|
 |
- Search
| Korean J Fam Med > Volume 45(1); 2024 > Article |
|
Abstract
Background
Appropriate nutrition is necessary for maintaining good health in the general population. During primary physician training, it is important to educate residents on the basic concepts of nutrition and methods to manage nutritional aspects according to various disease. However, little is known about the perception of nutritional education among Korean family medicine residents. This study analyzed the recognition of the importance of nutritional education, the amount received, and satisfaction with it as well as self-perceived competency in various nutrition topics among residents.
Methods
Web-based questionnaires were sent via mobile messages to all the residents registered with the Korean Academy of Family Medicine (KAFM). Out of 566 residents, 68 voluntarily participated in the study. The questionnaire consisted of 41 items related to perceptions of nutrition education, self-perceived competency in nutrition topics, and demographic characteristics.
Results
The response rate was 12.01%. Residents rated their satisfaction with nutrition education at 4.78 out of 10, and 83.3% considered it important. However, only 13.24% of the participants felt that it was adequate. The most common training method for nutrition education was lectures at KAFM conferences. Among the 29 nutritional topics, the residents reported highest confidence in subjects related to chronic diseases such as obesity (77.94%), diabetes (75%), cardiovascular disease (67.65%), gastrointestinal disorders (67.65%), and weight loss management (67.65%). Conversely, topics related to women (36.76%), children and adolescents (38.23%), drug-nutrient interactions (39.7%), eating disorders (42.64%), and food labels (42.64%) showed low self-perceived confidence rates.
Appropriate nutrition is necessary for maintaining good health. Excessive nutritional intake is a major cause of obesity and can reduce physical activity. It is well known that obesity causes various chronic diseases; therefore, proper nutritional management is important to prevent and treat these chronic diseases [1,2]. Conversely, poor nutrition is also associated with poor health outcomes. Malnourishment in patients can result in more complications, leading to increased mortality rates, longer hospital stay, and higher treatment costs [3]. Mortality rate and functional decline decreases, and quality of life improves when appropriate nutritional interventions are implemented in malnourished patients [4]. Additionally, readmission rates and medical costs are also reduced when nutritional therapy is administered [5].
Recently, much information about nutrition, such as diet and nutritional supplements, has surfaced in the media. Consequently, an increasing number of people seek consultation with doctors to clarify this uncertain nutrition-related information [6]. Although nutrition experts, such as dietitians, have specialized training, consumers tend to place more trust in the nutritional information provided by doctors [7,8], leading to positive behavioral changes [9]. In addition, nutrition-related approaches to patient care are developed by an interdisciplinary team consisting of doctors, nutritionists, nutrition nurses, and pharmacists. Sufficient nutritional knowledge is required for effective communication [6]. Therefore, as a primary physician, it is important to understand the basic concepts of nutrition and methods for managing nutritional aspects according to the patients’ diseases.
Training on nutrition-related topics is essential for family physicians in primary care settings. They are the first doctors to be seen by patients with health concerns, and play a significant role in the healthcare of people with chronic conditions, given their involvement in addressing widespread and ongoing health problems [10].
Nutritional education of doctors is lacking in medical school curriculum [11] and in training courses worldwide [12-15]. Previous studies have shown that family physicians [16], general practitioners (GP) [17-19], and residents [12,19-22] hold a positive attitude toward nutritional counseling or managing patients’ nutrition. However, their confidence in nutrition counseling or management abilities has been evaluated as insufficient [13,21] or moderate [18-20,22,23].
