 |
 |
- Search
| Korean J Fam Med > Volume 43(6); 2022 > Article |
|
Abstract
Background
Methods
Results
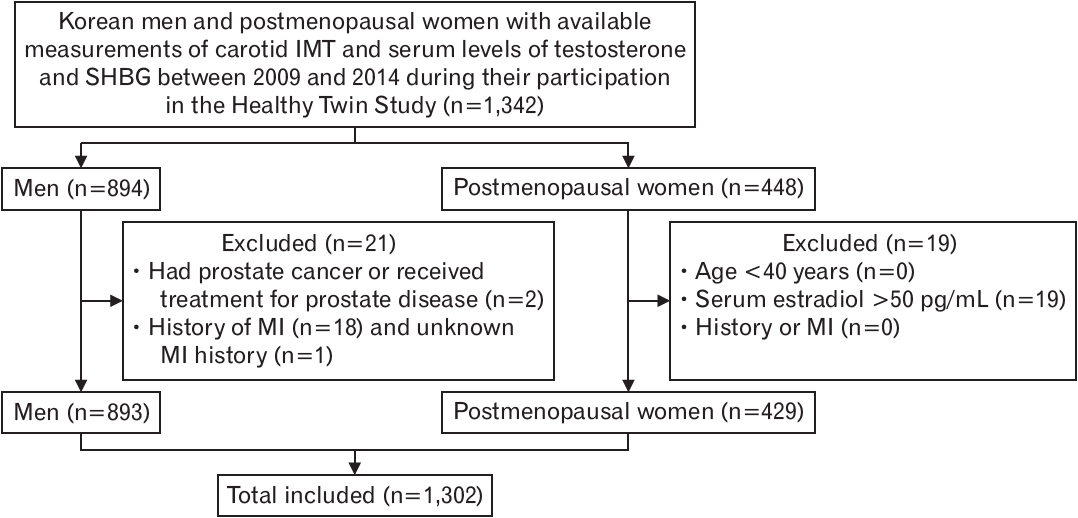
Figure.┬Ā1.
Table┬Ā1.
| Characteristic | Men (N=873) | Women (N=429) |
|---|---|---|
| Age (y) | 46.0┬▒14.7 | 61.3┬▒8.2 |
| Intima-media thickness (cm) | ||
| ŌĆāCommon carotid artery | 0.056┬▒0.02 | 0.063┬▒0.02 |
| ŌĆāInternal carotid artery* | 0.05┬▒0.03 | 0.052┬▒0.02 |
| ŌĆāBifurcation* | 0.079┬▒0.05 | 0.092┬▒0.04 |
| ŌĆāCombinedŌĆĀ | 0.062┬▒0.03 | 0.069┬▒0.02 |
| Sex hormones (nmol/L) | ||
| ŌĆāTotal testosterone | 593.4┬▒215.5 | 37.5┬▒24.8 |
| ŌĆāCalculated free testosterone | 10.93┬▒4.2 | 0.45┬▒0.4 |
| ŌĆāSex hormone binding globulin | 42.6┬▒20.4 | 73.51┬▒35.5 |
| Non-high-density lipoprotein cholesterol (mg/dL) | 141.3┬▒36.2 | 153.2┬▒36.3 |
| Body mass index (kg/m2) | 24.0┬▒3.2 | 23.8┬▒3.4 |
| HypertensionŌĆĪ | 186 (21.3) | 139 (32.4) |
| Diabetes mellitus┬¦ | 61 (7.0) | 40 (9.3) |
| Smoking habit* | ||
| ŌĆāNever smoker | 267 (30.7) | 410 (95.8) |
| ŌĆāEx-smoker | 252 (28.9) | 8 (1.9) |
| ŌĆāCurrent smoker | 352 (40.4) | 10 (2.3) |
| Regular physical exercise* | ||
| ŌĆā<1/wk | 497 (56.9) | 260 (60.6) |
| ŌĆā1ŌĆō2/wk | 159 (18.2) | 37 (8.6) |
| ŌĆāŌēź3/wk | 192 (22.0) | 128 (29.8) |
| Alcohol consumption* | ||
| ŌĆāCurrent | 684 (78.7) | 139 (32.8) |
| ŌĆāNo | 185 (21.3) | 285 (67.2) |
* Information was missing in some study subjects: internal carotid artery (male 13, female 4), bifurcation (male 1), smoking (male 2, female 1), physical exercise (male 25, female 4), and alcohol consumption (male 4, female 5).
