|
 |
- Search
| Korean J Fam Med > Epub ahead of print |
|
Abstract
Background
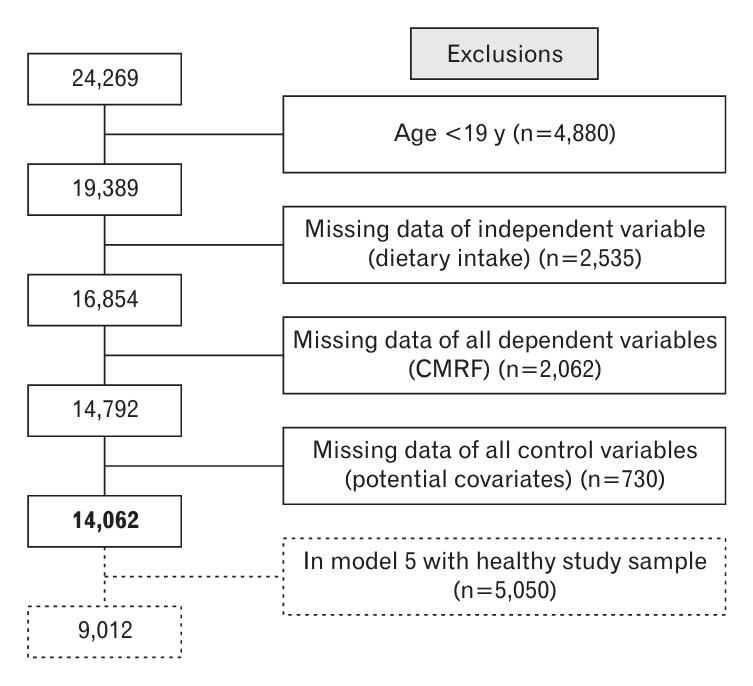
Methods
Results
Table┬Ā1.
Table┬Ā2.
| Characteristic |
Categories of regular meal skipping (N=14,062) |
P-value* | |||||||
|---|---|---|---|---|---|---|---|---|---|
| G1 (RE) (N=8,120) | G2 (ID) (N=432) | G3 (IL) (N=641) | G4 (IB) (N=3,515) | G5 (ILD) (N=131) | G6 (IBD) (N=567) | G7 (IBL) (N=456) | G8 (IBLD) (N=200) | ||
| Age (y) | <0.0001 | ||||||||
| ŌĆā19ŌĆō29 (n=1,569) | 357 (4.40) | 55 (12.73) | 37 (5.77) | 770 (21.91) | 15 (11.45) | 160 (28.22) | 119 (26.10) | 56 (28.00) | |
| ŌĆā30ŌĆō39 (n=2,243) | 721 (8.88) | 66 (15.28) | 70 (10.92) | 997 (28.36) | 25 (19.08) | 155 (27.34) | 148 (32.46) | 61 (30.50) | |
| ŌĆā40ŌĆō49 (n=2,620) | 1,279 (15.75) | 88 (20.37) | 101 (15.76) | 874 (24.86) | 19 (14.50) | 136 (23.99) | 87 (19.08) | 36 (18.00) | |
| ŌĆā50ŌĆō59 (n=2,649) | 1,700 (20.94) | 103 (23.84) | 107 (16.69) | 548 (15.59) | 27 (20.61) | 77 (13.58) | 51 (11.18) | 36 (18.00) | |
| ŌĆā60ŌĆō69 (n=2,533) | 2,010 (24.75) | 69 (15.97) | 144 (22.46) | 231 (6.57) | 20 (15.27) | 24 (4.23) | 29 (6.36) | 6 (3.00) | |
| ŌĆā70ŌĆō80 (n=2,448) | 2,053 (25.28) | 51 (11.81) | 182 (28.39) | 95 (2.70) | 25 (19.08) | 15 (2.65) | 22 (4.82) | 5 (2.50) | |
| Gender | <0.0001 | ||||||||
| ŌĆāMale (n=5,996) | 3,592 (44.24) | 117 (27.08) | 222 (34.63) | 1,676 (47.68) | 30 (22.90) | 153 (26.98) | 153 (33.55) | 53 (26.50) | |
| ŌĆāFemale (n=8,066) | 4,528 (55.76) | 315 (72.92) | 419 (65.37) | 1,839 (52.32) | 101 (77.10) | 414 (73.02) | 303 (66.45) | 147 (73.50) | |
| Household income | <0.0001 | ||||||||
| ŌĆāLow (n=2,681) | 1,847 (22.75) | 66 (15.28) | 229 (35.73) | 346 (9.84) | 28 (21.37) | 64 (11.29) | 72 (15.79) | 29 (14.50) | |
| ŌĆāMiddle-low(n=3,429) | 1,986 (24.46) | 108 (25.00) | 153 (23.87) | 859 (24.44) | 34 (25.95) | 131 (23.10) | 112 (24.56) | 46 (23.00) | |
| ŌĆāMiddle-high (n=3,842) | 2,013 (24.79) | 115 (26.62) | 137 (21.37) | 1,168 (33.23) | 28 (21.37) | 177 (31.22) | 139 (30.48) | 65 (32.50) | |
| ŌĆāHigh (n=4,110) | 2,274 (28.00) | 143 (33.10) | 122 (19.03) | 1,142 (32.49) | 41 (31.30) | 195 (34.39) | 133 (29.17) | 60 (30.00) | |