Few studies have examined the current state of nutrition education or residents’ awareness of nutrition in training courses for Korean family medicine (FM) majors. Therefore, in this study, we analyzed nutrition-related perceptions such as the importance of nutrition education, the amount of education received, overall satisfaction, and self-perceived competency in various nutrition topics among Korean FM residents.
This cross-sectional survey conducted in 2022 targeted 566 residents of the Korean Academy of Family Medicine (KAFM). In November 2022 a link to a web questionnaire created using Google Survey, was sent via mobile text messages to all residents using a mobile phone number registered with the KAFM. Seventy participants who voluntarily agreed to participate in the survey responded. Finally, 68 resident questionnaires were analyzed, excluding two that provided duplicate answers. This study was approved by the Institutional Review Board of Inje University Haeundaepaik Hospital (IRB approval no., 2022-09-009-004).
The survey consisted of 41 questions: five about perceptions related to nutrition education, 29 assessing perceptions of self-perceived competence on various nutrition-related topics, one question inquiring about nutrition-related topics that require more education during training, one open-ended question about nutrition education during training, and five questions on demographic characteristics. The questionnaire items were based on the Recommended Curriculum Guidelines for Family Medicine Residents regarding nutrition [24] and the Nutrition Curriculum Guide for Training Physicians [25], particularly regarding nutrition topics.
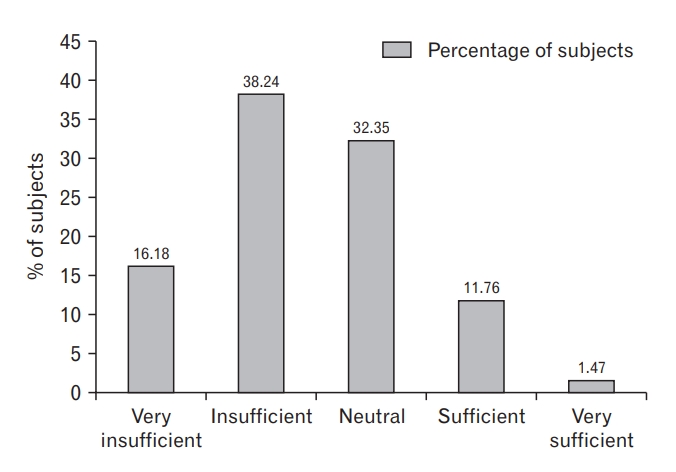
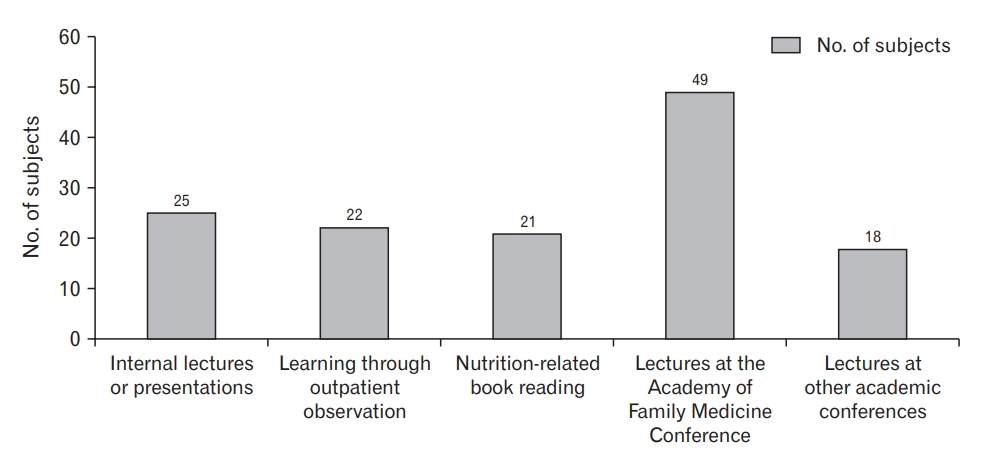
The five questions on perceptions related to nutritional education included overall satisfaction and importance, amount of education received in training and medical schools, and the educational methods received during training. Overall satisfaction with the nutritional education received during the training course was evaluated using a 10-point Likert scale. Recognition of the importance of nutritional education was categorized into five categories: strongly disagree, disagree, neither agree nor disagree, agree, and strongly agree. The duration of training and medical school was classified into five categories: very insufficient, insufficient, neutral, sufficient, and very sufficient. Regarding nutrition education methods, five relevant items were duplicated and selected from internal lectures or presentations, learning through outpatient observations, reading nutrition-related books, lectures from the Academy of FM Conferences, and lectures from other academic conferences.
Self-perceived competency was evaluated for each of the 29 topics that were classified into five categories: five questions on the basic principles of nutrition category, four questions on nutrition according to the life cycle category, 10 questions on the role of nutrition in the prevention and treatment of various diseases category, seven questions regarding nutrition evaluation and treatment category, and three questions about other nutrition topic categories (Table 1). Self-perceived competency level was chosen from five grades: very poor, poor, average, good, and excellent. A very poor grade indicates that the residents are not at the level of board-certified family doctors and require considerable effort to meet expectations. A poor grade indicates a slight decrease from the level of a board-certified family doctor but is easily correctable and has the potential to improve. The average grade is appropriate for a board-certified family doctor, and no immediate behavioral change is required. A good grade indicates that the residents are slightly better than the board-certified family doctors. Excellent: grade is above the level of board-certified family doctors. Participants selected their competency levels in various nutrition topics from among five categories.