Table┬Ā2.
| Variable | Overall |
Quartiles of total testosterone level (nmol/L) |
P trend | ||||
|---|---|---|---|---|---|---|---|
| Q1 (Ōēż445) | Q2 (446ŌĆō584) | Q3 (585ŌĆō709) | Q4 (Ōēź710) | ||||
| No. of subjects (persons) | 873 | 219 | 218 | 218 | 218 | ||
| Age (y) | 46.0┬▒14.7 | 47.7┬▒13.8 | 47.0┬▒14.1 | 45.0┬▒14.6 | 44.2┬▒15.6 | 0.001 | |
| Sex hormones (nmol/L) | |||||||
| Calculated free testosterone | 10.9┬▒4.2 | 6.8┬▒2.1 | 9.9┬▒2.2 | 12.0┬▒2.7 | 14.8┬▒4.5 | 0.000 | |
| Sex hormone binding globulin | 42.6┬▒20.4 | 32.8┬▒16.3 | 38.8┬▒15.2 | 43.4┬▒16.8 | 55.2┬▒24.8 | 0.000 | |
| Intima-media thickness (cm) | |||||||
| Common carotid artery | 0.056┬▒0.02 | 0.057┬▒0.02 | 0.059┬▒0.02 | 0.054┬▒0.02 | 0.053┬▒0.02 | 0.012 | |
| Internal carotid artery* | 0.05┬▒0.02 | 0.05┬▒0.02 | 0.053┬▒0.03 | 0.051┬▒0.03 | 0.046┬▒0.01 | 0.050 | |
| Bifurcation* | 0.079┬▒0.05 | 0.083┬▒0.06 | 0.087┬▒0.05 | 0.074┬▒0.04 | 0.074┬▒0.04 | 0.014 | |
| CombinedŌĆĀ | 0.062┬▒0.02 | 0.063┬▒0.03 | 0.066┬▒0.03 | 0.060┬▒0.02 | 0.058┬▒0.02 | 0.014 | |
| Non-high density lipoprotein cholesterol (mg/dL) | 141.2┬▒36.1 | 144.9┬▒37.3 | 145.4┬▒36.3 | 140.2┬▒36.4 | 134.55┬▒33.5 | 0.000 | |
| Body mass index (kg/m2) | 23.9┬▒3.1 | 24.3┬▒3.2 | 24.4┬▒3.5 | 23.8┬▒2.8 | 23.2┬▒2.9 | 0.000 | |
| HypertensionŌĆĪ | 186 (21.3) | 52 (23.7) | 44 (20.2) | 45 (20.6) | 45 (20.6) | 0.475 | |
| Diabetes mellitus┬¦ | 61 (7.0) | 21 (9.6) | 18 (8.3) | 10 (4.6) | 12 (5.5) | 0.039 | |
| Smoking status* | 0.049 | ||||||
| Never smoker | 267 (30.7) | 72 (33.0) | 61 (28.1) | 68 (31.2) | 66 (30.3) | ||
| Ex-smoker | 252 (28.9) | 75 (34.4) | 72 (33.2) | 52 (23.9) | 53 (24.3) | ||
| Current smoker | 352 (40.4) | 71 (32.6) | 84 (38.7) | 98 (45.0) | 99 (45.4) | ||
| Physical exercise* | 0.989 | ||||||
| <1/wk | 497 (58.6) | 124 (58.8) | 124 (59.1) | 127 (60.2) | 122 (56.5) | ||
| 1ŌĆō2/wk | 159 (18.8) | 38 (18.0) | 39 (18.6) | 39 (18.5) | 43 (19.9) | ||
| Ōēź3/wk | 192 (22.0) | 49 (23.2) | 47 (22.4) | 45 (21.3) | 51 (23.6) | ||
| Current alcohol consumption* | 0.294 | ||||||
| No | 185 (21.2) | 49 (22.5) | 52 (24.0) | 41 (18.9) | 43 (19.8) | ||
| Yes | 684 (78.4) | 169 (77.5) | 165 (76.0) | 176 (81.1) | 174 (80.2) | ||
Values are presented as mean┬▒standard deviation or number (%). P-values for trend were assessed by SpearmanŌĆÖs correlation analysis for continuous variables and by the CochranŌĆōMantelŌĆōHaenszel test for categorical variables.