| Education level | <0.0001 | ||||||||
| ŌĆāLower or no education (n=2,931) | 2,277 (28.04) | 82 (18.98) | 206 (32.14) | 230 (6.54) | 37 (28.24) | 35 (6.17) | 47 (10.31) | 17 (8.50) | |
| ŌĆāMiddle-school education (n=1,429) | 1,025 (12.62) | 36 (8.33) | 86 (13.42) | 217 (6.17) | 9 (6.87) | 28 (4.94) | 19 (4.17) | 9 (4.50) | |
| ŌĆāHigh-school education (n=4,456) | 2,284 (28.13) | 149 (34.49) | 188 (29.33) | 1,303 (37.07) | 38 (29.01) | 208 (36.68) | 193 (42.32) | 93 (46.50) | |
| ŌĆāCollege and higher (n=5,246) | 2,534 (31.21) | 165 (38.19) | 161 (25.12) | 1,765 (50.21) | 47 (35.88) | 296 (52.20) | 197 (43.20) | 81 (40.50) | |
| Work shift | <0.0001 | ||||||||
| ŌĆāDay shift (n=7,970) | 4,433 (54.59) | 243 (56.25) | 247 (38.53) | 2,343 (66.66) | 54 (41.22) | 353 (62.26) | 208 (45.61) | 89 (44.50) | |
| ŌĆāSwing or night shift (n=1,579) | 660 (8.13) | 55 (12.73) | 89 (13.88) | 517 (14.71) | 22 (16.79) | 99 (17.46) | 90 (19.74) | 47 (23.50) | |
| ŌĆāUnemployed (n=4,513) | 3,027 (37.28) | 134 (31.02) | 305 (47.58) | 655 (18.63) | 55 (41.98) | 115 (20.28) | 158 (34.65) | 64 (32.00) | |
| Physical activity | |||||||||
| ŌĆāNo (n=8,001) | 4,732 (58.28) | 230 (53.24) | 400 (62.40) | 1,944 (55.31) | 77 (58.78) | 275 (48.50) | 243 (53.29) | 100 (50.00) | <0.0001 |
| ŌĆāYes (n=6,061) | 3,388 (41.72) | 202 (46.76) | 241 (37.60) | 1,571 (44.69) | 54 (41.22) | 292 (51.50) | 213 (46.71) | 100 (50.00) | |
| Smoking status | |||||||||
| ŌĆāNever (n=8,648) | 5,082 (62.59) | 313 (72.45) | 412 (64.27) | 1,966 (55.93) | 89 (67.94) | 388 (68.43) | 268 (58.77) | 130 (65.00) | <0.0001 |
| ŌĆāFormer (n=3,048) | 2,035 (25.06) | 62 (14.35) | 117 (18.25) | 654 (18.61) | 18 (13.74) | 66 (11.64) | 72 (15.79) | 24 (12.00) | |
| ŌĆāCurrent (n=2,366) | 1,003 (12.35) | 57 (13.19) | 112 (25.46) | 895 (25.46) | 24 (18.32) | 113 (19.93) | 116 (25.44) | 46 (23.00) | |
| Alcohol consumption | <0.0001 | ||||||||
| ŌĆāNo (n=6,547) | 4,234 (52.14) | 206 (47.69) | 349 (54.45) | 1,255 (35.70) | 67 (51.15) | 184 (32.45) | 179 (39.25) | 73 (36.50) | |
| ŌĆāYes (n=7,515) | 3,886 (47.86) | 226 (52.31) | 292 (45.55) | 2,260 (64.30) | 64 (48.85) | 383 (67.55) | 277 (60.75) | 127 (63.50) | |
