
| Male | 6,412 (48) | 6,980 (34) | 2,200 (26) | 3,336 (22) | ||
| Age (y) | 53.54±8.32 | 53.41±8.09 | 53.20±7.76 | 53.00±7.53 | <0.001 | |
| Family history of diabetes | 2,681 (20) | 4,696 (23) | 1,950 (23) | 3,267 (22) | <0.001 | |
| Initial body mass index (kg/m2) | 23.90±2.97 | 23.82±2.86 | 23.73±2.79 | 23.62±2.76 | <0.001 | |
| Caloric intake per day (kcal) | 1,600.41±490.69 | 1,700.14±505.92 | 1,771.88±530.44 | 1,940.01±588.61 | <0.001 | |
| Initial moderate to vigorous exercise (min/wk) | <0.001 | |||||
| 1–120 | 3,664 (27) | 6,072 (29) | 2,577 (31) | 4,402 (29) | ||
| 121–180 | 1,005 (7.5) | 1,881 (9.1) | 826 (9.8) | 1,591 (11) | ||
| Greater than 180 | 1,958 (15) | 3,351 (16) | 1,454 (17) | 2,914 (20) | ||
| None | 6,791 (51) | 9,356 (45) | 3,545 (42) | 6,032 (40) | ||
| Initial smoking status | <0.001 | |||||
| Current smoker | 2,364 (18) | 2,019 (9.8) | 538 (6.4) | 837 (5.6) | ||
| Ex-smoker | 2,702 (20) | 3,191 (15) | 1,072 (13) | 1,613 (11) | ||
| Never-smoker | 8,352 (62) | 15,450 (75) | 6,792 (81) | 12,489 (84) | ||
| Initial drinking status | <0.001 | |||||
| Drinker | 7,153 (53) | 9,152 (44) | 3,350 (40) | 5,582 (37) | ||
| Non-drinker | 6,265 (47) | 11,508 (56) | 5,052 (60) | 9,357 (63) | ||
| Initial income (million KRW/mo) | <0.001 | |||||
| >4 | 4,949 (37) | 8,037 (39) | 3,247 (39) | 6,580 (44) | ||
| 2–4 | 2,539 (19) | 3,627 (18) | 1,348 (16) | 2,692 (18) | ||
| 1–1.99 | 2,871 (21) | 4,725 (23) | 2,211 (26) | 3,563 (24) | ||
| <1 | 3,059 (23) | 4,271 (21) | 1,596 (19) | 2,104 (14) | ||
Table 2.
| Items |
Unadjusted (N=57,419) |
Adjusted (N=57,419)* |
||
|---|---|---|---|---|
| HR† (95% CI) | P-value | HR† (95% CI) | P-value | |
| Fruit, total | 1.02 (0.99–1.06) | 0.2 | 1.02 (0.99–1.06) | 0.2 |
| Strawberries | 0.98 (0.92–1.05) | 0.6 | 0.98 (0.92–1.05) | 0.6 |
| Melons/oriental melons | 1.06 (1.00–1.12) | 0.051 | 1.02 (0.96–1.08) | 0.5 |
| Watermelons | 0.98 (0.93–1.03) | 0.4 | 0.98 (0.93–1.03) | 0.4 |
| Peaches/apricots | 0.97 (0.91–1.03) | 0.3 | 0.99 (0.93–1.05) | 0.8 |
| Bananas | 0.94 (0.88–0.99) | 0.028 | 0.94 (0.88–1.00) | 0.039 |
| Persimmons/dried persimmons | 0.99 (0.94–1.04) | 0.6 | 0.97 (0.92–1.02) | 0.3 |
| Tangerines | 0.93 (0.89–0.97) | <0.001 | 0.96 (0.92–1.00) | 0.060 |
| Pears | 0.98 (0.92–1.03) | 0.4 | 0.96 (0.90–1.01) | 0.14 |
| Apples | 0.95 (0.91–0.99) | 0.014 | 0.96 (0.92–1.01) | 0.10 |
| Oranges | 0.96 (0.89–1.03) | 0.2 | 0.99 (0.93–1.06) | 0.9 |
| Grapes | 0.87 (0.82–0.93) | <0.001 | 0.90 (0.84–0.96) | <0.001 |
| Tomatoes‡ | - | - | - | - |
* Adjusted for age (years), body mass index (16.0–19.9, 20.0–24.9, ≥25.0 kg/m2), smoking status (never, former, current), physical activity (<120, 120–180, >180 min/wk of moderate to vigorous exercise), family history of diabetes (yes or no), and total energy intake (kcal/d). Individual fruit consumption was mutually adjusted.
Table 3.
| Items* |
Unadjusted (N=57,419) |
Adjusted† (N=57, 419) |
|||
|---|---|---|---|---|---|
| HR‡ (95% CI) | P-value | HR‡ (95% CI) | P-value | ||
| Grouped by glycemic loads | |||||
| High GL | 0.97 (0.93–1.00) | 0.059 | 0.97 (0.94–1.00) | 0.091 | |
| Middle GL | 1.07 (1.03–1.12) | <0.001 | 1.03 (0.98–1.07) | 0.2 | |
| Low GL§ | - | - | - | - | |
| Grouped by glycemic values | |||||
| High GI | 1.03 (0.98–1.07) | 0.2 | 1.02 (0.97–1.06) | 0.4 | |
| Middle GI | 0.95 (0.92–0.98) | <0.001 | 0.97 (0.94–1.00) | 0.046 | |
| Low GI§ | - | - | - | - | |
| Fruits, total | 0.99 (0.98–1.01) | 0.2 | 1.00 (0.99–1.01) | >0.9 | |
From Food database by the Korean Ministry of Food and Drug Safety [Internet]. Cheongju: Korean Ministry of Food and Drug Safety; 2023 [cited 2023 Nov 2]. Available from: https://various.foodsafetykorea.go.kr/nutrient/13); Song S, et al. Korean J Nutr 2012;45:80-93. [2]
HR, hazard ratio; CI, confidence interval; GI, glycemic index; GL, glycemic load.
* The fruits were grouped as follows: low GI fruits (strawberries, peaches/apricots, pears, apples, oranges, tomatoes), middle GI fruits (persimmons/dried persimmons, tangerines, grapes), high GI fruits (melons/oriental melons, watermelons, bananas), low GL fruits (strawberries, peaches/apricots, tangerines, pears, apples, tomatoes), middle GL fruits (melons/oriental melons, persimmons/dried persimmons), and high GL fruits (watermelons, bananas, oranges, grapes).
† Adjusted for age (years), body mass index (16.0–19.9, 20.0–24.9, ≥25.0 kg/m2), smoking status (never, former, current), physical activity (<120, 120–180, >180 min/wk of moderate to vigorous exercise), family history of diabetes (yes or no), and total energy intake (kcal/d). Individual fruit consumption was mutually adjusted.