Table┬Ā3.
| Variable | Overall |
Quartiles of total testosterone level (nmol/L) |
P trend | ||||
|---|---|---|---|---|---|---|---|
| Q1 (Ōēż24) | Q2 (25ŌĆō35.0) | Q3 (36.0ŌĆō47.0) | Q4 (Ōēź48.0) | ||||
| No. of subjects (persons) | 429 | 107 | 114 | 105 | 103 | ||
| Age (y) | 61.3┬▒8.2 | 62.7┬▒8.8 | 61.6┬▒8.1 | 60.8┬▒7.6 | 60.0┬▒7.8 | 0.016 | |
| Sex hormones (nmol/L) | |||||||
| Calculated free testosterone | 0.4┬▒0.4 | 0.2┬▒0.1 | 0.3┬▒0.1 | 0.5┬▒0.1 | 0.8┬▒0.8 | 0.000 | |
| Sex hormone binding globulin | 73.5┬▒35.4 | 77.3┬▒35.1 | 75.6┬▒38.6 | 73.6┬▒38.5 | 67.1┬▒27.7 | 0.067 | |
| Intima-media thickness (cm) | |||||||
| Common carotid artery | 0.063┬▒0.02 | 0.061┬▒0.01 | 0.063┬▒0.01 | 0.063┬▒0.02 | 0.066┬▒0.02 | 0.352 | |
| Internal carotid artery* | 0.052┬▒0.02 | 0.052┬▒0.02 | 0.049┬▒0.01 | 0.055┬▒0.03 | 0.052┬▒0.02 | 0.889 | |
| Bifurcation* | 0.092┬▒0.04 | 0.095┬▒0.04 | 0.088┬▒0.03 | 0.091┬▒0.04 | 0.094┬▒0.04 | 0.444 | |
| CombinedŌĆĀ | 0.069┬▒0.02 | 0.069┬▒0.02 | 0.067┬▒0.01 | 0.070┬▒0.02 | 0.071┬▒0.02 | 0.649 | |
| Non-high-density lipoprotein cholesterol (mg/dL) | 153.1┬▒36.2 | 152.53┬▒37.7 | 151.60┬▒36.1 | 154.1┬▒33.9 | 154.7┬▒37.6 | 0.637 | |
| Body mass index (kg/m2) | 23.8┬▒3.3 | 23.3┬▒2.9 | 24.1┬▒3.7 | 23.5┬▒3.0 | 24.3┬▒3.6 | 0.090 | |
| HypertensionŌĆĪ | 139 (32.4) | 32 (29.9) | 47 (41.2) | 31 (29.5) | 29 (28.2) | 0.398 | |
| Diabetes mellitus┬¦ | 40 (9.3) | 10 (9.3) | 10 (8.8) | 12 (11.4) | 8 (7.8) | 0.879 | |
| Smoking status* | |||||||
| Never smoker | 410 (95.6) | 101 (94.4) | 111 (97.4) | 101 (96.2) | 97 (94.2) | 0.725 | |
| Ex-smoker | 8 (1.9) | 3 (2.8) | 1 (0.9) | 1 (1.0) | 3 (2.9) | ||
| Current smoker | 10 (2.3) | 3 (2.8) | 1 (0.9) | 3 (2.9) | 3 (2.9) | ||
| Regular physical exercise* | 0.043 | ||||||
| <1/wk | 260 (61.2) | 63 (59.4) | 65 (57.0) | 72 (69.2) | 60 (59.4) | ||
| 1ŌĆō2/wk | 37 (8.7) | 2 (1.9) | 13 (11.4) | 10 (9.6) | 12 (11.9) | ||
| Ōēź3/wk | 128 (30.1) | 41 (38.7) | 36 (31.6) | 22 (21.2) | 29 (28.7) | ||
| Current alcohol consumption* | |||||||
| No | 285 (66.4) | 70 (66.7) | 79 (69.9) | 65 (62.5) | 71 (69.6) | 0.959 | |
| Yes | 139 (32.4) | 35 (33.3) | 34 (30.1) | 39 (37.5) | 31 (30.4) | ||
Values are presented as mean┬▒standard deviation or number (%). P-values for trend were assessed by SpearmanŌĆÖs correlation analysis for continuous variables and by the CochranŌĆōMantelŌĆōHaenszel test for categorical variables.