In addition, participants were asked to select three of the 29 nutrition-related topics that they believed required more education during the training period. Additionally, they were encouraged to provide opinions on nutrition education during their training in a descriptive form.
Regarding demographic characteristics, age (<31 years, 31–35 years, and >35 years), sex (male and female), year of residency (first, second, and third year), size of training hospital (tertiary and secondary hospitals), and training area (Seoul, Gyeonggi-do, Incheon, Busan, Gwangju, Gyeongsang-do, Jeolla-do, Chungcheong-do, Gangwon-do, and Jeju-do) were documented.
Overall satisfaction with nutritional education was evaluated by calculating the mean scores. The importance and amount of nutrition education, education methods, self-perceived competency in 29 nutritionrelated topics, and demographic characteristics were expressed as frequencies and percentages. Stata SE ver. 15.0 (Stata Corp., College Station, TX, USA) was used to analyze the collected data.
Among the 566 residents, 68 participated in the survey, with a response rate of 12.01%. The average age of the participants was 33.4 years, and when divided into groups, 27.94% were under 30 years, 48.53% were between 31 and 35 years, and 28.53% were over 36 years. Females accounted for 64.71% (35.29% more than males). Regarding hospital size, the participation rate was higher for residents working in tertiary hospitals (69.21%) than for those working in secondary hospitals (30.88%). The percentages of first-, second-, and third-year residents who participated in the study were 35.29%, 27.94%, and 36.76%, respectively. The region with the highest participation was Seoul (57.35%), followed by Busan (14.71%) and Gyeonggi-do (8.82%) (Table 2).
The average score for overall satisfaction with nutrition-related education as evaluated by Korean FM residents was 4.78. In addition, 83.33% of the respondents strongly agreed or agreed that nutrition education is important for the training of residents, 16.67% of the respondents answered neither agree nor disagree, and none of the participants chose to disagree or strongly disagree. The percentages of residents who chose very insufficient, insufficient, neutral, sufficient, and very sufficient regarding the amount of nutrition education received during training were 16.18%, 38.24%, 32.35%, 11.76%, and 1.47%, respectively (Figure 1). Also, the percentages of subjects who chose the same category of answers for nutrition education received in medical school were 27.94%, 48.53%, 22.06%, 1.47%, and 0%, respectively. The residents believed that the nutritional education they received during training was more significant than what they received in medical schools. The most common type of nutrition education method received during training was lectures at the Academy of FM Conferences (49 participants, 72.05%), followed by internal lectures or presentations (25 participants, 36.76%), learning through outpatient observations (22 participants, 32.35%), nutrition-related book reading (21 participants, 30.88%), and lectures at other academic conferences (18 participants, 26.47%) (Figure 2).
Table 1 shows the self-perceived competencies of the FM residents regarding nutrition. Among the five response items of the survey, the ratio was obtained in three forms by combining very poor and poor into poor grades, and good and excellent into good grades. Among the 29 nutrition topics, those that residents believed they were lacking in competency were nutrition-related to the life cycle of women (63.24%), childhood and adolescence (61.76%), drug-nutrient interactions (60.29%), eating disorders (57.35%), food labels (57.35%), hematologic disorders (52.94%), malnutrition (52.94%), and secondary malnutrition caused by systemic diseases (52.94%). Conversely, subjects with a reduced perception of incompetence were obesity (22.06%), diabetes mellitus (25%), cardiovascular disease (32.35%), gastrointestinal disorders (32.35%), and weight loss management (32.35%). The topics that were thought to require more education during training were dietary guidelines (48.53%), the role of macronutrients (proteins, carbohydrates, and lipids), micronutrients (vitamins and minerals), fiber (33.82%), dietary supplements (26.47%), nutrition for old age (25%), and the nutritional content of staple foods (17.65%) (Table 3).