| Hypertension (% by row) | <0.0001 | ||||||||
| ŌĆāNo (n=10,566) | 5,462 (51.69) | 344 (3.26) | 423 (4.00) | 3,144 (29.76) | 98 (0.93) | 514 (4.86) | 406 (3.84) | 175 (1.66) | |
| ŌĆāYes (n=3,496) | 2,658 (76.03) | 88 (2.52) | 218 (6.24) | 371 (10.61) | 33 (0.94) | 53 (1.52) | 50 (1.43) | 25 (0.72) | |
| Hyperlipidemia (% by row) | <0.0001 | ||||||||
| ŌĆāNo (n=11,425) | 6,192 (54.20) | 358 (3.13) | 484 (4.24) | 3,180 (27.83) | 100 (0.88) | 513 (4.49) | 419 (3.67) | 179 (1.57) | |
| ŌĆāYes (n=2,637) | 1,928 (73.11) | 74 (2.81) | 157 (5.95) | 335 (12.70) | 31 (1.18) | 54 (2.05) | 37 (1.40) | 21 (0.80) | |
| Stroke (% by row) | <0.0001 | ||||||||
| ŌĆāNo (n=13,739) | 7,878 (57.34) | 419 (3.05) | 625 (4.55) | 3,480 (25.33) | 126 (0.92) | 559 (4.07) | 455 (3.31) | 197 (1.43) | |
| ŌĆāYes (n=323) | 242 (74.92) | 13 (4.02) | 16 (4.95) | 35 (10.84) | 5 (1.55) | 8 (2.48) | 1 (0.31) | 3 (0.93) | |
| Myocardial infarction (% by row) | |||||||||
| ŌĆāNo (n=13,901) | 7,991 (57.49) | 424 (3.05) | 635 (4.57) | 3,507 (25.23) | 130 (0.94) | 563 (4.05) | 453 (3.26) | 198 (1.42) | <0.0001 |
| ŌĆāYes (n=161) | 129 (80.12) | 8 (4.97) | 6 (3.73) | 8 (4.97) | 1 (0.62) | 4 (2.48) | 3 (1.86) | 2 (1.24) | |
| Angina pectoris (% by row) | <0.0001 | ||||||||
| ŌĆāNo (n=13,768) | 7,890 (57.31) | 421 (3.06) | 622 (4.52) | 3,494 (25.38) | 127 (0.92) | 560 (4.07) | 455 (3.30) | 199 (1.45) | |
| ŌĆāYes (n=294) | 230 (78.23) | 11 (3.74) | 19 (6.46) | 21 (7.14) | 4 (1.36) | 7 (2.38) | 1 (0.34) | 1 (0.34) | |
| Diabetes (% by row) | <0.0001 | ||||||||
| ŌĆāNo (n=12,697) | 7,037 (55.42) | 409 (3.22) | 559 (4.40) | 3,387 (26.68) | 124 (0.98) | 554 (4.36) | 436 (3.43) | 191 (1.50) | |
| ŌĆāYes (n=1,365) | 1,083 (79.34) | 23 (1.68) | 82 (6.01) | 128 (9.38) | 7 (0.51) | 13 (0.95) | 20 (1.47) | 9 (0.66) | |
| Energy intake (kcal/d) | 1,955.7┬▒824.5 | 1,783.6┬▒839.2 | 1,696.9┬▒910.9 | 2,072.9┬▒999.9 | 1,614.9┬▒862.0 | 1,737.9┬▒896.5 | 1,797.6┬▒901.7 | 1,673.4┬▒992.3 | <0.0001 |
| Body mass index (kg/m2) | 24.01┬▒3.28 | 24.39┬▒3.58 | 24.3┬▒3.85 | 23.9┬▒3.86 | 24.62┬▒3.74 | 24.1┬▒3.99 | 23.79┬▒4.03 | 24.03┬▒4.04 | 0.0087 |
Table┬Ā3.