Table┬Ā4.
| Sites of carotid intima media thickness measurement | Total testosterone | Calculated free testosterone | Sex hormone binding globulin | |
|---|---|---|---|---|
| Men aged Ōēź40 y (N=472) | ||||
| Common carotid artery | -4.5 (-7.6 to -1.3) | -3.3 (-6.7 to 0.1) | -1.3 (-3.8 to 1.3) | |
| Internal carotid artery | -2.2 (-6.0 to 1.7) | 0.6 (-3.4 to 4.8) | -2.3 (-5.1 to 0.7) | |
| Bifurcation | -3.4 (-7.7 to 1.1) | -3.0 (-7.6 to 1.8) | -0.5 (-4.0 to 3.2) | |
| CombinedŌĆĪ | -3.4 (-6.7 to 0.0) | -2.2 (-5.7 to 1.5) | -1.2 (-3.8 to 1.5) | |
| Men aged <40 y (N=401) | ||||
| Common carotid artery | 1.1 (-1.4 to 3.6) | 1.4 (-0.8 to 3.6) | 0.2 (-2.5 to 3.1) | |
| Internal carotid artery | -0.8 (-3.6 to 2.1) | -0.3 (-2.8 to 2.3) | -0.8 (-4.0 to 2.5) | |
| Bifurcation | 0.7 (-2.5 to 4.2) | 2.9 (-0.1 to 5.9) | -2.9 (-6.5 to 0.8) | |
| CombinedŌĆĪ | 0.2 (-2.2 to 2.6) | 1.3 (-0.8 to 3.5) | -1.6 (-4.2 to 1.1) | |
| Postmenopausal women (N=429) | ||||
| Common carotid artery | 4.5 (-4.2 to 14.1) | -3.6 (-7.5 to 16.0) | -0.9 (-3.8 to 2.1) | |
| Internal carotid artery | -0.7 (-11.7 to 11.6) | 0.8 (-13.3 to 17.1) | -1.0 (-4.9 to 3.1) | |
| Bifurcation | -8.3 (-19.2 to 4.0) | -13.8 (-26.6 to 1.4) | 1.7 (-2.5 to 6.2) | |
| CombinedŌĆĪ | -2.2 (-10.9 to 7.4) | -4.9 (-15.7 to 7.2) | 0.5 (-2.6 to 3.7) | |
* Adjusted for age, alcohol consumption, smoking status, physical exercise, body mass index, hypertension, diabetes mellitus, and non-high-density lipoprotein cholesterol.
ŌĆĀ ╬▓ coefficients per 1-SD increase of age-adjusted levels of each sex hormone were assessed by the linear mixed model for log-transformed carotid intima media thicknessmeasures. Then, % differences (95% confidence intervals) of carotid intima media thickness per 1-SD increase of age-adjusted levels of each sex hormone were calculated by subtracting 1 from the exponentiated ╬▓ coefficients.
REFERENCES
- TOOLS
-
METRICS

- Related articles in KJFM
-
The Relationship between Serum Cholesterol Level and Dietary Pattern.1996 October;17(10)