This study analyzed the awareness of nutrition education received by Korean FM residents during their training, and their confidence regarding various nutrition topics. Overall, satisfaction with the nutrition education received during training was 4.78, which was moderate. Few studies have evaluated the residents’ overall satisfaction with their nutritional education. According to a study on nutritional education among medical students in Canada [26], satisfaction was 4.7, similar to the results of our study. In this study, the percentage of residents’ perceptions of receiving sufficient and very sufficient nutrition education was low at 13.23%, which is similar to the findings of previous studies [12,13,19,22]. In a survey of GP trainees in Ireland, about 10% of the GP trainees who responded said that nutrition education for chronic disease management was appropriate [12]. In a survey involving a small number of American FM residents, 85% agreed that most physicians had not received adequate training to discuss nutritional problems with patients [13]. In a study targeting general internal medicine residents in Switzerland [19] and internal medicine residents in the United States [22], only 11.4% and 14% of the participants responded that they had been properly trained in nutrition education.
In this study, 83.33% of Korean FM residents agreed that nutritional education was important during training. These results are consistent with those of previous studies conducted worldwide, in which residents [12,13,19,20,22], GPs, and family doctors [16-19,23,27] showed a positive attitude toward nutrition education and counseling with patients. This shows that Korean FM residents consider nutritional management of patients to be important in clinical practice.
The most common nutritional education method identified in our study was lectures at Academy of FM Conferences. Although few previous studies have directly investigated educational methods for residents, according to a survey conducted by the directors of training institutions in the United States [14,15], the education provided by training institutions includes didactic lectures, informal rounds, special conferences, and web-based programs. Meanwhile, KAFM applied an education credit system based on entrustable professional activities following a conference held in 2019. As a result of this initiative, many residents participated in conferences, and those who participated in this study had been trained from 2020 to 2022. Therefore, conferences were selected as the most common nutritional education method.
Residents’ self-perceived competency in nutrition differed according to the topic. The topics in which the participants had highest confidence levels included chronic diseases, like obesity (77.94%), diabetes (75%), cardiovascular disease (67.65%), gastrointestinal disorders (67.65%), and weight loss management (67.65%). Conversely, lower levels of self-confidence were observed in areas related to women’s health (36.76%), children and adolescents (38.23%), drug-nutrient interactions (39.7%), eating disorders (42.64%), and food labels (42.64%), which is consistent with other studies [13,20,22,23]. According to the study by Cassidy-Vu and Kirk [13], American FM residents had relatively high confidence in nutritional topics related to clinical practice, such as osteoporosis, diabetes, gastrointestinal disorders, and malnutrition, and low confidence in topics related to nutritional demands of the elderly, infants, and children, as well as on vitamins, and dietary therapy. In addition, in the study by Nowson and O’Connell [20], 67% of Australian GP registrars showed confidence in the clinical scenario of nutritional counseling for patients with hyperlipidemia and obesity. In a study by Han et al. [22], 66% and 59% of residents were comfortable with the dietary pattern recommendations for patients with diabetes and dietary counseling in general practice, respectively. However, patients with weight loss due to chronic illness were less comfortable with nutritional counseling (36%) and assessment of fluid needs (38%). Al-Gassimi et al. [23] also showed sufficient confidence in topics on nutritional care for diet-related chronic diseases. In contrast, Crowley et al. [19] showed higher confidence in topics related to women, infants, and pediatric nutrition than in those related to chronic diseases.