| Cardio-metabolic risk factors |
Categories of regular meal skipping (N=14,062) |
|||||||
|---|---|---|---|---|---|---|---|---|
| G1 (RE) (N=8,120) | G2 (ID) (N=432) | G3 (IL) (N=641) | G4 (IB) (N=3,515) | G5 (ILD) (N=131) | G6 (IBD) (N=567) | G7 (IBL) (N=456) | G8 (IBLD) (N=200) | |
| High-sensitive CRPŌĆĀ (mg/dL) | 0 | 0.02 | -0.03 | 0.01 | 0.19 | 0.10 | 0.08 | 0.26 |
| Systolic blood pressureŌĆĪ (mm Hg) | 0 | 0.78 | -0.73 | 0.55(*) | -0.94 | -0.79 | 1.07 | 1.58 |
| Diastolic blood pressureŌĆĪ (mm Hg) | 0 | -0.26 | 0.33 | 0.94*** | -1.07 | 0.48 | 1.65*** | 1.95** |
| Fasting blood sugar┬¦ (mg/dL) | 0 | -1.06 | -0.29 | 0.94* | 3.67(*) | 0.60 | 0.90 | 0.25 |
| Hemoglobin A1c┬¦ (%) | 0 | -0.05 | -0.004 | 0.0001 | 0.10 | -0.05* | -0.04 | -0.04 |
| Total cholesterolŌłź (mg/dL) | 0 | 2.61** | 4.17 | 5.17*** | 3.68 | 5.03*** | 6.02*** | 3.18 |
| HDL-CŌłź (mg/dL) | 0 | 2.09*** | 0.67 | 0.27 | -0.02 | 1.07* | 0.55 | 0.29 |
| LDL-CŌłź (n=2,163) (mg/dL) | 0 | 2.91 | 6.04(*) | 4.83** | -4.42 | 7.02 | 4.49 | 14.79(*) |
| Calculated LDL-CŌłź (mg/dL) | 0 | 1.06 | 2.84* | 3.54** | -3.17 | 2.16 | 3.02(*) | 1.25 |
| TriglycerideŌłź (mg/dL) | 0 | -2.73 | 3.30 | 6.78** | 34.31* | 9.02 | 13.18* | 5.04 |
By multiple linear regression; all values are ╬▓-coefficient. Statistically significant results are marked in bold.