In studies that evaluated self-perceived confidence in nutrition topics, including ours, there were many differences in the questionnaire content and number of items. There were also differences between the groups to be surveyed, which made an accurate comparison difficult. However, almost all studies have shown relatively high confidence in the nutritional management of diet-related chronic diseases such as diabetes. According to a factor analysis of GPs’ confidence in nutrition counseling [27], factors related to confidence include the type of patient diagnosis and patient subgroups. Perhaps, the topics learned most during training were most related to confidence.
Dietary guidelines (48.53%); the role of macronutrients, micronutrients, and fiber (33.82%); dietary supplements (26.47%); and nutrition for old age (25%) were the nutritional topics perceived as requiring more emphasis during the training of majors. This contrasted with the areas where they reported lack of confidence, such as nutrition for women, children, and adolescents. It is suggested that this selection was based on either inadequate educational coverage or the frequency of encountering these topics in clinical practice.
This study has some limitations. First, the questionnaire items were based on the recommended nutrition curriculum, but lacked validation. Second, the survey had a low response rate (12%); potentially limiting the generalizability of the findings. Finally, more positive results may have been obtained because of participation bias, as residents with particular interest in nutrition may have responded to the questionnaires. Additionally, this assessment confirmed self-perceived confidence and did not evaluate actual nutritional knowledge or management abilities. Therefore, further research employing an objective evaluation is required. Despite these limitations, our study is the first to evaluate awareness of and confidence in nutrition-related topics among Korean FM residents. In addition, although the response rate to the questionnaire was low, it targeted all the residents of the Korean Academy of FM; therefore, it was representative. Compared with other studies that evaluated self-confidence related to chronic diseases, mainly focusing on diet, our study offers a more comprehensive evaluation of each recommended nutritional topic for FM residents. Consequently, it allows for a clearer identification of topics that the residents perceive as lacking. Finally, future directions for education should also be elucidated.
In conclusion, despite the limited number of residents participating in this study, they recognized nutrition education as necessary, aligning with the perspectives of primary care doctors and residents of other countries. However, satisfaction with the current nutritional education was moderate, and the amount of nutritional education provided during training was perceived as insufficient. This highlights the necessity for enhanced nutrition-related education in FM training in Korea. Additionally, confidence levels in nutrition-related topics varied according to the topic. Consequently, future efforts should focus on providing education in nutrition topics where the residents feel a lack of self-perceived competency, along with the need to evaluate the objective competency in nutrition knowledge and counseling.
Table 1.
Self-perceived competency levels on 29 nutrition-related subjects of Korean family medicine residents
Table 2.
Baseline characteristics of participants (n=68)
Table 3.
Nutritional topics requiring further education during training as a family medicine resident
REFERENCES
1. World Health Organization. Diet, nutrition and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation. Geneva: World Health Organization; 2003.
2. Yu E, Malik VS, Hu FB. Cardiovascular disease prevention by diet modification: JACC Health Promotion Series. J Am Coll Cardiol 2018;72:914-26.


3. Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr 2008;27:5-15.


4. Schuetz P, Fehr R, Baechli V, Geiser M, Deiss M, Gomes F, et al. Individualised nutritional support in medical inpatients at nutritional risk: a randomised clinical trial. Lancet 2019;393:2312-21.


5. Muscaritoli M, Krznaric Z, Singer P, Barazzoni R, Cederholm T, Golay A, et al. Effectiveness and efficacy of nutritional therapy: a systematic review following Cochrane methodology. Clin Nutr 2017;36:939-57.


6. Devries S, Willett W, Bonow RO. Nutrition education in medical school, residency training, and practice. JAMA 2019;321:1351-2.


7. International Food Information Council. 2018 Food & Health Survey [Internet]. Washington (DC): International Food Information Council; 2018 [cited 2023 Oct 5]. Available from: https://www.foodinsight.org/2018-FHS-Report-FINAL.pdf
8. Ball L, Hughes R, Desbrow B, Leveritt M. Patients’ perceptions of nutrition care provided by general practitioners: focus on type 2 diabetes. Fam Pract 2012;29:719-25.


9. Ball L, Johnson C, Desbrow B, Leveritt M. General practitioners can offer effective nutrition care to patients with lifestyle-related chronic disease. J Prim Health Care 2013;5:59-69.


10. American Academy of Family Physicians. Role definition of family medicine [Internet]. Leawood (KS): American Academy of Family Physicians; c2023 [cited 2023 Oct 5]. Available from: https://www.aafp.org/about/policies/all/role-definition.html
11. Crowley J, Ball L, Hiddink GJ. Nutrition in medical education: a systematic review. Lancet Planet Health 2019;3:e379-89.


12. Owens S, O’Carroll A, Allman J, Badoi A. Attitudes on the role of nutrition in GP training. Ir Med J 2022;115:517.

13. Cassidy-Vu L, Kirk J. Assessing the need for a structured nutrition curriculum in a primary care residency program. J Am Coll Nutr 2020;39:243-8.


14. Deen D, Spencer E, Kolasa K. Nutrition education in family practice residency programs. Fam Med 2003;35:105-11.

15. Daley BJ, Cherry-Bukowiec J, Van Way CW 3rd, Collier B, Gramlich L, McMahon MM, et al. Current status of nutrition training in graduate medical education from a survey of residency program directors: a formal nutrition education course is necessary. JPEN J Parenter Enteral Nutr 2016;40:95-9.

16. Wynn K, Trudeau JD, Taunton K, Gowans M, Scott I. Nutrition in primary care: current practices, attitudes, and barriers. Can Fam Physician 2010;56:e109-16.


17. Dumic A, Miskulin I, Pavlovic N, Cacic Kenjeric D, Orkic Z, Miskulin M. Attitudes toward nutrition care among general practitioners in Croatia. J Clin Med 2018;7:60.



18. Crowley J, O’Connell S, Kavka A, Ball L, Nowson CA. Australian general practitioners’ views regarding providing nutrition care: results of a national survey. Public Health 2016;140:7-13.


19. Crowley J, Ball L, Han DY, McGill AT, Arroll B, Leveritt M, et al. Doctors’ attitudes and confidence towards providing nutrition care in practice: comparison of New Zealand medical students, general practice registrars and general practitioners. J Prim Health Care 2015;7:244-50.


20. Nowson CA, O’Connell SL. Nutrition knowledge, attitudes, and confidence of Australian general practice registrars. J Biomed Educ 2015;2015:219198.


21. Vetter ML, Herring SJ, Sood M, Shah NR, Kalet AL. What do resident physicians know about nutrition?: an evaluation of attitudes, self-perceived proficiency and knowledge. J Am Coll Nutr 2008;27:287-98.



22. Han SL, Auer R, Cornuz J, Marques-Vidal P. Clinical nutrition in primary care: an evaluation of resident physicians’ attitudes and self-perceived proficiency. Clin Nutr ESPEN 2016;15:69-74.


23. Al-Gassimi O, Shah HB, Sendi R, Ezmeirlly HA, Ball L, Bakarman MA. Nutrition competence of primary care physicians in Saudi Arabia: a cross-sectional study. BMJ Open 2020;10:e033443.



24. American Academy of Family Physicians. Recommended curriculum guidelines for family medicine residents [Internet]. Leawood (KS): American Academy of Family Physicians; c2023 [cited 2023 Oct 5]. Available from: https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint275_Nutrition.pdf
25. Curriculum Committee of the Nutrition Academic Award Program. Nutrition curriculum guide for training physicians: practice behavior skills and attitudes across the curriculum [Internet]. Bethesda (MD): National Heart, Lung, and Blood Institute; 2002 [cited 2023 Oct 5]. Available from: https://www.nhlbi.nih.gov/sites/default/files/media/docs/NAA%20Nutrition%20Curriculum%20Guide.pdf