RE, regular eater; ID, irregular dinner; IL, irregular lunch; IB, irregular breakfast; ILD, irregular lunch & dinner; IBD, irregular breakfast and dinner; IBL, irregular breakfast and lunch; IBLD, irregular breakfast & lunch & dinner; CRP, C-reactive protein; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Table┬Ā4.
| Cardio-metabolic risk factors |
Categories of regular meal skipping (N=9,012) |
|||||||
|---|---|---|---|---|---|---|---|---|
| G1 (RE) (N=4,354) | G2 (ID) (N=299) | G3 (IL) (N=332) | G4 (IB) (N=2,923) | G5 (ILD) (N=81) | G6 (IBD) (N=479) | G7 (IBL) (N=383) | G8 (IBLD) (N=161) | |
| Systolic blood pressure (mm Hg) | 0 | 0.48 | 0.63 | 0.49 | 0.71 | -0.16 | 1.10 | 1.79 |
| Diastolic blood pressure (mm Hg) | 0 | -0.06 | 0.52 | 1.00*** | 0.18 | 0.83(*) | 1.95*** | 2.45*** |
| Fasting blood sugar (mg/dL) | 0 | -0.59 | 0.05 | 0.89* | 1.82 | 0.69 | 1.19 | -0.01 |
| Hemoglobin A1c (%) | 0 | -0.02 | -0.001 | -0.011 | 0.04 | -0.05* | -0.05* | -0.02 |
| High-sensitive CRP (mg/dL) | 0 | 0.03 | -0.06 | -0.06 | -0.17 | 0.08 | 0.07 | 0.34(*) |
| Total cholesterol (mg/dL) | 0 | 1.49 | 6.47*** | 4.92*** | 8.09* | 3.94* | 6.62*** | 1.21 |
| HDL-C (mg/dL) | 0 | 2.38*** | 0.94 | 0.33 | 1.41 | 1.34* | 0.49 | 0.32 |
| LDL-C (N=1,173; mg/dL) | 0 | 0.33 | 5.61 | 4.58* | 7.20 | 0.11 | 2.66 | 4.37 |
| Calculated LDL-C (mg/dL) | 0 | -0.25 | 5.28** | 3.24*** | 2.65 | 1.99 | 3.74* | -0.56 |
| Triglyceride (mg/dL) | 0 | -3.20 | 1.28 | 6.78** | 20.17(*) | 3.04 | 11.95(*) | 7.26 |
All values are ╬▓-coefficient. Statistically significant results are marked in bold. By multiple linear regression (model 5: adjusted for age, sex, household income, education level, work shift, physical activity, smoking status, alcohol consumption, energy intake, and body mass index).
RE, regular eater; ID, irregular dinner; IL, irregular lunch; IB, irregular breakfast; ILD, irregular lunch & dinner; IBD, irregular breakfast and dinner; IBL, irregular breakfast and lunch; IBLD, irregular breakfast & lunch & dinner; CRP, C-reactive protein; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Table┬Ā5.
| Cardio-metabolic risk factors |
Categories of regular meal skipping (N=14,062) |
|||||||
|---|---|---|---|---|---|---|---|---|
| G1 (RE) | G2 (ID) | G3 (IL) | G4 (IB) | G5 (ILD) | G6 (IBD) | G7 (IBL) | G8 (IBLD) | |
| Systolic blood pressure (mm Hg) | 118.91┬▒0.17 | 0.78 | -0.72 | 0.55(*) | -0.94 | -0.79 | 1.07 | 1.58 |
| Diastolic blood pressure (mm Hg) | 75.09┬▒0.11 | -0.27 | 0.32 | 0.94*** | -1.08 | 0.47 | 1.64*** | 1.95** |
| Fasting blood sugar (mg/dL) | 101.06┬▒0.23 | -1.06 | -0.29 | 0.93* | 3.67(*) | 0.59 | +0.9 | 0.25 |
| Hemoglobin A1c (%) | 5.72┬▒0.01 | -0.05(*) | -0.01 | 0.002 | 0.07 | -0.05* | -0.04 | -0.03 |
| High-sensitive CRP (mg/dL) | 1.18┬▒0.02 | 0.02 | -0.03 | 0.01 | 0.19 | +0.10 | 0.08 | 0.26 |
| Total cholesterol (mg/dL) | 190.53┬▒0.40 | 2.61 | 4.16** | 5.16*** | 3.67 | 5.03*** | 6.02*** | 3.18 |
| HDL-C (mg/dL) | 50.83┬▒0.13 | 2.1*** | 0.67 | 0.28 | -0.02 | 1.07* | 0.37 | 0.93 |
| LDL-C (n=2,163; mg/dL) | 114.69┬▒1.03 | 2.91 | 6.04(*) | 4.84** | -4.42 | 7.02 | 4.49 | 14.8(*) |
| Calculated LDL-C (mg/dL) | 113.16┬▒0.37 | 1.07 | 2.84* | 3.53*** | -3.17 | 2.16 | 3.02(*) | 1.24 |
| Triglyceride (mg/dL) | 132.69┬▒1.20 | -2.73 | 3.30 | 6.78** | 34.31(*) | 9.02 | 13.18* | 5.04 |
Values are presented as mean┬▒standard error or marginal difference. Statistically significant results are marked in bold. By multiple linear regression.
RE, regular eater; ID, irregular dinner; IL, irregular lunch; IB, irregular breakfast; ILD, irregular lunch & dinner; IBD, irregular breakfast and dinner; IBL, irregular breakfast and lunch; IBLD, irregular breakfast & lunch & dinner; CRP, C-reactive protein; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Table┬Ā6.
| Cardio-metabolic risk factors |
Categories of regular meal skipping (N=9,012) |
|||||||
|---|---|---|---|---|---|---|---|---|
| G1 (RE) | G2 (ID) | G3 (IL) | G4 (IB) | G5 (ILD) | G6 (IBD) | G7 (IBL) | G8 (IBLD) | |
| Systolic blood pressure (mm Hg) | 114.42┬▒0.21 | +0.48 | 0.63 | 0.49 | 0.71 | -0.16 | 1.1 | 1.79 |
| Diastolic blood pressure (mm Hg) | 74.81┬▒0.14 | -0.06 | 0.53 | 1.01*** | 0.18 | 0.84(*) | 1.95*** | 2.46*** |
| Fasting blood sugar (mg/dL) | 95.09┬▒0.25 | -0.60 | 0.04 | 0.88** | 1.82 | 0.68 | 1.19 | -0.02 |
| Glycated hemoglobin (%) | 5.49┬▒0.01 | -0.025 | -0.002 | -0.01 | 0.04 | -0.05* | -0.05* | -0.02 |
| High-sensitive CRP (mg/dL) | 1.08┬▒0.03 | +0.03 | -0.06 | -0.01 | -0.17 | 0.08 | 0.07 | 0.34(*) |
| Total Cholesterol (mg/dL) | 194.37┬▒0.53 | +1.48 | 6.47*** | 4.92*** | 8.09* | 3.94* | 6.62*** | 1.21 |
| HDL-cholesterol (mg/dL) | 52.32┬▒0.18 | +2.38*** | 0.95 | 0.33 | 1.42 | 1.35* | 0.49 | 0.33 |
| LDL-cholesterol (N=1,173; mg/dL) | 121.94┬▒1.51 | +0.34 | 5.62 | 4.59* | 7.21 | 0.11 | 2.67 | 4.37 |
| Calculated LDL-chol. (mg/dL) | 117.50┬▒0.48 | -0.25 | 5.28* | 3.24*** | 2.65 | 1.99 | 3.74* | -0.56 |
| Triglyceride (mg/dL) | 122.71┬▒1.53 | -3.21 | 1.28 | 6.78** | 20.17(*) | 3.03 | 11.94(*) | 7.26 |
Values are presented as mean┬▒standard error or marginal difference. Statistically significant results are marked in bold. By multiple linear regression.
RE, regular eater; ID, irregular dinner; IL, irregular lunch; IB, irregular breakfast; ILD, irregular lunch & dinner; IBD, irregular breakfast and dinner; IBL, irregular breakfast and lunch; IBLD, irregular breakfast & lunch & dinner; CRP, C-reactive protein; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.